Powerpoint
advertisement
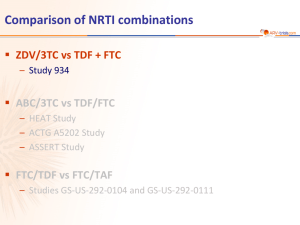
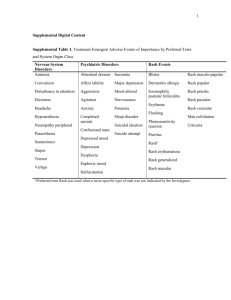
HIV Cases “What to Start” Dr Anton Pozniak Chelsea and Westminster Hospital London Case-SP • A 57 year old caucasian man presented to the emergency department with progressive difficulty in swallowing over the last 4 weeks. • He is hypertensive and has diet controlled diabetes and asthma and takes inhaled B2 agonists and inhaled steroids • He had seen his family practitioner who saw oral thrush and thought it was related to his diabetes/ inhalers and gave him amphotericin lozenges • He had been diagnosed with HIV a year before but had not attended any clinics as he “felt well” Case-SP • He had extensive oral thrush and had severe dysphagia • BP 145/90 mmHg • He was admitted and treated with fluconazole • Social History – Lives alone is MSM – Smokes 15 a day – Alcohol 20 units a week, no recreational drugs • Drugs – – – – Salbutamol inhaler Fluticasone Inhaler Amlodopine St Johns Wort for depression Case-SP • • • • • • • • • • • Labs STD screen negative FBC,U and Es, LFTs Normal , Cr CL 69 mls/min, Urine protein +no glucose CD4 33 cells/uL VL 365000 copies/ml Hep B immune Hep C negative STS negative Resistance test and HLA B5701 awaited Framingham 10 year risk risk 18% You decide to start ARVs DHHS[1] IAS[2] EACS[3] EFV/TDF/FTC Preferred Recommended Recommended ATV/RTV + TDF/FTC Preferred Recommended Recommended DRV/RTV + TDF/FTC Preferred Recommended Recommended RAL + TDF/FTC Preferred Recommended Recommended LPV/RTV + TDF/FTC Alternative Alternative Recommended EFV + ABC/3TC Alternative Alternative Recommended ATV/RTV + ABC/3TC Alternative Alternative Recommended DRV/RTV + ABC/3TC Alternative Alternative Recommended NVP + TDF /FTC Acceptable Alternative Recommended MVC + TDF/FTC Acceptable Alternative Alternative RPV + TDF /FTC Alternative No recommendation No recommendation RAL + ABC/3TC Alternative No recommendation No recommendation Regimen 1. DHHS Guidelines, March 2012. 2. T. JAMA. 2012;304:321-333. 3. EACS Guidelines, November 2011. You decide to start ARVs What is your choice of main agent? • NNRTI • PI/r • Integrase • other Difficulties in choosing-which 3rd agent? • NNRTI– may have transmitted dug resistance – RPV may not be effective in High viral load • Integrase – BD – and may have NRTI transmitted dug resistance • PI/r – drug interactions, – diabetes, lipids NNRTI/NRTI and Prevalence of Transmitted Drug Resistance 12% 10% prevalence of mutations 8.9% 8% 6% 5.0% 4% 2.9% 2.5% 2% 0.8% 0.4% 0% Any class Eacs 2011 SPREAD NRTI NNRTI PI Multi Drug Multi Drug Restistance (2 Resistance (3 classes) classes) If you decide to give a boosted PI Drug Interactions • What Drugs have significant interactions with a boosted PI? 1 St Johns Wort 2 Fluticasone 3 Amlodopine 4 None 5 all What NRTI back bone? • • • • • AZT/3TC ABC/3TC TDF/FTC DDI/3TC OTHER Difficulties in choice of NRTI • AZT– lipodystrophy – BD • ABC – High Viral load – Cardiovascular risk(smoker and diabetic and BP) • TDF – Renal changes, – Bone changes 1.9 1.5 1.5 1.2 1.2 ** 1.0 1.0 0.8 0.6 # PYFU: # MI: RR of cumulative exposure/year 95%CI NRTI 1.9 0.8 ZDV ddI 138,109 523 74,407 331 ddC 29,676 148 d4T 95,320 405 3TC ABC TDF 152,009 554 53,300 221 39,157 139 PI† 1.2 RR of cumulative exposure/year 95%CI RR of recent* exposure yes/no 95%CI CVD – Do drugs matter? D:A:D: Recent and/or cumulative ARV exposure and risk of MI 0.6 NNRTI 1.13 1.1 1.0 0.9 # PYFU: # MI: IDV 68,469 298 NFV 56,529 197 LPV/RTV 37,136 150 SQV 44,657 221 NVP 61,855 228 EFV 58,946 221 *Current or within past 6 months; †Approximate test for heterogeneity: p=0.02; **not shown due to low number of patients receiving ddC CVD=cardiovascular disease; ARV=antiretroviral; MI=myocardial infarction; RR=relative risk; NRTI=nucleoside reverse transcriptase inhibitor; PI=protease inhibitor; NNRTI=nonnucleoside reverse transcriptase inhibitor; PYFU=patient years of follow up Adapted from Lundgren JD, et al. CROI 2009. Oral presentation 44LB. CVD: Do drugs matter? FDA meta-analysis of abacavir and MI • • Meta-analysis of Phase II–IV RCTs including ABC – Mean follow up 1.6 person-years per subject – Patients: 80% male (mean age=39 years) Limitations – Young adults, so underlying MI risk low – Other CV risk factors usually unknown – Unvalidated MIs – Some studies had a PI control group CVD=cardiovascular disease; FDA=Food and Drug Administration; MI=myocardial infarction; RCTs=randomised controlled trials; CV=cardiovascular; PI=protease inhibitor Created from Ding X, et al. CROI 2011. Poster presentation 808. Mantel-Haenszel Risk Difference % (95% CI) Academic Trials n=5 -0.53 NIH Trials n=5 0.31 -0.45 GSK Trials n=16 -0.43 All Trials n=26 -0.8 0.03 -0.11 -0.26 0.008 -0.4 0 1.16 0.51 0.21 0.27 0.4 0.8 1.2 Chronic renal disease: ART risk factors • 6,843 patients (5,136 male), median age 43 yrs, 90.1% exposed to cART, CD4 450 cells/mm3, 21.7% hypertension, 4.9% diabetes • Median follow up 3.7 years • 2-fold increased risk if hepatitis C RNA+ Incidence: 1.05 (0.91–1.18)/100 PYFU Multivariate analysis IRR/ year p Tenofovir 1.16 <0.0001 Indinavir 1.12 <0.0001 Atazanavir 1.21 0.0003 Lopinavir/r 1.08 0.030 Months ART=antiretroviral therapy; PYFU=patient years follow up; IRR=incidence rate ratio Adapted from Mocroft A, et al. AIDS. 2010;24:1667–8. Low bone density/fracture: Relationship to ART ACTG 5224 & SMART: BMD loss with ART initiation ~2-4% at 1-2 yrs1 NNRTI/PI Component Secondary Analysis EFV ATV/rtv 0 0 TDF/FTC ABC/3TC p=.004* p=.035* -4 -4 -3 -3 -2 -2 -1 -1 p=.004* -5 -5 Spine BMD percent change from week 0 NRTI Component Primary Analysis 0 No. of subjects TDF/FTC 128 ABC/3TC 130 24 111 122 96 144 48 Visit Week from Randomization 105 106 97 101 87 80 192 53 53 0 No. of subjects EFV 133 ATV/rtv 125 24 48 96 144 117 116 109 102 107 91 86 81 * - two-sample t-test No significant interaction of NRTI and NNRTI/PI components (p=0.63) ART=antiretroviral therapy; BMD=bone mineral density; DC=drug conservation; VS=viral suppression; NRTI=nucleoside reverse transcriptase inhibitor; NNRTI=nonnucleoside reverse transcriptase inhibitor; PI=protease inhibitor; DXA=dual-energy X-ray absorptiometry 1. Adapted from McComsey G, et al. JID. 2011;203:1791–801. 192 Visit Week from Randomization 58 48 Case-SP • Resistance was wild type • He starts EFV TDF FTC Case AP • • • • • 35 year old Asian women presents with Night sweats, weight loss and cough CXR - RUL cavity and infiltrates AAFB - smear positive and started on RZHE Had an HIV test and was positive CD4 was 35 cells/uL Case AP • As her CD4 was<50 cells/uL she was offered ARVs within 2 weeks of starting and tolerating her TB meds What ARV combination would you offer her? What is your choice of main agent? • • • • NNRTI-Efavirenz PI/r-Lopinavir/r Integrase-Raltegravir other Case AP • Started Efavirenz but couldn't tolerate it • What would you offer her? • • • • NNRTI-Nevirapine PI/r-Lopinavir/r Integrase-Raltegravir other Case AP • What would you offer her? • NNRTI-Nevirapine-less efficacy ? Drug interaction • PI/r-Lopinavir/r major interaction with rifampicin so switch to rifabutin or double dose lopinavir/r or high dose ritonavir 400mg bd • Integrase-Raltegravir 400 or 800mg bd • Other-4 nucleosides