Patient Surge Triage Tabletop - Missouri Hospital Association
advertisement

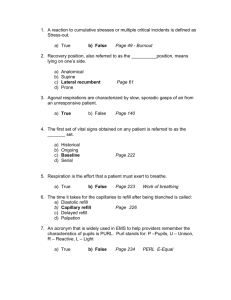
This exercise program was developed and made available by the Missouri Hospital Association through funds from the ASPR Hospital Preparedness Program CFDA 93.889, through a subcontract from the Missouri Department of Health and Senior Services for the purposes of individual hospital preparedness and exercise. Sources used in the development of these materials are noted in the Notes Section except where general knowledge. Patient Surge Tabletop Exercise Focus: Patient Triage Exercise Purpose and Goal The goal and purpose of this exercise is to orient hospital triage staff to the process of disaster patient triage and to triage simulated patients. This exercise will utilize the START triage system to triage simulated patients. This system can be used to sort simulated patients, according to their injuries and level of acuity, into categories allowing the most critical patients to receive treatment more quickly than patients who may be able to have delayed treatment. Exercise Objectives Provide an orientation to Surge Capacity and the Care Continuum Discuss the need for triage Review various decision tools for triage Discuss the activation process for our Mass Casualty or Patient Surge Plan Discuss the key components for the response Develop response objectives for a mass casualty event Triage simulated patients using the START triage system (or substitute your triage methodology) Surge Capacity and the Care Continuum Hospitals must prepare for surges of patients due to a variety of causes: natural disasters, man-made events causing injury and/or illness, and disease outbreaks. Numbers of patient surge capabilities will vary, hospitals should plan for a 20% surge. Response will span the continuum from Conventional, Contingency, to Crisis care Care Continuum Conventional Capacity: The spaces, stuff, and supplies used are consistent with daily practices within the institution. These spaces and practices are used during a major mass casualty incident that triggers activation of the facility emergency operations plan. Contingency Capacity: The spaces, staff, and supplies used are not consistent with daily practices but provide care that is functionally equivalent to usual patient care. These spaces or practices may be used temporarily during a major mass casualty incident or on a more sustained basis during a disaster (when the demands of the incident exceed community resources.) Source: Hick et al., 2009. Care Continuum Crisis Capacity: Adaptive spaces, staff, and supplies are not consistent with usual standards of care, but provide sufficiency of care in the context of a disaster (i.e., provide the best possible care to patients given the circumstances and resources available). Crisis capacity activation constitutes a significant adjustment to standards of care. Source: Hick et al., 2009. What is disaster triage? Triage is used to classify patients for care based on the severity of their illness or injury in context of the resources available with the goal of doing the most good for the greatest number of people. When do we go to disaster triage? When a large number of patients present that overwhelm normal resources for treatment. Triage helps to ensure best use of the limited resources. The triage process should be ongoing; in the field, when patients present, when arriving at their treatment area, after initial treatment is given….. Types of triage Primary triage – takes place early in an incident either in the field by EMS or when patients present to the hospital. Secondary triage – performed after additional assessments and initial interventions Tertiary triage – performed after or during the provision of definitive diagnostics and medical care Decision Tools for the Triage Process Decision tools provide: Common criteria that can be applied in a relatively uniform fashion by multiple providers Objective indicators by which to determine prognosis Improved consistency of decisions across multiple providers and facilities Prognostic value that is evidence based A degree of protection from legal action if the provider is following published guidelines or facility plans in good faith Type of triage decision tools Limited resource allocation algorithms (i.e. ventilators) SOFA (Sequential Organ Failure Assessment) ESI (Emergency Severity Index) START (Simple Triage and Rapid Transport) JumpSTART – Pediatric version of START SOFA Emergency Severity Index Decision Criteria Immediate life saving intervention required Mental status Level of pain Vitals; HR, RR, O2 sat Number of resources needed Why tag at the hospital? Re-triage patients who arrive via EMS as status may have changed. Triage disaster patients at the Hospital Triage Area as soon as possible after their arrival. Triage tag communicates priority of treatment. Easily identifiable as to category and therefore hospital treatment area destination. Avoids the need to repeatedly re-triage the patient. (periodic reassessment is still needed) START Triage criteria Walk? Breath? Respiratory Rate? Perfusion? Capillary refill or radial pulse? Mental status? JumpSTART Utilizes same assessment criteria as START. Algorithm adjusted for pediatric patients. START triage tag training video http://www.triagetags.com/index.php?route=inf ormation/information&information_id=9 Types of triage tags DMS others Triage Tag Common Elements Color based categories: Red – need immediate care Yellow – delayed Green – minor, walking wounded Black – deceased or not expected to survive May have bar codes May have place for patient information Other times to triage Evacuation – triage patients for order to evacuate the facility Based on type of event: no notice vs. advanced warning Time available to evacuate Resources available to evacuate Reverse triage may be used: evacuate the largest number of patients in the shortest amount of time – Greens and those in immediate danger 1st – Yellows – require additional resources to move – Reds – critical care and/or require the most resources to move Other times to triage Large influx of patients expected Triage existing ED and inpatients to determine who can be discharged or released to a lower level of care There is a shortage of a critical resource. Triage criteria must be developed for allocation of that resource. Critical Plan Components Alerting – receive notice of a significant event from local and/or regional partners Notification – internal responders as well as relevant external partners Command – HICS, scaled, flexible. Incident action planning. Control – departmental specific response Communications – ability to communicate between critical areas and responders Critical Plan Components Coordination – within the hospital as well as to external local and regional partners Public Information - internally to patients, staff, families, and visitors. External to the public and news media. Operations – triage and clinical teams. Develops the strategy and tactics to meet the incident objectives. Expansion of clinical care areas, patient triage and treatment. Critical Plan Components Logistics – acquisition of resources to support the operation Planning – gathers incident related data, analyses, and forecasts. Conducts planning meetings and prepares the Incident Action Plan. Material, personnel, patient, and bed tracking. Patient Surge (Mass Casualty) Plan Review Review the key components of your plan here Triage Exercise Exercise objectives Discuss the need for activation of the hospital patient surge plan Discuss the need for establishment of triage and treatment areas Utilize patient cards to triage patients for transport to treatment areas using START triage system Scenario Part 1 Monday evening, 9pm Your ED is at normal staffing, supply, and patient levels You receive a call in the ED from Public Safety Dispatch that there has been a transportation accident (insert most likely scenario, bus, train, plane, etc. for your area) in your community EMS and Fire are enroute. They anticipate at least 30 (can modify to stress your facility) casualties from initial reports. Discussion Break Would this cause an activation of your Emergency Plan? Who would you contact? What level of activation? What are the critical components (priorities) of the response to this situation? What are your incident objectives at this time? Who is in charge? Scenario Part 2 An update is received by Incident Command on the scene. There are an estimated 100 casualties with 40 estimated as being critical. The other hospital in the community can accept 20 of the non-critical casualties as they are currently under construction in their ED. Modify this slide to stress your facility and cause an adequate level of required response. Discussion Break Does this new information cause any of your previous decisions to change? Additional notifications? Level of activation? Areas to set up/activate? (Command Center, Triage Area, Treatment Areas, Labor Pool, etc.) Where are they located? Who is the hospital Incident Commander? What hospital incident command system (HICS) positions would you activate? Have your objectives changed? Scenario Part 3 Your first patient arrives by helicopter with serious injuries. A bus load of green patients arrive from the scene. They have triage tags on them from EMS. A passenger van arrives with 10 people they have brought in from the scene. Triage Exercise You are working the Triage Area. Triage the paper patients with the information listed on their card. Tear off the appropriate portion of the triage tag and attach the tag prior to movement of the patient to the appropriate Treatment Area. What have we learned? What went well? What did not go well? Any gaps in our knowledge, skills, resources, or planning that need to be enhanced to be more prepared for this type of a situation in the future? Questions? Thank you for your participation! Please complete your Participant Evaluation Form prior to leaving References IOM (Institute of Medicine). 2012. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington DC: The National Academic Press HICS Guidebook, 2014: California Medical Services Authority.