Refractive Errors
advertisement

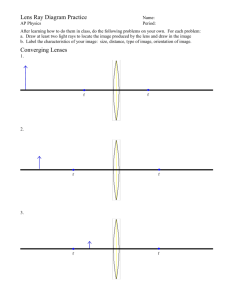
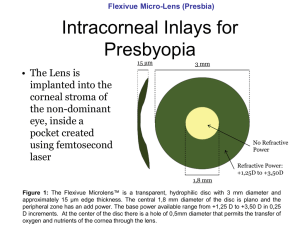
Refractive Errors Dr.Sucharitha Refraction • Def: Method of evaluating the optical state of eye. • Or The process by which the patient is guided through the use of a variety of lenses so as to achieve the best possible acuity on distance and near vision test. • Acc. To the physicist, Refraction is defined as bending of light rays when it passes from one media to other having diff refractive indices. Five Activities 1. 2. 3. 4. 5. Retinoscopy (Objective Refraction) Cycloplegia / Mydriasis Refinement (Subjective Refraction) Binocular Balancing Prescription Of Spectacle Lenses Ophthalmic Optics • Principle of Vergence: • Reciprocal of the distance from the lens to the point of convergence of light. • Divergent: • Light rays that are moving away from each other. • Convergent: • Light rays that are moving towards each other. Parallel rays have zero vergence Convex Lens Identification of a Convex lens: 1. Thick at center, thin at periphery. 2. Object held close to the lens appears magnified. 3. When it is moved, the object seen through it moves in opposite direction to the lens. Image formed by a convex lens: Real, inverted & magnified. Concave Lens Identification of concave lens: 1. Thin at center, thick at periphery. 2. An object seen through it appears minified. 3. When it is moved, the object seen through it moves in the same direction as the lens. Image formed by a concave lens: Virtual, erect and diminished. • Cylinder lens: • Vergence power is in only one meridian, the one perpendicular to the axis of the cylinder. • Spherico- cylinder (Compound lens, Toric lens): o Focus light in two line foci. o The shape of the light rays as they are focused by the spherico-cylinder lens called the-conoid of sturm o Between the two line foci produced by the conoid of sturm is a point called the-Circle of Least Confusion (point of best overall focus for a sphericocylindrical lens. Strum’s Conoid Refractive State of eye • Emmetropia: • Parallel light rays are focused sharply on retina. • Ammetropia: • Unable to bring parallel light rays into focus. • Types: 1. Myopia 2. Hypermetropia 3. Astigmatism Emmetropia o It’s a optically normal eye. o In emmetropic eye, parallel light rays are focused sharply on sensitive layer of retina with the accommodation at rest. What happens to the light rays coming from the FP and entering the eye? o In emmetropia the FP is at infinity. So the rays coming from FP, and entering the eye are parallel. They are focused upon the retina (with accommodation at rest) to give a clear image of object at FP. Hypermetropia • Definition: • Etiology:1. Axial 2. Curvatural 3. Index 4. Positional 5. Absence of lens • Clinical types: 1. Simple 2. Pathological 3. Functional • Components: 1. Total 2. Latent 3. Manifest (facultative/ absolute) • Signs: 1. Size of eye ball 2. Size of cornea 3. AC 4. Fundus • Complications: 1. Recurrence, Stye, Blepharitis, chalazion 2. Convergent squint 3. Amblyopia 4. Glaucoma Myopia • Definition: • Etiology: • Clinical types: 1. Congenital 2. Simple 3. Pathological Pathological Myopia • Etiology: • Genetic Factors General Growth Process more growth of retina Stretching of sclera Increased axial length Degeneration of choroid Degeneration of retina Degeneration of vitreous • Signs: Fundus changes: 1. Myopic crescent 2. Foster fuch’s spots 3. Peripheral degeneration 4. Posterior staphyloma 5. PVD • Complications: 1. RD 2. Complicated cataract 3. Vitreous & Choroidal Haemorrhage RK Astigmatism • Definition: • Types: 1. Regular 2. Irregular • Etiology: 1. Corneal 2. Lenticular 3. retinal • Types: 1. With the rule 2. Against the rule 3. Oblique 4. Bi-Oblique • Clinical Types: 1. Simple 2. compound 3. Mixed Retinoscopy o Objective Refraction o Skiascopy or Shadow test o The goal of retinoscopy is to determine the nature of pat.’s refractive error (if any) and approx. lens power that will diminish (neutralize) that error and approach clear vision. o Types : -Manual -Automated Prerequisites for Manual Retinoscopy 1. Dark room 2. Mydriatic / Cycloplegic 3. Leister’s bulb( 50W / inside Hg, outside black / aperture -1 big, 2 small 2cm) 4. Retinoscope – Priestly – Smith R. - Plane mirror R. - Streak R. 5. Trial Frames / Halberg clip 6. Trial set Commonly used Cycloplegics: Cyclopentolate Hydrochloride (0.5-1%) - Drops applied 2-3 times at 5 minutes interval. - Retinoscopy is done after 30 minutes. - Effect lasts for 8 hours. Tropicamide (0.5-1%) - Drops applied 2-3 times at 5 minutes interval. - Retinoscopy is done after 30 minutes. - Effect lasts for 8 hours Atropine Sulphate (0.5 – 1%): - lower strength below 5 years of age - Used for cycloplegia in children <7–10yrs of age. - In cases with ciliary spasm and in Convergent Strabismus. - Effect lasts for 2 weeks. Homatropine Hydrobromide (1 – 2%) - Drops applied at 15 minutes interval for 6-8 times. - Retinoscopy is done after 1 hour. - Effect lasts for 2 days. Retinoscopes Priestley–Smith retinoscope: o Plane mirror at one end /concave mirror at other end. oHole- 2.5mm ant. ; 4.0mm post.. Fitted with low polar convex lens. oProjects a circle of light in the patient’s pupil. Streak retinoscope o Self illuminating, projects a streak. oWe can rotate the streak in diff angles. Trial Frame Trial Set • Typical “Trial Set” will have:o Spheres - every quarter of a diopter to 4D, every half to 6D, every diopter to 14D, every 2D to 20D. o Cylinder – every quarter of a diopter to 2D. Every half to 6D. o Prism – upto 10 PD, additional 15 & 20 PD. o Plano lenses o Opaque disc o Pin hole o Stenopaeic discs o Maddox rods o Red & Green glasses Principle Of Retinoscopy o Retinoscope illuminates an area of the retina, the image of this area formed at the pat.’s far point. - observer views rays of light emanating from the illuminated retina through pat.’s pupillary area from a working distance. -Depending upon the behavior of reflex the observer knows whether emerging rays are – - Convergent, Divergent or Parallel. o Lenses from the trial set are used to neutralize the movement (neutralization point = subject’s far point coincides observer’s nodal point.) Optics of Retinoscopy o In retinoscopy an illuminated area of retina serves as an object, & the image at the far point of the eye located by moving the illumination across the fundus & noting the behavior of the luminous reflex in the pupil. o The observer does not see the illuminated area of the pat.’s fundus, but only the rays emanating from it to form an illuminated area of the pupil. Working Distance o The distance between the examiner and the patient’s eye is measured and converted to diopter. o Usually, most examiners uses a working distance of a arm length i.e, approx. 66cm / 2/3m / 26 inches. o D=1/f i.e, D=1/2/3 i.e, D=3/2 i.e, D=1.5D o This power is then substracted from the final dioptric amount that is measured. o The working distance must remain constant through out the examination. Far Point o Far Point (FP) is the furthest point at which objects can be seen clearly by the eye. Object kept at FP of the eye can be seen clearly with accommodation at rest. o Position of FP depends on the optical state (static refraction) of the eye. o In emmetropia it is at infinity. o In myopia it is at a finite distance. o In hypermetropia it is a virtual point behind the retina. o If the image is formed between pat. & observerAgainst movement. Seen in- 1. Myopia > 1.5 D o If the image is formed either behind the pat.’s eye or behind the observer’s- With movement. Seen in- 1. Emmetropia 2. Hypermetropia 3. Myopia < 1.5 D o The point of reversal or neutral point of retinoscopy is reached when the subject’s far point coincides with the observer’s nodal point & examiner see a diffuse bright red reflex in the pat.’s pupil & no movement of the reflex is discernible. Retinoscopy Reflex Clues we get from features of retinoscopy reflex - 1. Intensity: In high refractive errors we get a faint reflex and in low refractive errors we get a brighter reflex. 2. Speed: In high refractive error we get a slow movement, and in low refractive error a rapid movement of the reflex. As the neutral point is reached the movement of the reflex is fast. 3. Size: In high refractive error we get a narrow reflex. Reflex will fill the pupil when the neutral point is reached. In very high refractive errors we may not get a reflex or may get a faint reflex with negligible movement. We will not get a good reflex with low power lenses in these cases. So try with high plus or minus lenses Steps in Retinoscopic Procedure 1. Set the retinoscope so that the light rays emanating are parallel. 2. Adjust the pat. In appropriate testing position & distance. 3. Direct the pat. To look at a specific distant target, (optotype). If cycloplegia has been used, pat. Can directly look into the light. • 4. look through the examiner’s eye piece of the • retinoscope & direct the light into the pat.’s • pupil. • - If refraction from the pat.’s pupil is not easy to • see then reason are--o Retinoscope bulb can be dim, dirty or turned off. o The pat. May have very high refractive error. o The room light may not be sufficiently dim. o Media opacity. -Extra reflection can be- Cornea, Trial lens, Extra light in examining room. • 5. Streak horizontal – Move up & down. • Streak vertical – Move right & left. 6. Note the motion of the reflexAgainst- Add “-” minus lenses in 0.5 diopter increment until the against movement lost. With- Add “+” plus lenses in 0.5 diopter until it becomes difficult to tell the direction of movement. • 7. Smaller sweeps are helpful as the reflex band • appears widen. When the movement of the • reflex fills the pupil and can not be ascertain• - The reflected light rays coming from the eyes • are parallel. • -The lens combination used to reach this point • (with the dioptrc equivalent of working distance) • is the objective measurement of the refractive • error of the eye. • - This is referred to as neutrality. 8. Confirmation of neutrality: If our assessment is correct we will get the following results– 1. After reaching the neutral point (end point) in Retinoscopy (with plane mirror) we move slightly towards the subject, then we will get a ‘with movement’ (because the Far Point is now behind the Observer). 2. If we move slightly away from the subject we will get an ‘against movement’ (because now the Far Point is between the observer and the subject). • 9. Note the power of the lenses used. • Substract the dioptric equivalent of working distance = Refractive error in the axis of • sweeping. • 10. If there is different reflexes from the horizontal & the vertical orientation of the streak = Astigmatism. - Need cylindrical eye glasses. Automated retinoscopy o Alternative method, takes less time. Optical Principle: 1. 2. o 1. The Scheiner Principle The optometer principle Types - Based on operational method used: Analysis of image quality: Dioptron, Canon Autorefractometers, Hoya Autorefractometers. 2. Retinoscopic Scanning: Ophthalmetron, Humphrey Autorefractor, Nikon 5000 & 7000. 3. Sceiner disc refraction: 6600 Autorefractor, Nidek &Topcon Autorefractor. THANK U