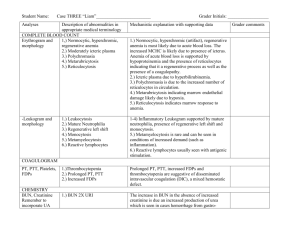
ALP
advertisement

Liver Function Tests รองศาสตราจารย์ แพทย์ หญิงพรรธนมณฑน์ อุชชิน ภาควิชาเวชศาสตร์ ชันสู ตร คณะแพทยศาสตร์ จุฬาลงกรณ์ มหาวิทยาลัย วัตถุประสงค์ : หลังจากเสร็จสิ้นการเรียน นิสิตสามารถ 1. อธิบายลักษณะทั่วไปของตับ 2. เข้ าใจหน้ าทีส่ าคัญของตับ(Major Functions of the Liver) 3. แยกชนิดและอธิบายการเกิด Jaundice ชนิดต่ างๆ ในร่ างกาย 4. เข้ าใจ Pathway of Bilirubin 5. รู้ จักInherited Disorders of Bilirubin Metabolism 6. รู้ จกั ชนิดต่ างๆของ LFTs 7. เข้ าใจหลักการและแปลผล routine LFTs ทีเ่ ลือกได้ 8. อธิบายสาเหตุและเลือกใช้ LFTs ทีเ่ หมาะสมสาหรับโรคตับและทางเดิน นา้ ดีทพี่ บบ่ อยๆได้ 9. แปลผล LFTs ทีเ่ ลือกใช้ ได้ LIVER Blood supply 15 ml/min : Portal vein, Hepatic artery Parenchymal cells : Hepatocyte Nonparenchymal cells : Endothelial cells Kupffer cells Hepatic stellate cells Pit cells Hypoglycemia Major Functions of the Liver 1. Synthesis and metabolism of proteins,carbohydrates and lipids 2. Production, metabolism and excretion of bile Detoxification and drug metabolism Enzymes synthesis Storage of vitamins and minerals 3. 4. 5. 6. 7. Biotransformation or Inactivation of hormones Phagocytosis Synthesis & metabolism of proteins,carbohydrates and fats 90 % of plasma protein ( except for gammaglobulin, hemoglobin ) nutrition, oncotic pressure, transportation glycogenesis, glycogenolysis, glycolysis, gluconeogenesis triglycerides, VLDL, LDL, HDL, cholesterol Production, metabolism and excretion of bile น้ำดี : bilirubin, bile acids / salts, electrolytes, cholesterol, fatty acids, น้ำ, lecithin primary bile acids : cholic, chenodeoxycholic acids secondary bile acids : deoxycholic, lithocholic acids enterohepatic circulation bilirubin : hemoglobin, myoglobin, cytochromes, catalase unconjugated bilirubin ( + albumin ) Production, metabolism and excretion of bile Protein Y & Z , Ligandin UDPG - T ( Uridyldiphosphate glucuronyl transferase ) conjugated bilirubin ( + glucuronic acids ) urobilinogen, stercobilin biliprotein ( delta bilirubin ) jaundice / icteric ( TB > 2.5 mg /dl ) Jaundice classified by origin 1. Prehepatic ( TB < 5 mg/dl) : Hereditary hemolytic processes Acquired hemolytic processes Ineffective erythropoiesis Impaired delivery of bilirubin to the liver Sport injuries Jaundice classified by origin 2. Hepatic : Pre - microsomal Microsomal Post - microsomal Intrahepatic obstruction 3. Posthepatic : CBD stones Cancers of the bile ducts, pancreas Stricture, stenosis, atresia Cholagitis, Choledochal cysts Physiological classification of Jaundice 1. Unconjugated Hyperbilirubinemia Production Delivery to hepatocyte Uptake across hepatocytic membrane Storage in cytosol Conjugation Physiological classification of Jaundice 2. Conjugated Hyperbilirubinemia Secretion into canaliculi Drainage Intrahepatic obstruction Septicemia, total parenteral nutrition Drugs Inherited Disorder of Bilirubin Metabolism Gilbert’s syndrome : mild fluccuate unconjugated hyperbilirubinemia conjugation +/- uptake normal lifespan Crigler - Najjar syndrome : severe unconjugated hyperbilirubinemia Type I : absence of UDPG - T Type II : partial defect of UDPG - T Inherited Disorder of Bilirubin Metabolism Dubin - Johnson syndrome : mild fluccuate conjugated hyperbilirubinemia hepatic excretion normal lifespan hepatic pigmentation, bilirubinuria Rotor syndrome : unknown defect similar to Dubin - Johnson syndrome no hepatic pigmentation Detoxification and Drug Metabolism Phase I : oxidation, hydroxylation Phase II : conjugation with glucuronic acid, glycine, taurine and sulfate Cytochrome P450 and allied hepatic enzyme system Epoxide hydrolase UDP - glucuronosyl transferase Sulphotransferase Glutathione S - transferase Enzymes Synthesis Cytoplasmic enzyme : AST(SGOT), ALT(SGPT), LD Mitochondrial enzyme : AST Canalicular enzyme : ALP, GGT Storage of Vitamins and Minerals Fat soluble vitamins ( A, D, E, K ) Vitamin B12 Iron Copper Biotransformation or inactivation of hormones Somatomedin Glucagon Phagocytosis Kupffer cells Pit cells LIVER FUNCTION TESTS 1. Routine ( Conventional ) LFTs bilirubin, urobilinogen, ALP, AST, ALT, GGT 2. True tests of liver function ( QLFTs : Quantitative LFTs ) Dynamic test ; measure metabolite / excretion rate, liver blood flow or functional hepatic mass QLFTs Metabolic Capacity : Indocyanine Green ( ICG ) test 14C- Galactose breath test Microsomal enzyme function : Aminopurine breath test Caffeine breath test Functional hepatic perfusion : Galactose tolerance test ICG ( low dose ) test Microsomal enzyme function and hepatic perfusion : Lidocaine clearance test LIVER FUNCTION TESTS 3. Provide information about severity and prognosis TP, Alb, Clotting factors, Ammonia 4. Special laboratory tests Alpha-1-antitrypsin, Alpha-fetoprotein, Autoantibodies Ceruloplasmin, Copper, Hepatitis markers Immunoglobulin, Iron and ferritin, Glutamine, LD Serum Bilirubin Newborn (Direct spectrophotometric method) > 1month (Colorimetric Wahlefeld method) Urobilinogen in urine & feces Urinary urobilinogen Hemolytic disease Viral hepatitis Fecal urobilinogen Biliary obstruction Hepatocellular disease LIVER ENZYMES Principles of Diagnostic Enzymology Half - life of liver enzymes in serum ALP ………..3 - 7 วัน ALT……….. 50 ชั่วโมง AST…………12 - 14 ชั่วโมง GGT………..7 - 10 วัน Factors affecting enzyme levels in serum 1. Leakage of enzymes from cells Hypoxia, Chemicals and drugs, Physical agents, Microbiological agents, Immune mechanisms, Genetic defects, Nutritional disorders 2. Altered enzyme production 3. Clearance of enzymes average half - life in serum 6-48 ชั่วโมง Characteristics of Elevated Concentration Mild : AST, ALT, GGT < 2 - 3 x URL ALP < 1.5 - 2 x URL Moderate : AST, ALT up to 20 x URL GGT up to 10 x URL ALP up to 5 x URL Marked : AST, ALT > 20 x URL GGT > 10 x URL ALP > 5 x URL AST &ALT Mild : Fatty liver NASH ( Nonalcoholic steatohepatitis ) Chronic viral hepatitis Marked : Acute viral hepatitis Drug or Toxin induced hepatic necrosis Ischemic hepatitis AST &ALT > 2 : Alcoholic liver disease > 1 : Cirrhosis < 1 : NASH Viral hepatitis Aspartate Transaminase (AST,SGOT) UV assay : Pyridoxal phosphate Tissue Sources : cardiac tissue, liver, skeletal muscle, kidney, pancreas, RBC Sources of Error : hemolysis Diagnostic Significances : Cardiac disease, Hepatobiliary disease, Major crush injuries, Skeletal muscle disease, Pancreatitis, Delerium tremens. Pregnancy Alanine Transaminase ( ALT,SGPT ) UV assay : Pyridoxal phosphate Tissue Sources : liver Sources of Error : hemolysis Diagnostic Significances : Hepatobiliary disease, Heart failure with hepatic necrosis Alkaline Phosphatase ( ALP ) ALP > 3 x URL Hepatobiliary disease ( cholestasis ) Marked increase Extrahepatic biliary obstruction PBC ( Primary Biliary Cirrhosis ) PSC ( Primary Sclerosing Cholangitis ) Drug - induced cholestasis Mild - moderate increase Amyloidosis Granulomatous disease Neoplasms, Hodgkin’s disease Renal cell carcinoma Alkaline Phosphatase ( ALP ) Colorimetric assay : ++Mg Tissue Sources : intestinal epithelium, liver (sinusoidal and bile canalicular membrane), bone (osteoblast), kidney tubules, placenta, spleen Sources of Error : phosphate, borate, oxalate, cyanide, Lphenylalanine, urea, hemolysis Diagnostic Significances : Hepatobiliary disease, Bone disease, Healing fracture, Normal growth,Pregnancy Hereditary hypophosphatasia Alkaline Phosphatase ( ALP ) Diagnostic Significances Isoenzymes ; liver(heat stable), bone(heat labile), intestinal and placental Placenta-like ( Regan & Nagao ) ; germ cell tumors, seminoma, serous carcinoma of ovary, endometrial carcinoma and leukemia - Glutamyl Transferase ( GGT ) Enzymatic Colorimetric assay Tissue sources : cell membrane and mitochondria Sources of Error : smoking, pregnancy, alcohol, phenytoin, barbiturate, carbamazepine, valproic acid,oral contraceptive - Glutamyl Transferase ( GGT ) Diagnostic Significances : ), Hepatobiliary disease, Hepatic microsomal enzyme induction ( drugs ; warfarin, phenytoin, phenobarbital Alcoholism and heavy drinking, Pancreatitis, Diabetic mellitus, Congestive cardiac failure Lactate Dehydrogenase ( LD, LDH ) UV assay Tissue Sources : myocardium, kidney, liver, skeletal muscle and RBC Sources of Error : hemolysis Diagnostic Significances : AMI, Hepatobiliary disease,Renal disease, Cancers, Anemia, Progressive muscular dystrophy, Isoenzymes( LD1,2,3,4,5 ) Liver Enzymes Routine AST, ALT, ALP Liver specific OCT (Ornithine Carbamoyl Transferase) ID (Iditol Dehydrogenase), Guanase hepatic isoenzyme of ALP Liver Enzymes Interpretation AST&ALT ………..hepatocellular damage ALP…………………cholestasis Plasma Proteins Colorimetric assay Hyperproteinemia : Dehydration, Liver diseases, Chronic inflammatory diseases, Increased plasma immunoglobulins, Faulty technique in blood sample Hypoproteinemia : Overhydration, Pregnancy, Malnutrition, Liver diseases, Protein loss, Hypogammaglobulinemia, Hyperthyroidism Albumin Colorimetric assay : Dye-binding method Sources of Error : hemolysis Hypoalbuminemia : Hereditary defects, Malnutrition, Malabsorptive disease, Severe burn, Shock, Chronic liver disease, Major surgery, Accidental trauma, Infection, Renal disease, Exfoliative dermatitis Protein-losing gastroenteropathy, Clotting Factors Quick’s One Stage Prothrombin Time or Plasma Prothrombin Time Extrinsic pathway Factors : I, II, V, VII, X INR ( International Normalized Ratio ) Ammonia Enzymatic kinetic assay EDTA plasma, hemolysis, protein in food, drugs, exercise Diagnostic Significances ; Reye’s syndrome, Liver disease, Cirrhosis, Hepatic coma, Hyperornithinemia Unexplained lethargy and vomiting, Encephalitis & Neonate with unexplained neurologic deterioration Ceruloplasmin(CERU; Cp ) Ferrioxidase activity, acute phase protein Immunoturbidimetric method Serum, heparinized plasma, hemolysis, lipemia & rheumatic factors Diagnostic Significances ; Wilson’s disease, Monkes disease, Nutritional copper deficiency, Renal copper loss, Massive burn, Inflammation disease, RE neoplasia, Biliary obstruction, Estrogen therapy, Pregnancy Most Common Disease of Liver 1. Hepatitis : Acute ( viruses, toxins and drugs ) recovery from viral hepatitis ...transaminases are normal within 10-12 weeks ( > 6 months ………chronic ) Chronic ( autoimmune, viruses, alcohol and drugs ) : normal ALP, increased AST&ALT abnormal Albumin & PT Most Common Disease of Liver 2. Cirrhosis : Chronic excessive alcohol intake Autoimmune chronic active hepatitis Chronic hepatitis B, C, D, Inherited metabolic disease : Wilson’s disease, DM, Glycogen storage disease, Galactosemia Disease of Prolonged Cholestasis : PBC, PSC, Cystic fibrosis, Biliary atresia *decompensated cirrhosis…increased blood ammonia Most Common Disease of Liver 3. Tumours Metastatic : primary sites ; lung, bronchus, breast, gastrointestinal tract, prostate gland *normal TB, AST, mild increases of GGT and ALP with marked increase of LD Hepatoma : Cirrhosis, Hepatitis B, C, Aflatoxins *increases of alpha-fetoprotein and ALP Differential of Hepatocellular Injury and Cholestasis Test Hepatocellular Injury Cholestasis ALT > 10 x URL < 10 x URL ALP < 3 x URL > 3 x URL GGT < 5 x URL > 5 x URL Bilirubin DB 50-80% DB 50-80% PT No Respond to Vit K Imaging studies Normal ducts Abnormal ducts Pattern of Cholestasis Bilirubinostasis………… Hepatocyte Cholestatic hepatitis……Canalicular Ductular injury……………Intrahepatic bile ducts Complete obstruction… Extrahepatic bile ducts Some Drugs causing liver diseases Hepatotoxicity Cholestasis Cholestatic hepatitis Paracetamol (overdose) Methyltestosterone Chlorpromazine Salicylate( high dose) Erythromycin Tetracycline ( high Chlorpropamide dose) Rifampicin Comments for Interpretation of LFTs 1. Definite diagnosis : special tests or liver biopsy 2. ALP, GGT and 5’- NT 3. Moderated or marked increase of ALP 4. AST, ALT > 10 x URL… hepatocellular damage 5. ALP > 3 x URL….cholestasis Comments for Interpretation of LFTs 6. Prolongation of PT a. vitamin K…Advanced liver destruction b. vitamin K…Vitamin K deficiency or Long-standing extrahepatic obstruction 7. Bile acids analysis….Inactive cirrhosis 8. Liver scan……Metastatic carcinoma 9. U/S & PTC….Extra / intrahepatic obstruction 10. Repeat LFTs …..2 -3 days Thank you for your attention