REFRACTION
advertisement
REFRACTION
Dr. Puneet Kumar Srivastava
Refraction
• Def: Method of evaluating the optical state of
eye.
•
Or
The process by which the patient is guided
through the use of a variety of lenses so as to
achieve the best possible acuity on distance
and near vision test.
• Acc. To the physicist, Refraction is defined as
bending of light rays when it passes from one
media to other having diff refractive indices.
Five Activities
1.
2.
3.
4.
5.
Retinoscopy (Objective Refraction)
Cycloplegia / Mydriasis
Refinement (Subjective Refraction)
Binocular Balancing
Prescription Of Spectacle Lenses
Ophthalmic Optics
• Principle of Vergence:
• Reciprocal of the distance from the lens to the
point of convergence of light.
• Divergent:
• Light rays that are moving away from each other.
• Convergent:
• Light rays that are moving towards each other.
Parallel rays have zero vergence
• Vergence Power:
• Describes the ability of a curved lens to converge or
diverge light rays.
• Divergent Power: “-” minus
• Convergent Power: “+” plus
• Diopter (D):
• Unit of measurement of the refractive power of a lens.
• Focal Length (f):
• Distance between the lens and the image formed by an
object at infinity
•
f =1/D
Convex Lens
Identification of a Convex lens:
1. Thick at center, thin at periphery.
2. Object held close to the lens appears magnified.
3. When it is moved, the object seen through it
moves in opposite direction to the lens.
Image formed by a convex lens:
Real, inverted & magnified.
Concave Lens
Identification of concave lens:
1. Thin at center, thick at periphery.
2. An object seen through it appears minified.
3. When it is moved, the object seen through it
moves in the same direction as the lens.
Image formed by a concave lens:
Virtual, erect and diminished.
D= 1/f
o1D of plus power converges / minus power diverges
parallel rays of light to focus at 1 meter on opposite
side / same side respectively from lens.
o +/- 0.25D ---------- +/- 4 meters.
o +/- 4D ---------------- +/- 0.25 meters.
• Cylinder lens:
• Vergence power is in only one meridian, the one
perpendicular to the axis of the cylinder.
• Spherico- cylinder (Compound lens, Toric lens):
o Focus light in two line foci.
o The shape of the light rays as they are focused by
the spherico-cylinder lens called the-conoid of sturm
o Between the two line foci produced by the conoid
of sturm is a point called the-Circle of Least Confusion (point of best overall focus
for a sphericocylindrical lens.
Strum’s Conoid
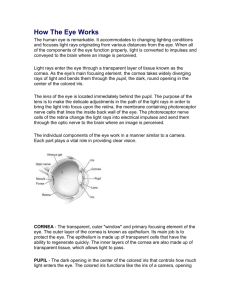
Refractive State of eye
• Emmetropia:
• Parallel light rays are focused sharply on retina.
• Ammetropia:
• Unable to bring parallel light rays into focus.
• Types:
1. Myopia
2. Hypermetropia
3. Astigmatism
Emmetropia
o It’s a optically normal eye.
o In emmetropic eye, parallel light rays are focused
sharply on sensitive layer of retina with the
accommodation at rest.
What happens to the light rays coming
from the FP and entering the eye?
o In emmetropia the FP is at infinity. So the rays coming
from FP, and entering the eye are parallel. They are focused
upon the retina (with accommodation at rest) to give a clear
image of object at FP.
Myopia
o Short sightedness, excessive convergent power
o Parallel rays of light coming from infinity are
focused in front of retina when accommodation is
at rest.
o In myopia the FP is at a finite distance.
oSo, the rays coming from object at the far point, and
entering the eye are divergent.
oThese rays are focused upon the retina to give a
clear image (with accommodation at rest).
Hypermetropia
oLong sightedness, Insufficient convergent power.
oParallel rays of light coming from infinity are focused
behind the retina with accommodation being at rest.
oThe posterior focal point is behind the retina, which
therefore receives a blurred image.
o In hypermetropia object can't be placed at the FP ( It is a
virtual point behind the retina).
o Here the converging rays directed towards the FP behind
the retina can be focused upon the retina to give a clear
image by the dioptric (optical) system of the eye (with
accommodation at rest).
o The Far Point and the Point of Focus on the retina are
Conjugate Foci.
Astigmatism
o Refraction varies in different meridia.
o The rays of light entering the eye cannot converge
to a point focus but form focal lines.
TYPES:
o Regular astigmatism:
When refractive power changes uniformly from one
meridian to another.
o Irregular astigmatism:
Irregular changes of refractive power in different
meridian.
Retinoscopy
o Objective Refraction
o Skiascopy or Shadow test
o The goal of retinoscopy is to determine the nature
of pat.’s refractive error (if any) and approx. lens
power that will diminish (neutralize) that error and
approach clear vision.
o Types : -Manual
-Automated
Prerequisites for Manual Retinoscopy
1. Dark room
2. Mydriatic / Cycloplegic
3. Leister’s bulb( 50W / inside Hg, outside black /
aperture -1 big, 2 small 2cm)
4. Retinoscope – Priestly – Smith R.
- Plane mirror R.
- Streak R.
5. Trial Frames / Halberg clip
6. Trial set
Commonly used Cycloplegics:
Cyclopentolate Hydrochloride (0.5-1%)
- Drops applied 2-3 times at 5 minutes interval.
- Retinoscopy is done after 30 minutes.
- Effect lasts for 8 hours.
Tropicamide (0.5-1%)
- Drops applied 2-3 times at 5 minutes interval.
- Retinoscopy is done after 30 minutes.
- Effect lasts for 8 hours
Atropine Sulphate (0.5 – 1%):
- lower strength below 5 years of age
- Used for cycloplegia in children <7–10yrs of age.
- In cases with ciliary spasm and in Convergent
Strabismus.
- Effect lasts for 2 weeks.
Homatropine Hydrobromide (1 – 2%)
- Drops applied at 15 minutes interval for 6-8 times.
- Retinoscopy is done after 1 hour.
- Effect lasts for 2 days.
Retinoscopes
Priestley–Smith retinoscope:
o Plane mirror at one end /concave mirror at other
end.
oHole- 2.5mm ant. ; 4.0mm post.. Fitted with low
polar convex lens.
oProjects a circle of light in the patient’s pupil.
Streak retinoscope
o Self illuminating, projects a streak.
oWe can rotate the streak in diff angles.
Trial Frame
Trial Set
• Typical “Trial Set” will have:o Spheres - every quarter of a diopter to 4D, every
half to 6D, every diopter to 14D, every 2D to 20D.
o Cylinder – every quarter of a diopter to 2D. Every
half to 6D.
o Prism – upto 10 PD, additional 15 & 20 PD.
o Plano lenses
o Opaque disc
o Pin hole
o Stenopaeic discs
o Maddox rods
o Red & Green glasses
Principle Of Retinoscopy
o Retinoscope illuminates an area of the retina, the
image of this area formed at the pat.’s far point.
- observer views rays of light emanating from the
illuminated retina through pat.’s pupillary area from
a working distance.
-Depending upon the behavior of reflex the observer
knows whether emerging rays are –
- Convergent, Divergent or Parallel.
o Lenses from the trial set are used to neutralize the
movement (neutralization point = subject’s far
point coincides observer’s nodal point.)
Optics of Retinoscopy
o In retinoscopy an illuminated area of retina serves
as an object, & the image at the far point of the eye
located by moving the illumination across the
fundus & noting the behavior of the luminous reflex
in the pupil.
o The observer does not see the illuminated area of
the pat.’s fundus, but only the rays emanating from
it to form an illuminated area of the pupil.
Working Distance
o The distance between the examiner and the
patient’s eye is measured and converted to diopter.
o Usually, most examiners uses a working distance of
a arm length i.e, approx. 66cm / 2/3m / 26 inches.
o D=1/f i.e, D=1/2/3 i.e, D=3/2 i.e, D=1.5D
o This power is then substracted from the final
dioptric amount that is measured.
o The working distance must remain constant through
out the examination.
Far Point
o Far Point (FP) is the furthest point at which objects
can be seen clearly by the eye. Object kept at FP of
the eye can be seen clearly with accommodation at
rest.
o Position of FP depends on the optical state (static
refraction) of the eye.
o In emmetropia it is at infinity.
o In myopia it is at a finite distance.
o In hypermetropia it is a virtual point behind the
retina.
o Type of mirror we are using to reflect the rays from
the original source of illumination is also a factor
deciding the optics.
o If we are using a Plane mirror, the virtual image of
the original source of illumination is formed as far
behind the mirror as the original source is in front of
it.
o So, the tilt of the mirror to one side will shift the
image (immediate source of illumination) to the other
side.
o Tilt of the plane mirror and the shift of illuminated
patch on the retina are in the same direction.
o If we are using a Concave mirror, the real image of
the original source of illumination is formed in front
of the mirror ( position depends on the focal length of
the mirror).
o So, the tilt of the mirror to one side will shift the
image (immediate source of illumination) to the same
side itself.
o Tilt of the concave mirror and the shift of
illuminated patch on the retina are in opposite
directions.
o If the image is formed between pat. & observerAgainst movement.
Seen in- 1. Myopia > 1.5 D
o If the image is formed either behind the pat.’s eye
or behind the observer’s- With movement.
Seen in- 1. Emmetropia
2. Hypermetropia
3. Myopia < 1.5 D
o The point of reversal or neutral point of retinoscopy
is reached when the subject’s far point coincides
with the observer’s nodal point & examiner see a
diffuse bright red reflex in the pat.’s pupil & no
movement of the reflex is discernible.
The detail optics is most easily considered
in three stages:
1. Illumination Stage: The illumination of the
subject’s retina.
2. Reflex Stage: The reflex imagery of the illuminated
area formed by the subject’s dioptric apparatus.
3. Projection Stage: The projection of image by the
observer.
ILLUMINATION STAGE
REFLEX STAGE
o The S1 is a finite distance from the subject and the eye is
emmetropic, an image of S1 will be formed behind the retina.
oThe illuminated patch can now be considered as an object in its
own right and will form an image at the far point of eye, which in
emmetropia is at infinity
oReflex stage is so called because the light is actually reflected
from the fundus.
PROJECTION STAGE
Retinoscopy Reflex
Clues we get from features of retinoscopy reflex -
1. Intensity:
In high refractive errors we get a faint reflex and in low refractive errors we
get a brighter reflex.
2. Speed:
In high refractive error we get a slow movement, and in low refractive error
a rapid movement of the reflex.
As the neutral point is reached the movement of the reflex is fast.
3. Size:
In high refractive error we get a narrow reflex.
Reflex will fill the pupil when the neutral point is reached.
In very high refractive errors we may not get a reflex
or may get a faint reflex with negligible movement. We
will not get a good reflex with low power lenses in these cases.
So try with high plus or minus lenses
o In Optics Direction of Light Ray is Reversible.
o What happens to the light rays coming out of the eye from
a point on retina?
o They meet at the FP of the eye (when the accommodation
is at rest).
o In emmetropia light rays coming out from a point on the
retina through the optical system of the eye will be parallel
(when the accommodation is at rest).
o These rays can meet only at infinity ( ie. where the Far Point
is located in emmetropia).
o In myopia light rays coming out from a point on the retina
through the optical system of the eye will be convergent.
o These rays meet at the FP of the eye (at a finite distance)
when the accommodation is at rest
o In hypermetropia light rays coming out are divergent.
oThey will only meet "beyond infinity" when the
accommodation is at rest.
o They can meet only at the FP of the eye, which is a virtual
point behind the retina, by extrapolating the divergent rays in
the reverse direction to meet behind the retina.
o If we can locate the Far Point of subject's eye, then we can calculate
the refraction of that eye. But observer moving towards FP is not
practical. (In emmetropia FP is at infinity and in hypermetropia FP is
virtual point behind patient's eye).
oThe method used for calculation is keeping the subject and the
observer at fixed places, and bringing (shifting) the FP of the subject to
the position of the nodal point of observer's eye.
o This is done by using converging or diverging lenses.
o Now we know the exact distance of the FP from patient's eye (ie.
exact distance at which we are sitting) and also the power of lens used
to bring the FP to this position.
oFrom the measurement of distance we can calculate the power
required to bring the FP to this position in emmetropia –
o I call it observer factor - The power used other than this power, gives
the refractive error - patient factor .
o The Total Power of lenses we use contain two parts.
o First one is the power used because of the position of the
observer (Observer Factor or Induced Factor or False
Factor). If the subject is emmetropic this is the only factor
that will be there. This is the power used, only because of
the position of the observer and not because of the
patient's refractive error.
o Second part is the power of lenses used because of the
patient's refractive error (Patient Factor or True Factor).
o From the above three values we can calculate the
refraction of the subject's eye.
o Total Power = Observer Factor + Patient Factor.
I.e, Total Power - Observer Factor = Patient Factor
(Refraction of Patient's Eye).
Practical Aspect
o If the observer is at a distance of one metre from
the subject the Observer Factor is +1.0 Dioptre. (+1
Dioptre is the power of the lens which can focus
parallel rays at 1 metre.) Then...............
o In emmetropia the parallel rays coming out of the
subject's eye can be brought to a focus at 1 metre by
using converging (convex) lens of 1 Dioptre kept close
to subject's eye.
o In other words, if the power of the lens used to
bring the FP to 1 metre is +1 D then we know that the
rays coming out are parallel (which normally meet at
infinity) and the eye we are examining is emmetropic.
o Total Power = +1 D,
oObserverFactor = +1 D.
o So, Patient Factor is 0 (zero)
o Total Power - Observer Factor = Patient Factor
(Ref.Error)
o (+1) - (+1) = 0 (zero) Subject is emmetropic.
o In hypermetropia the diverging rays coming out of the
eye are brought to a focus at 1 metre by using
converging lenses of power more than +1 D.
o (+1 required for parallel rays in emmetropia).
o The power used in excess of +1 D is the measure of
hypermetropia of that eye.
o Total Power = +3 D,
o Observer Factor = +1 D.
o So, Patient Factor = +2 D
o Total Power - Observer Factor = Patient Factor.
o I.e, (+ 3) - (+1) = +2.
o This means the patient is 2 Dioptres
Hypermetropic.
o In myopia of less than 1 Dioptre the converging
rays coming out are focused at 1 metre by using
converging lens of power less than +1 D .
o This difference in power compared with the
emmetropic eye will give the exact measure of
myopia.
o Total Power= +0.50 D,
o Observer Factor = +1 D.
o So, Patient Factor = -0.50D
o Total Power - Observer Factor = Patient Factor (Ref.
error)
o (+0.50) - (+1.0) = - 0.50
o Patient is 0.50 Dioptre myopic.
o In myopia of 1 Dioptre the rays coming out of the
eye are convergent and meet at 1 metre with out
using any lens.
o In other words if we are not using any lens to bring
the FP to 1 metre we know that we are dealing with
an eye which is 1 D myopic.
o Total Power = 0 (zero),
o Observer Factor = +1 D,
o So, Patient Factor = - 1.0 D.
o Total Power - Observer Factor = Patient factor
o ( 0 ) - ( + 1.0 ) = - 1.0
o Patient is 1 Dioptre myopic.
o In myopia of more than 1 Dioptre the converging rays
coming out of the eye will focus at the FP which is less than
1 metre from the eye. (between the patient and the
observer).
o So, this focus (FP) can be brought to 1 metre by using
diverging (concave) lens.
o So this much of diverging (minus) power is in excess when
compared with an eye with FP at 1 metre (ie.eye with 1 D
myopia).
o Total Power = - 2.0 D,
o Observer Factor = +1D,
o So, Patient Factor = - 3.0D.
Total Power - Observer Factor = Patient Factor
(ref.error)
o ( - 2.0 ) - ( + 1.0 ) = - 3.0
o Patient is 3 Dioptre myopic.
How do you know that you are at the FP of
the Subject's eye ?.
o The technique of Objective method of Refraction
(Retinoscopy) will answer these questions.
o Principle : Behavior of the luminous reflex in the
pupil of the patient is studied by moving the
illumination across the fundus.
o This behaviour depends on the vergence of the
light rays coming out of the pupil.
o It also depends on the position of the observer.
• Finding 1.
o When the observer is at 1 metre from the patient and if the
rays coming out from the patient's eye form a focus (FP of
the patient) behind the observer at a finite distance or at
infinity or 'beyond infinity' (virtual point behind patient's
retina), then the luminous reflex in the pupil will move in
the same direction of movement of the illumination across
the retina ('With Movement').
o This finding we get in myopia less than 1 D, in emmetropia
and in hypermetropia.
Finding 1.
o The first ray of light entering observer's eye is from
the same edge of the pupil as the first position of
retinal illumination.
o As the illumination on the retina moves towards the
principal axis the light reflex in the pupil also moves in
the same direction.
o The last ray of light entering the observer's eye is
from the other edge of the pupil.
o This gives a with movement reflex in the pupil.
o(As in emmetropia, hypermetropia and myopia less
than 1D - observer at 1 metre from patient.)
• Finding 2.
o When the observer is at 1 metre from the patient
and if the rays coming out from the patient's eye
form a focus (FP) in front of the observer (between
patient and observer) the luminous reflex in the
pupil will move in the opposite direction of
movement of the illumination across the retina
('Against Movement').
o This finding we get in myopia more than 1 D.
Finding 2.
o The first ray of light entering observer's eye is from the opposite edge
of the pupil when the position of the retinal illumination is considered.
(Light rays cross at FP and the diverging rays are entering observer's
eye).
o As the retinal illumination moves towards the principal axis the light
reflex in the pupil moves in the opposite direction.
o The last ray of light entering the observer's eye is from the other edge
of the pupil, this gives an against movement reflex in the pupil. (seen in
myopia more than 1D - observer at 1 metre)
Finding 3.
o When the observer is at 1 meter from the patient
and if the rays coming out from the patient's eye
form a focus (FP) at the nodal point of the
observer then the pupil of the patient will appear
uniformly illuminated.
o The rays coming out through all the parts of
the pupil are focused at the nodal point of
observer's eye.
o By a slight shift of retinal illumination this
focal point is displaced away from observer's
eye making patient's pupil uniformly dark.
• Neutral Point or End Point or Point of Reversal in
Retinoscopy is reached by bringing the FP of
patient's eye to the Nodal Point of observer's eye by
using lenses.
• (except in myopia of 1 D, where it is reached
without any lens).
Steps in Retinoscopic Procedure
1. Set the retinoscope so that the light rays
emanating are parallel.
2. Adjust the pat. In appropriate testing position &
distance.
3. Direct the pat. To look at a specific distant target,
(optotype). If cycloplegia has been used, pat. Can
directly look into the light.
• 4. look through the examiner’s eye piece of the
•
retinoscope & direct the light into the pat.’s
•
pupil.
• - If refraction from the pat.’s pupil is not easy to
•
see then reason are--o Retinoscope bulb can be dim, dirty or turned off.
o The pat. May have very high refractive error.
o The room light may not be sufficiently dim.
o Media opacity.
-Extra reflection can be- Cornea, Trial lens, Extra
light in examining room.
• 5. Streak horizontal – Move up & down.
•
Streak vertical – Move right & left.
6. Note the motion of the reflexAgainst- Add “-” minus lenses in 0.5 diopter
increment until the against movement lost.
With- Add “+” plus lenses in 0.5 diopter until it
becomes difficult to tell the direction of
movement.
• 7. Smaller sweeps are helpful as the reflex band
•
appears widen. When the movement of the
•
reflex fills the pupil and can not be ascertain• - The reflected light rays coming from the eyes
•
are parallel.
• -The lens combination used to reach this point
•
(with the dioptrc equivalent of working distance)
•
is the objective measurement of the refractive
•
error of the eye.
•
- This is referred to as neutrality.
8. Confirmation of neutrality:
If our assessment is correct we will get the following
results–
1. After reaching the neutral point (end point) in
Retinoscopy (with plane mirror) we move slightly towards
the subject, then we will get a ‘with movement’
(because the Far Point is now behind the Observer).
2. If we move slightly away from the subject we will get
an ‘against movement’
(because now the Far Point is between the observer and
the subject).
• 9. Note the power of the lenses used.
•
Substract the dioptric equivalent of working
distance = Refractive error in the axis of
•
sweeping.
•
10. If there is different reflexes from the horizontal
& the vertical orientation of the streak =
Astigmatism.
- Need cylindrical eye glasses.
Determining Cylinder
• Steps to determine the presence of astigmatism:
1. Position the pat. & yourself , illuminate the pat.’s
pupil with retinoscope.
Horizontal – up & down
Vertical – Right & left
2. Compare the intensity & direction of the reflex.
- If both are comparable in intensity & directionAn insignificant Astigmatism is present.
- If streak is brighter in one direction than its in
other, or if the reflex moves in opposite directions
– A cylindrical, or astigmatic, refractive error is
present.
3. Neutralize with a retinoscope.
- If we are using “-” minus cylinder – First neutralize
that is moving slowest or the most “with” the
steak. Then neutralize the reflex, perpendicular to
it.
- If we are using “+” plus cylinder – First neutralize
the reflex that is the most “against” & then
neutralize the one perpendicular to it.
4. Rotate the sleeves of the retinoscope so that the
streak oriented perpendicular to the direction of
the initial orientation.
• - If we are only using spheres for retinoscopy:o Neutralize in one direction & note the power of lens
in that axis.
o Repeat the process in axis 90 to the first, and note
the power of the lens in that axis
o Now add the two sphere powers.
5. If the neutrality can not be achieved with streak
oriented horizontally & vertically, an oblique
astigmatism can be present.
- Adjust the streak acc. to the direction of
movement of reflex & neutralize in the axis of
movement & second at 90 to the axis.
• 6. Note the power of the lens combinations that
used at each axis.
• - In writing the eye glasses orescription in “plus”
cylinder form – Write the power & axis of the least
– plus lens that used to neutralize the reflex.
• - Horizontal streak neutralizes vertical meridian.
• - Vertical streak neutralizes horizontal meridian.
• Say,
o From 1m pat. Need -1.00 D in horizontal direction.
(up & down movement)
o I.e, -2.00 D at 180
Similarly,
o From 1m pat. Need -0.5 D in vertical direction.
(Right & left movement)
o I.e, -1.50 D at 90
So,
o Cylinder = +0.5 D
Therefore,
o Prescription = -2.00 D + 0.50D 90
Automated retinoscopy
o Alternative method, takes less time.
Optical Principle:
1.
2.
o
1.
The Scheiner Principle
The optometer principle
Types - Based on operational method used:
Analysis of image quality: Dioptron, Canon
Autorefractometers, Hoya Autorefractometers.
2. Retinoscopic Scanning: Ophthalmetron, Humphrey
Autorefractor, Nikon 5000 & 7000.
3. Sceiner disc refraction: 6600 Autorefractor, Nidek
&Topcon Autorefractor.
• In next presentation I will discuss Subjective
retinoscopy.
THANK U