clinical-biochmeistry-and-liver
advertisement

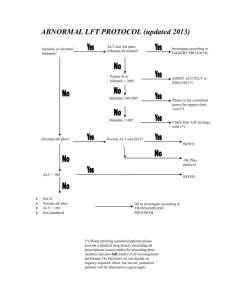
Recommended Reading Lecture Notes in Clinical Biochemistry 7th Edition G Beckett, S Walker, P Rae, P Ashby (Blackwell publishing) Clinical Chemistry 6th Edition W J Marshall, S K Bangert (Pubslished by Mosby) An illustrated Colour text - Clinical Biochmeistry 3rd edition Alan Gaw et al (Churchill Livingston) Handbook of Clinical biochmeistry 1st Edition R Swaminathan (Oxford University Press) Clinical Chemistry in diagnosis and treatment Philip Mayne (Edward Arnold) A Guide to Diagnostic Clinical Chemistry 3rd Edition Walmsely & White (Blackwell) Clinical Biochemistry of Liver Disease Dr Vivion Crowley Consultant Chemical Pathologist St James’s Hospital Illustrative case History 75 yr old female presented to her GP C/O dyspepsia and “back “ pain Background hx: •Breast Ca – Rx with mastectomy, Tamoxifen •Variegate Porphyria •Type 2 Diabetes mellitus •Subclinical Hypothyroidism GP requested Liver Function Tests (Liver Profile) Albumin 43 (34-48) g/L Total Bilirubin 7 (0 – 21) umol/L Alkaline Phosphatase 67 (35 -104) IU/L GGT 93 (5 – 36) IU/L Alanaine transaminase (ALT) 40 (6 – 31) IU/L In view of abnormal LFTs the GP ordered further investigations •Anti Smooth Muscle abs - neg •Anti Mitochondrial abs - neg •Alpha-1 Antitrypsin 1.5 (0.9 – 2.0) g/L •Caeuroloplasmin 26.2 (20 – 60) mg/dl •Transferrrin Saturation 34% (15 – 45) % •PT 14.8 (11.5 – 15.0) s •APTT 30.4 s (25 – 35) s GP requested imaging studies in view of negative blood tests Ultrasound of abdomen and pelvis Liver -Diffuse inhomogenous somewhat echogenic texture -No focal lesion -Bile ducts not dilated CT scan of abdomen Liver -Normal size -Subcapsular surface of the liver has a nodular outline -Liver texture has a diffuse slightly coarse appearance Appearances consistent with Cirrhosis Learning Point • The only indicator for the presence of underlying cirrhosis in this patient were her mildly abnormal LFTs What are the functions of the liver? •Key role in intermediary metabolism e.g. gluconeogenesis, glycolysis, ketogeneis, lipid synthesis •Protein synthesis – including many plasma proteins and blood clotting factors •Bile secretion and role in digestion •Primary site of xenobiotic detoxification -drug and toxin metabolism •Ureagenesis - ? Role in acid-base balance What are Liver Function Tests (LFTs) Total Bilirubin -Conjugated vs. Unconjugated -Anion transport Alkaline Phosphatase (ALP) -Reference range varies with age – higher in childhood and adolescence -Isoenzymes e.g. bone, liver, intestine, malignancy -Bile flow Gamma-glutamyl transferase (GGT) -Sensitive indicator of liver disorder -Cholestasis -Induced by many drugs and toxins e.g. C2H5OH, pheytoin, barbiturates, ? statins Transaminases -Alanine aminotransferase (ALT) -Aspartate aminotransferease (AST) -ALT is more liver specific -AST is also found in cardiac and skeletal muscle -Hepatocellular integrity Albumin - Plasma transport protein -Assesses Protein synthesis in liver Prothrombin time -Extrinsic pathway of coagulation -Reflects protein synthetic function What role do LFTs in clinical management ? Detecting the presence of liver disease Indicating the broad diagnostic category of the liver disease Monitoring treatment Specialised Liver-related tests Viral Hepatitis Screen – A, B, C etc. Autoimmune Heaptitis screen – AMA, ASMA, Serum protein electrophoresis α1- antitrypsin α fetoprotein (AFP) Transferrin Saturation/Ferritin/HFE Genotyping Caeruloplasmin, Plasma/Urine Copper Ultrasound scan, CT, MRI Biopsy Clinical History C2H5OH Hx Family Hx – Haemochromatosis, Wilson Disease, Drug Hx – What medication is the patient taking? Travel Hx – Recent travel, Blood transfusions Bilirubin production and metabolism UDP Glucoronosyl transferase Hyperbilirubinaemia •Jaundice evident with Bilirubin levels 35-70μmol/L •Normally 95% of plasma bilirubin is unconjugated Unconjugated - prehepatic *(No bilirubinuria) Conjugated – Hepatic/posthepatic (Bilirubinuria) •Haemolyis •Resolving haematoma •Gilbert’s Syndrome •Crigler-Najjar syndrome •Hepatocellular diseases •Cholestatic diseases •Dubin-Johnson** •Rotor’s syndrome** *Except in Nephrotic syndrome **Benign congenital conjugated hyeprbilirubinaemia Gilbert’s Syndrome Present in 5% of the population •Males > females •Genetic origin – insertion of TA in promoter region of UGT-1A gene •Exacerbated by fasting and illness •Confirm conjugated hyperbilirubinaemia •Rule out haemolysis FBC, Reticulocyte count •Rule out underlying liver disease - Causes of neonatal jaundice Unconjugated bilirubin level > 300μmol/L may be associated with Kernicterus (brain damage due to uptake of unconjugated bilirubin) Patterns of LFTs Hepatocellular •Predominant elevation in AST/ALT – Cholestatic •Predominant elevation in ALP with GGT ± Bilirubin Mixed •Elevation in both AST/ALT, and ALP/GGT ± Bilirubin Causes of a Hepatocellular Pattern of LFTs Marked elevations in ALT/AST > x5 URL (patient likely to be symptomatic) •Viral hepatitis •Ischaemic hepatitis •Autoimmune hepatitis •Drug/toxins e.g. alcoholic hepatitis Mild/Moderate elevations in ALT/AST < x5 URL (patient may be asymptomatic) •Chronic Hepatitis •ALD •NAFLD/NASH – associated with obesity, T2DM, Hyerlipidaemia •Metabolic liver disease - HH, WD, A1AT •Drugs •Autoimmune LD Approach to an asymptomatic patient with elevated ALT/AST Elevated AST/ALT ? Muscle problem Repeat test Normal Still Elevated Check CK Elevated Normal Likely Liver Aetiology Drug Hx etc Viral serology AI hepatitis screen Fe/TIBC/Ferritin/HFE genotyping Caeuruloplasmin if < 40 yr A1AT Coeliac screen Ultrasound scan MRI/CT Bx Causes of a Cholestatic Pattern of LFTs Elevated ALP and GGT ± Bilirubin, relative to transaminases Intrahepatic (Bilirubin not elevated) Extrahepatic (Bilirubin elevated) •Medications •TPN •Sepsis •Postoperative •PBC •Alcoholic hepatitis •Liver mets •Pregnancy-related •CCF •Cholelithiasis (CBD) •Malignancy – HOP, •Primary sclerosing cholangitis GGT is useful in differentiating Liver as a cause of elevated ALP An approach to the patient with isolated elevation in ALP Elevated ALP Normal ?bone, placenta, Intestine etc. What is GGT? Elevated US/CT/MRI Biliary dilation No abnormality Focal mass Medications PBC -AMA Consider other causes Specialised investigations Other LFTs Serum ammonia -used for investigation of hepatic encephalopathy -lacks sensitivity and specificity -useful for investigation of urea cycle disorders Serum LDH -included in LFTs in SJH -5 isoenzymes – heart, erythrocytes, skel mus, liver, others -not specific for liver - ? role in ischaemia-related abnormal LFTs -useful in monitoring certain malignancies e.g. B-cell lymphoma - “not really a LFT” Reference Ranges for LFTs Biochemistry Department, St James’s Hopsital Albumin Bilirubin 35-50 g/L <17 umol/L ALP* 40-120 IU/L* AST ALT 7-40 IU/L 7-35 IU/L GGT 10-55 IU/L * NB: Reference Range is age related Case 1 24 yr old male Insurance medical showed abnormal LFTs ? Cause Albumin Bilirubin 42 (35-50 g/L) 38 (<17 umol/L) ALP 98 (40-120 IU/L) AST ALT 30 (7-40 IU/L) 28 (7-35 IU/L) GGT 37 (10-55 IU/L) What further tests are indicated? What is the most likely cause of raised Bilirubin? Case 2 35 yr old female with a 4/52 hx of -malaise, anorexia, upr abdominal pain, ?haematuria -O/E Icteric Alb Bilirubin 35 126 ALP 250 (40-120) AST 1459 ALT 2009 GGT 331 What further investigations are indicated? What fraction of her bilirubin is elevated and how does this impact on her “haematuria”? Case 3 You are phoned about the following results and asked to comment on the ALP which appears to be elavated? Pt is a 17 yr old male – clinical details Alb Bilirubin ALP 46 12 220 (40-120) AST ALT GGT 20 20 9 “still growing” What is the likely cause for the elevated ALP? Which isoenzyme is increased? Case 4 48yr old female is attending a lipid-clinic -polygenic hypercholesterolaemia -On atorvastatin 20mg/d for 2 years -C/o tired fatigue, malaise Alb TBilirubin ALP 42 8 250 (40-120) AST ALT GGT 38 26 220 LFTs measured 6/12 previously were normal What further investigations would you perform? What is the differential diagnosis? Case 5 37 yr old male is referred to a lipid clinic with ? Mixed hyperlipidaemia (Chol 7.0 Trigs 5.2) -BMI 35, WC=120cm -Normotensive -Otherwise clinically well Fasting Glucose Alb 6.8 mmol/L 38 TBili ALP AST 15 82 58 ALT GGT 72 67 (<55) What further investigations would you suggest and why? Case 6: Background Phonecall from a GP regarding LFTs 72yr old female with discomfort in R hypochondrium No other hx of note Not on medications No C2H5OH Case 6: LFTs Alb (35-50) Tbili (3-17) AST (7-40) ALT (7-35) Alk Phos (40-120) GGT (5-40) LDH (230-450) CK (34-170) 28/4 3/5 39 10 113 39 6 106 95 372 930 495 82 352 874 426 Case 6: Further investigations Mixed cholestatic and hepatocellular liver disease Fe, TIBC, TS% - all normal Hepatic Antibody screen – negative Ultrasound of Upr Abdomen recommended Gallstones diagnosed Case 7: Background •47 yr old male •Hx – malaise and ?icterus (confirmed in sclera) •No recent hx C2H5OH excess or medication 6/5 12/5 Alb 45 43 TBili 181 242 Alk Phos 454 408 GGT 813 428 AST 344 75 ALT 707 Case 7: Dx •Predominant hepatitic picture •Resolving to cholestatic LFTs Probable acute viral hepatitis Case 8 24 yr old male -Vague hx of feeling unwell, also wt loss >7Kg -? Eating disorder/psychiatric illness 7/3 4/4 Alb 51 50 Tbili (3-17) 93 48 Conj Bili 9 Alk Phos 74 84 GGT 14 18 AST 25 23 Case 8: Further Investigations FBC and Reticuloctye count – normal Viral Hep screen – normal Hep antibody screen – normal U/S – normal Biochmeical Dx: -unconjugated Hyeprbilirubinaemia (Gilbert’s syndrome) -confirmed by genetics Case 9: Why the elevated LFTs? 52 yr old male No medical hx of note Not on regular medications Non-specific hx Routine Bloods done by GP “Family Hx IHD” written on request form Case 9: Results Fasting Lipid and Glucose – unremarkable AST = 243, LDH = 1525 (230-450) GGT = 85 (10-55) other LFTs normal GP surprised at the raised AST ? Further investigations Case 9: Further Investigations ALT = 50 (7-35) CK 1191 (29-195) CK-MBmass = 132 (<12) CK-MB fractionation 10% (<6%) Case 9: Dx GP practice contacted: -Informed by Registrar that results were of concern -needed to be communicated to GP -1day later Consultant phoned to see if action had been taken -Pt contacted and advised to present to A/E SJH Troponin T = 3.25 (<0.01) Acute Coronary Syndrome (Acute MI) PTCA and stenting performed Paracetamol Overdose •Hepatic necrosis observed within 36-72 hours •Accumulation of breakdown product NAPQI Early diagnosis and treatment of paracetamol OD is essential •Ideally before 12 hours post ingestion •N-acetylcysteine (Parvolex) is an effective agent Iron Overload Syndromes Primary: Hereditary Haemochromatosis (HH) Secondary: Non HH Cirrhosis Ineffective erythropoiesis – sideroblastic anaemia, Thalassaemia Multiple transfusions Bantu siderosis Porphyria Cutanea Tarda (PCT) Hereditary Haemochromatosis Autosomal recessive Mutations in HFE gene -C282Y -H63D 93% associated with homozygosity C282Y + 6% associated with compound heterozygosity C282Y + H63D 1% No mutations identified Clinical presentation of HH Males > females Usually in middle age Clinical presentation caused by iron accumulation in Liver – fatty change Cirrhosis Pancreas – Diabetes Heart – dilated cardiomyopathy Joints – arthropathy Pituitary – secondary hypogonadism (males > females0 Testses – primary hypogonadism (rarer) Parathyroid - hypocalceamia Diagnosis of HH •Increased Transferrin Saturation (Plasma Fe/TIBC) 55% - genotype 45-55% - may consider genotype •Increased Ferritin •HFE genotype •Liver Biopsy •Liver Iron content Figure A H63D C282Y 1 2 1 3 2 3 1. Homozygous mutant 1. Homozygous mutant 2. Heterozygous 2. Heterozygous 3. Wild type (normal) 3. Wild type (normal) Case Example : Haemochromatosis 51yr old male Total protein Total Bilirubin Alk Phos GGT AST ALT Serum Fe TIBC Transferrin sat Ferritin 71 14 82 39 44 92 38 41 93% 1,316 HFE genotype C282Y homozygous –Hereditary Haemochromatosis Wilson disease Autosomal recessive Associated with mutations in ATP7B (Cu transporting P type ATPase) Clinical presentation – Children and adults usually < 40 years •CNS – extrapyramidal system, Kayser-Fleischer rings in cornea •Liver – fatty liver, cirrhosis,acute fulminant hepatic failure •Kidney, Haemolytic anaemia Dx: Low plasma caeruloplasmin Increased Urinary Cu excretion (Penicillamine Challenge Test) Liver Bx – measure Cu content