Active Efflux in Clinically-Important Gram-Negative Bacteria
advertisement

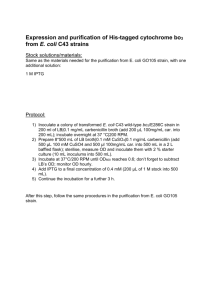
Role of the Efflux Pumps in Antimicrobial Resistance in E. coli Patrick Plésiat Bacteriology Department Teaching Hospital Besançon, France ANTIBIOTIC TARGET Bacterial targets for antibiotics Chromosome Cell wall Ribosomes Cytoplasmic membrane Main resistance mechanisms to drugs Inactivation Modification ANTIBIOTIC Efflux Impermeability Protection TARGET Substitution Amplification Reduced affinity - mutations - recombinaisons - enzymatic modification Gram-negative species with known efflux systems Escherichia coli Salmonella Typhimurium Shigella dysenteriae Klebsiella pneumoniae Enterobacter aerogenes Serratia marcescens Proteus vulgaris Citrobacter freundii... Bacteroides fragilis... Pseudomonas aeruginosa Pseudomonas putida Burkholderia cepacia Burkholderia pseudomallei Stenotrophomonas maltophilia Alcaligenes eutrophus... Haemophilus influenzae Campylobacter jejuni Helicobacter pylori Vibrio parahaemolyticus Vibrio cholerae Neisseria gonorrhoeae... Efflux mechanisms: practical implications Do efflux systems produce clinically relevant levels of resistance ? Does the expression of drug transporters somewhat impair the virulence of bacterial pathogens ? What is the prevalence of efflux systems relative to other resistance mechanisms among the clinical isolates ? How to recognize efflux mutants in laboratory practice ? What recommendations can be made to the physician for the treatment of patients infected with mdr strains ? Intracellular accumulation Drug accumulation experiments S ATP glucose R CCCP Time Structure of bacterial efflux systems One component systems – Mostly in Gram positive species (except Tet...) – A single transporter protein in the cytoplasmic membrane – Determines the substrate specificity and resistance Three component (tripartite) systems – Exclusively in Gram negative species (GNB) A transporter protein A periplasmic adaptor lipoprotein A outer membrane channel protein Energy sources Antiporters – PMF transporters (proton motive force) – Na+-antibiotic antiporters ABC transporters – ATP binding cassette pumps – Hydrolysis of ATP into ADP + Pi – Mostly in Gram positive species PMF transporters Major Facilitator Superfamily (MFS) – Drug efflux 12 TMS transporters 14 TMS transporters – Active uptake/export Small Multidrug Resistance Family (SMR) 4 TMS transporters Resistance/Nodulation Cell Division Family (RND) sugars... amino acids, secondary metabolites... 12 TMS transporters Multi Antimicrobial Extrusion Family (MATE) 12 TMS transporters Structure of drug efflux systems antibiotic antibiotic H+ Na+ H+ ATP MFS, SMR MATE ADP ABC RND, MFS, ABC Fernandez-Recio J. et al. FEBS 2004, 578: 5-9 Murakami S. et al. Nature 2002, 419: 587 Murakami S. et al. Curr Opinion Struct. Biol. 2003, 13: 443 Murakami S. et al. Curr Opinion Struct. Biol. 2003, 13: 443 Efflux systems in E. coli Chromosomally encoded pumps – 37 putative drug transporters: 19 MFS, 3 SMR, 7 RND, 7 ABC, 1 MATE – 20 pumps are able to transport toxic/antibiotic molecules – 15-17 pumps may provide with some resistance to antibiotics when overproduced from cloned genes (Nishino K et al. J. Bacteriol. 2001) – Upregulation of a single pump may result in increased drug efflux Acquisition of exogenous pump encoding genes – Genes carried by mobile elements (plasmids, transposons, integrons) Efflux pumps coded by mobile genetic elements Species System E. coli E. coli E. coli E. coli TetA/B/E CmlA Flo OqxAB-TolC Family MFS MFS MFS RND Substrates Tc, Min Cmp Cmp, Flo Olaquindox, Cmp Tc: tetracycline; Min: minocycline; Cmp: chloramphenicol; Flo: florfenicol Efflux pumps of MFS, MATE, SMR, or ABC family Species System E. coli E. coli E. coli E. coli E. coli E. coli E. coli E. coli E. coli E. coli E. coli EmrAB-TolC Bcr MdfA MdtG MdtH MdtL MdtM NorE EmrE MdtJK MacAB-TolC Family MFS MFS MFS MFS MFS MFS MFS MATE SMR SMR ABC Substrates Genes Nal Tc, Km, Fos Tc, Rif, Cmp, Ery, Neo, Fq... Fos Fq Cmp Cmp, Fq Cmp, Fq, Fos, Tmp Tc Nal, Fos Ery C C C C C C C C C C C Nal: nalidixic acid; Tc: tetracycline + glycylcyclines; Km: kanamycin; Fos: fosfomycin; Rif: rifampicin; Cmp: chloramphenicol; Ery: erythromycin; Neo: neomycin; Fq: fluoroquinolones; Tmp: trimethoprim Efflux pumps of the RND family Bacteria System Substrates E. coli AcrAB-TolC1 Fq, ß-lactams3, Tc, Cmp, Nov, Ery, Fus, Rif… E. coli AcrEF-TolC2 Fq, ß-lactams3, Tc, Cmp, Nov, Ery, Fus, Rif… E. coli AcrD2-AcrA-TolC AGs, Ery, PolyB E. coli CusAB-?2 Fos E. coli MdtABC-TolC2 Fq E. coli MdtEF-TolC2 Ery P. aeruginosa MexAB-OprM1 Fq, ß-lactams1, Tc, Cmp, Nov, Ery, Fus, Tm... P. aeruginosa MexCD-OprJ2 Fq, 3rd GC, Tc, Cmp, Ery, Tmp P. aeruginosa MexEF-OprN2 Fq, Cmp, Tmp P. aeruginosa MexXY2-OprM Fq, AGs, 3rdGC, Ery, Tc N. gonorrhoeae MtrCDE1 Tc, Cmp, ß-lactams1, Ery, Fus, Rif... Fq: (fluoro)quinolones; Tc: tetracycline; Cmp: chloramphenicol; Nov: novobiocin; Ery: erythromycin; Fus: fusidic acid; Rif: rifampicin; AGs: aminoglycosides; PolyB: polymyxin B; Tmp: trimethoprim; Sulf: sulfamethoxazole; 3rdGC: cefepime, cefpirome. expressed constitutively in wild type cells, 2 inducible expression, 3 except imipenem. 1 Induction of acrAB-tolC expression tetracycline chloramphenicol salicylate-acetylsalicylate benzoate stress... MarROAB SoxSR Rob Porin OmpF TolC AcrAB EmrAB Other proteins Mar regulon oxidative stress bile salts tetracycliner chloramphenicolr quinolonesr erythromycinr solvants, pine oil... Overexpression of acrAB and mtrCDE operons _ MarA (MppA) MarR _ + - SoxS acrA SoxR acrB acrR MtrA + - mtrC mtrD mtrE mtrR mutations mdr * * * * * * * * * * * Webber M. et al. Antimicrob. Agents Chemother. 2001, 45: 1550 Systems MtrCDE and FarAB in N. gonorrhoeae wild type CDE++ CDE- FarAB- Penicillin G 0.008 0.032 0.008 nd Erythromycin 0.25 1-2 0.06 0.25 Tetracycline 0.25 0.5 nd nd Rifampicin 0.06 0.25 0.015 nd Linoleic acid 1600 nd 25 - 50 50 Palmitic acid 100 nd 12.5 12.5 Antibiotics System AcrAB-TolC in E. coli Antibiotics wild type AcrAB++ AcrAB- Nalidixic acid 4-6 8.5 - 32 0.6 Norfloxacin 0.025 - 0.1 0.3 - 1.25 nd Ofloxacin 0.06 - 0.07 0.25 - 0.3 nd Ciprofloxacin 0.02 0.15 nd Ampicillin 2-4 5-6 0.6 - 2 128 - 256 > 512 <2-8 Tetracycline 1.25 - 3 5 - 16 0.25 - 0.3 Chloramphenicol 4 - 7.5 10 - 28 0.6 Erythromycin System MexAB-OprM in P. aeruginosa Antibiotics wild type MexAB++ MexAB- Norfloxacin 0.25 - 1 2-4 0.05 - 0.25 Ofloxacin 0.4 - 1 1.6 - 8 0.025 - 0.05 Ciprofloxacin 0.03 - 0.25 0.4 - 1.6 0.012 - 0.03 Carbenicillin 12.5 - 64 50 - 256 0.4 - 1 Aztreonam 1.6 - 4 12.5 - 32 0.1 - 0.2 Ceftazidime 0.4 - 2 1.6 - 8 0.2 - 0.4 Cefepime 0.8 - 2 3-4 0.1 - 0.5 Meropenem 0.2 - 0.5 0.8 - 2 0.1 - 0.2 Tetracycline 6.25 - 16 25 - 64 0.2 - 1.2 Chloramphenicol 12.5 - 32 100 - 512 0.8 - 2 Interplays between resistance mechanisms in GNB Outer membrane permeability Other mechanisms Active efflux Efflux/target double mutants of E. coli Genotype/Phenotype Oflo Cipro wild type AG100 0.03 ≤0.015 AcrAB++ 0.125 0.06 gyrA (Asp87->Gly) 0.25 0.25 gyrA (Asp87->Gly; Ser83->Leu) 4 2 gyrA (Asp87->Gly), AcrAB++ 8 4 0.06 0.03 gyrA (Asp87->Gly), AcrAB- Oethinger et al. Antimicrob. Agents Chemother. 2000, 44: 10-13 Therapeutic implications of efflux systems Resistance levels conferred by intrinsic pumps – Low to moderate drug resistance (MIC x 2 - 16) – Clinical significance Lack of clinical data ! Poor response to treatment when the concentrations of antibiotics are low at the infection site (insufficient dosage, inappropriate drug, abcess...) Increased emergence of target mutants ? Emergence of efflux mutants under treatment – Cross resistance to structurally unrelated molecules – Role of fluoroquinolones PK/PD Monte Carlo MI C (mg/L) Treatment Drug Ciproflox. total daily dosage (mg) unitary dose interval (hours) 1200 8 1600 2400 Levoflox. 500 1000 6 8 24 12 Target Attainm ent Rate (%) Cmax/MIC > 10 AUC/MIC > 125 0.12 66 87 0.25 6 7 0.12 66 90 0.25 5 12 0.12 98 100 0.25 60 85 0.5 4.2 3.7 0.5 70 40 1 4 3 0.5 72 72 1 4 5 Dupont P. et al. J. Antimicrob. Chemother. 2005 Efflux mutants, are they virulent ? Clinical experience – Many examples of mdr isolates recovered from clinical specimens (blood, urine, sputums…) Other considerations – marA disruption mutants of S. Typhimurium remain fully virulent in a murine BALB/c infection model (Sulavik, J. Bacteriol. 1997, 179: 1857) – First step fluoroquinolone resistant mutants with mutations in gyrA, gyrB or marOR do not display significant loss of fitness (in vitro competition experiments, experimental urinary tract infection in mouse) (Komp Lindgren P., AAC 2005, 49: 2343) – Role of secondary mutations ? How to characterize efflux mechanisms Plasmid or transposon encoded efflux systems – Multiresistance phenotype – Detection of efflux gene(s): PCR, nucleic probes Upregulation of intrinsic efflux systems – Protein levels Western blotting of membrane extracts with specific antibodies – mRNA levels Northern blot, MacroArray, MicroArray Real Time RT-PCR (Light Cycler, Taq Man, I Cycler…) – Intracellular accumulation of antibiotics [3H] ou [14C] radiolabeled or fluorescent compounds (BET, acriflavine…) – Sequencing of regulatory genes Efflux inhibitors Phenyl-Arginyl ß N-naphtylamide