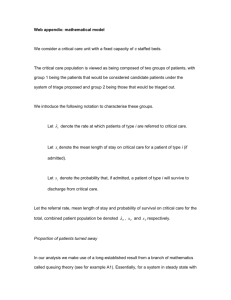
Eliminating Triage
advertisement
Eliminating Triage Christopher DeLuca, MD, FACEP Vice President, Performance Improvement Emergency Resource Management, Inc. Clinical Assistant Professor, Emergency Medicine University of Pittsburgh, School of Medicine Definition of Triage The allocation of treatment to battle and disaster victims according to a system of priorities designed to maximize the number of survivors. Triage originated in military medicine, when limited resources faced many wounded soldiers. Baron Larrey Definition of Triage Division of patients for priority of care into three categories: 1) Those who will not survive even with treatment 2) Those who will survive without treatment 3) Those whose survival depends on treatment. When triage is applied correctly, the treatment of patients requiring it is not delayed by useless or unnecessary treatment of those in the other groups. Evolution of Triage Soldiers triaged as mortally wounded were left on the battle field to die. Florence Nightingale would search the battlefields at night to care for these soldiers. Larrey altered the established pattern by going forward during battles to pick up the wounded who could survive with potentially lifesaving surgery. Florence Nightingale Evolution of Triage Triage 1) Those who will not survive even with treatment 2) Those who will survive without treatment 3) Those whose survival depends on treatment Delay-age 1) 2) 3) 4) 5) 6) 7) 8) 9) Chief complaint Vital signs History of present illness Past medical history Current medications Allergies Past surgical history Mandated screening questions Physical exam Who cares? CMS Quality Measure OP-20: Door to Diagnostic Evaluation by a Qualified Medical Provider Definition: Median Time from ED Arrival to Provider Contact for Emergency Department Patients Improvement noted as a decrease in the median value Solutions Provider in Triage Direct-to-room Process Direct-to-room Process If we could do it with ambulances, why couldn’t we do it with everyone? Lean principles utilized: Waiting (decrease door to room/provider) Defects (communication between intake staff and nursing staff in department) Over production (how do we distribute the patients evenly?) Extra processing (how many times does the patient need to give a history?) Unused employee creativity (committee formed to develop the process) Direct-to-room Process - Guide 1) Data elements required (rooms available): - Name and DOB - Chief complaint and Weight 2) Scripted communication plan developed to ensure nurses and techs in treatment spaces aware of new patients 3) ED tracking board developed to alert physicians of new patients 4) Registration and initial nursing assessment occurs at the bedside 5) ESI when beds are full Direct-to-room Process - Guide Culture changes required: 1) Triage is no longer a full initial nursing assessment. 2) Nursing assessment usually not available at time of physician assessment. Usually done simultaneously. 3) Quick registration by clinical staff, full registration by registration staff performed at bedside. Direct-to-room Process - Guide Advantages: 1) 10 triage nurses vs 1 2) 5 providers in triage vs 1 Disadvantages: 1) Need to shift nursing resources 2) Information not immediately available for physicians Direct-to-room Process - Results Median Door to Room Time St. Clair Hospital 70 60 50 40 30 20 10 0 58 8 1 2 1 2 1 2 2 Direct-to-room Process - Results Median Door to Provider St Clair Hospital 90 80 70 60 50 40 30 20 10 0 82 27 21 13 14 Questions? delucac@upmc.edu