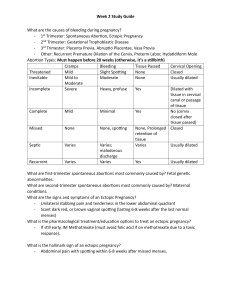
NURSING CARE of the CLIENT who is having an Abortion

Nursing Care:
Counseling about the procedures and alternatives
Provide nonjudgmental care
Allow the client to express her feelings
Preparation for the procedures:
Surgery-D&C or hysterotomy (rarely used)
Medications:
“Morning –after pill” –RU-482
Oxytocin
Prostaglandins-ProstinE2
Misoprotol (Cytotec)
Post –procedure care
Administer RhoGam if the client is Rh-negative
Discharge Instructions
INCOMPETENT CERVIX is where there is painless effacement and dilation of the cervical os that is not associated with contractions
It often occurs in the second trimester
Risk Factor:
Congenital uterine anomalies
Diethylstilbestrol (DES) exposure
Cervical operations
Cervical Trauma
Cervical Inflammation
Clinical manifestations:
Lower abdominal pain
Urinary frequency in the second trimester
Effacement and Dilation of the cervix
Protrusion of membranes through the cervix
Rupture of the membranes in second trimester
Treatment:
Bedrest- Position client so there is pressure off cervix Initially the Trendelenburg position may be used until after surgery
Serial cervical ultrasound assessment
No vaginal exams
Administer tocolytic agents
Surgical intervention- Cerclage is a band of nonabsorbable suture placed around the cervix.
Monitor for uterine contractions, fetal well being, and vital signs
Discharge planning:
Teach the client the clinical manifestations of preterm labor , rupture of membranes, and infection. And to report them to health care provider immediately.
Teach the client to return(to hospital) if uterine contraction begin , because the suture will need to be removed to prevent damage to cervix and allow birth
Keep follow up visits with the health care provider
Do Fetal Movement Counts
PLACENTA PREVIA is the improper implantation of the placenta in the lower uterine segment.
It is classified according to the degree to which the placenta covers the cervical os.:
Low-laying
Marginal
Partial
Complete or Total
Risk factors:
Endometrial scarring
Impede Endometrial vasculation related to:
Hypertension
Diabetes mellitus
Uterine tumor
Drug abuse
Smoking
Increase placenta mass
Closely spaced pregnancies
Multiple gestation
Multiparity
Clinical Manifestations:
Episodic painless vaginal bleeding after 20 weeks gestation
Bright Red Bleeding without uterine contractions
Ultrasound:
Reveals the malpositioned placenta
Complications of placenta previa:
Preterm delivery
Hypovolemia
Altered tissue perfusion
Deterioration in fetal status
NURSING CARE:
Perform a complete assessment on any pregnant client that presents with painless bright red vaginal bleeding except:
NO VAGINAL EXAMS
Insert large bore catheter(18 or greater) and maintain IV infusion
Monitor:
Vital signs
Continuous Fetal monitoring
I&O-pad count/weight them
Notify:
Physician, charge nurse, ICN, and anesthesia personnel
Nurse Care:
Obtain laboratory specimens:
CBC, Type & Rh, Type & Crossmatch
Be prepared to deliver client:
Vaginally for the low-lying placenta-have Double set up in the
Delivery room
Cesarean section for partial and complete placenta previahave Hysterectomy tray in the delivery room
Provide emotional support
Strict Bedrest- Position client so pressure is not on the placenta
If client is stable and has diet order make sure it is well balance
Prenatal vitamins and iron will be continue
ABRUPTIO PLACENTA is a premature separation, either partial or total of a normally implanted placenta from the decidual lining of the uterus after 20 weeks’ gestation.
Classifications of Abruptio Placenta:
Types: See next slide
Marginal-A
Central/Concealed/Covert-B
Complete-C
Degrees of placental separation:
Grades-0-3
RISK FACTORS:
Preeclampsia
Eclampsia
Chronic Hypertension
Multiparty
Abdominal Trauma
Uterine Anomalies
Smoking
Cocaine Abuse
Premature Rupture Of Membranes-PROM
Complications of Abruptio Placenta:
Risk of depleting clotting factors
DIC
Hypovolemia
Multiorgan failure
Maternal Death
Uterine Placenta insuffiency
Fetal Hypoxia
Fetal Death
Clinical manifestations:
Sudden Dark Red Vaginal Bleeding
Unremitting pain
Firm-to boardlike uterine
Shock greater than blood loss
Ultrasound will show abruption
EFM:
Uterine irritability
Nonreassuring Fetal Heart pattern- Loss of variability and late decelerations
NURSING CARE:
Assess and Monitor:
Amount of Vaginal Bleeding
Vital Signs
I&O
Measure abdominal girth
Uterine characteristics and activity
EFM-Continuously
For development of coagulation problems
Review lab values:
CBC, Coagulation studies, PT,PTT
Nursing Care:
Insert large IV Catheter(18-gauge or bigger) and maintain IV infusion
Provide O@ at 8-12L/min
Anticipate Transfusion Therapy:
RBC’s
FFP
PLT’s
Crypopreciate
Albumin
Nursing Care:
Anticipate Expedited Delivery:
Vaginally
Cesarean section
Have Hysterectomy Tray in room
Provide emotional support
Instruct client and family on disease process and procedures and possible surgery
Contact-Physician, Charge nurse, Anesthesia personnel, ICN unit
DISSEMINATED INTRAVASCULAR COAGULATION
(DIC) is a complex coagulopathy condition which occurs secondary to another underlying disease process
Risk Factor:
Preeclampsia/Eclampsia
Sepsis
Abruptio Placenta
Prolonged IUFD
Excessive Blood
Uterine inversion or rupture
Amniotic Fluid embolism (AFE)
Complications:
Hypovolemia
Alt. Tissue Perfusion
Multiorgan failure
Maternal death
Fetal death
Clinical Manifestations:
Shocklike state
Overwhelming and diffuse hemorrhage:
Petechia, ecchymosis, hematomas
Oozing of blood from puncture sites, IV sites, and /or surgery incisions. Bleeding gums.
Blood in urine
Laboratory valves:
Decreased Hg and Hct
Prolonged PTT and PT
Decreased fibrinogen
Decrease PLT’s
D-Dimer
NURSING CARE:
Care for this client is for the critically ill client.
Identify Risk factors predisposing to DIC. Early detection is extremely important
Maintain IV site- Central line maybe placed.
Anticipated Transfusion therapy:
Fresh Whole Blood
Fresh Frozen plasma
Cryoprecipate
Monitor VS, I&O, perfusion status*,bleeding, cardiopulmonary status
Nursing Care:
Educate the client and family concerning disease process, procedures.
Provide support to the client and family.
No Heparin is given to the client who has DIC and who is pregnant or has been delivered
HYPEREMESIS GRAVIDARUM is a disorder with intractable vomiting associated with pregnancy with significant electrolyte imbalance and fluid deficit and possible starvation.
Etiology is unknown/PREGNANCY
Risk Factors:
High levels of hCG
Gestational Trophoblastic Disease
Multigestation
Psychopathologic and emotional factors
Stress
Other pathophysiology