post CABG Myocardial Infarction
advertisement

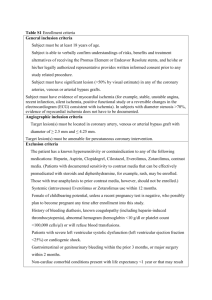
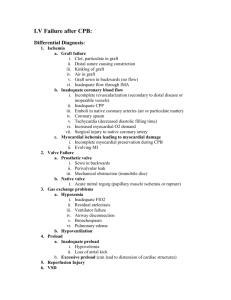
Susana G. Garcia MD Review the current definition, risk factors, clinical impact and incidence of PMI Describe the different clinical presentation of PMI and how this dictate the goal and approach to diagnosis and treatment of PMI Describe the use and limitation of different diagnostic tools in the evaluation of perioperative ischemia and infarction Present current data on novel diagnostic tools and therapies used in PMI Present algorithmic approach to post CABG patients with signs of ongoing ischemia Discuss the recent guideline on: Resuscitation of cardiac arrest after cardiac surgery Mechanical Circulatory Support Mgt of Early Graft Failure “ an increase in biomarker values to > 5x the URL during the first 72 h ff CABG, when associated with: the appearance of new pathological Q-waves or new LBBB or angiographically documented new graft or native coronary artery occlusion or imaging evidence of new loss of viable myocardium” Age >70 years (ESC) Female gender Renal Failure Diabetes Peripheral artery disease Emergency CABG Repeat CABG Preop MI Preop Ischemia Cardiomegaly Diastolic dysfunction Prior MI Use of nsaid No bb , no statin, no asa Severe LVdysfsn(EF<35%) or cardiogenic shock Long CPB time CABG combined with other surgery Intraop ischemia Surgical technique Inadequate protection High Hct (Spiess B. D. et al.; J Thorac Cardiovasc Surg 1998;116:460-46) Rapid arrhythmias Hypertension Hypotension Tachycardia from Volume depletion Blood loss Inotropes. Pressores Pain PMI is associated with adverse outcome Available data suggests a direct correlation between : the amount of myonecrosis the likelihood of reduced survival Because of the wide variability in the definitions used, the incidence of reported MI is highly variable Incidence= of 2–40% is not straightforward In the early period the critical issue is : to determine whether there is acute severe ischemia/infarction due to Early Graft Failure Acute Native Coronary Thrombosis that warrants urgent intervention. Subclinical Enzyme Leak Persistent Signs of Ischemia -Hemodynamically Sable Persistent Signs of Ischemia-Hemodynamically Unstable Cardiogenic Shock /Cardiac Arrest Some degree of myocardial injury virtually always occurs after CABG At one end of the spectrum, the myocardial injury is manifested as a small troponin release with no clinical sequelae Troponin release may be from: Myocardial trauma Imperfect myocardial protection Subclinical Enzyme Leak Persistent Signs of Ischemia -Hemodynamically Sable Persistent Signs of Ischemia-Hemodynamically Unstable Cardiogenic Shock /Cardiac Arrest At the other end of the spectrum, is severe myocardial ischemia or infarction that is associated with hypotension, LCOS and ventricular arrhythmias This latter situation demands urgent investigation because it may represent an acute obstruction of a coronary graft or native coronary vessel Timely intervention may be life saving To search for signs of ischemia/infarction which may be due to Early Graft Failure Acute Native Coronary Thrombosis that warrants urgent intervention. Angina (not reliable): Pain from myocardial ischemia is very difficult to distinguish from wound pain Most are sedated and ventilated during the early post op period Cannot report symptoms Hemodynamic Instability: Has many causes But one important to consider is ischemia Hemodynamic Instability Acute ischemia of severity sufficient to cause hypotension or low cardiac output state : implies a large region of threatened myocardium warrants urgent intervention and treatment Swan Ganz Catheter Measurements suggestive of LCOS Increased in PA pressure Increased PCWP Low CO New significant Q waves ST segment depression ≥ 0.04 second duration in any two leads except III and aVR may be indicative of full-thickness MI but they take 24 to 48 hours to develop therefore not useful in the assessment of suspected ischemia ≥ 1 mm, measured 0.06 sec after the J point if it occurs, develops concurrently with myocardial ischemia. ST segment elevation, with the subsequent new Q waves after CABG surgery may provide a useful marker of acute ischemia. Diffuse upsloping ST elevation New LBBB or AV block Pericarditis do not mply ischemia. may indicate acute ischemia, but they too are common following cardiac surgery. Recurrent Ventricular Tachycardia strongly suggestive of severe acute ischemia. Despite the limitations of ECG analysis, the finding of ST segment depression or elevation that is limited to a specific coronary territory + hemodynamic instability / ventricular arrhythmias is strongly suggestive of acute ischemia. All patients with suspected myocardial ischemia after CABG surgery should undergo urgent echocardiograms —preferably a transesophageal echocardiogram examination looking SWMAs SWMAs are more sensitive and specific for myocardial ischemia than ECG changes but they can be difficult to interpret in postoperative patients. Troponin I a value > 20 μg/l is associated with prolonged hospital stay indicative of early graft failure Salamonsen RF,. Clin Chem 2005; 51:40-46. Troponin T a value > 1.58 μg/l at 18 to 24 hours after surgery is predictive of adverse outcome, including death. Januzzi JL. J Am Coll Cardiol 2002; 39:1518-1523. A limitation of making judgments based on troponins is that peak levels occur at about 24 hours after an ischemic event Troponin T peaks a little later than troponin I Thus, these markers are not ideal for the evaluation of acute ischemia soon after surgery. CKMB is less sensitive and specific than the troponins takes nearly 24 hours to reach peak levels. Myoglobin levels peak within 6 to 12 hours of ischemic injury but are poorly predictive of outcome. Costa MA(ARTS trial). Circulation 2001; 104:2689-2693. cTnI elevation after CABG discriminates patients: with graft-related PMI non-graft-related PMI without PMI however, not earlier than 12 h after surgery. This detection window is far too long to enable timely rescue strategies Reported to detect ischemia within the first 30 minutes: Heart type fatty acid binding protein(hFABP) Ischemia Modified Albumin May enable early intervention aimed at restoring myocardial flow If ischemia is suspected on the basis of hemodynamic instability or ECG changes urgent transesophageal Hypotensive: / Signs of Ongoing Ischemia by ECG Initiate Mgt for Arrhythmia, Ischemia. LCOS Tamponade /Hemodynamic Deterioration +/- Ischemia TEE No Tamponade: +Acute Ischemia Intensify Tx of Spasm + Optimize Filling Pressure; Inotropic Support; IABP Re-exploration : Revision of Graft / Evacuation of Clot or Hematoma; Ligation of Bleeders No response Urgent Coronary Angiography PCI vs Surgical depending on anatomy 2010 ESC Guideline in Myocardial Revasc If ischemia is suspected on the basis of hemodynamic instability or ECG changes urgent transesophageal Hypotensive: / Signs of Ongoing Ischemia by ECG Initiate Mgt for Arrhythmia, Ischemia. LCOS Tamponade /Hemodynamic Deterioration +/- Ischemia TEE No Tamponade: +Acute Ischemia Intensify Tx of Spasm + Optimize Filling Pressure; Inotropic Support; IABP Re-exploration : Revision of Graft / Evacuation of Clot or Hematoma; Ligation of Bleeders No response Urgent Coronary Angiography PCI vs Surgical depending on anatomy Class I Recommendations to reduce the risk of perioperative myocardial ischemia and infarction, management targeted at optimizing the determinants of coronary arterial perfusion heart rate diastolic or mean arterial pressure, and right ventricular or LV end-diastolic pressure is recommended (Level of Evidence: B) 2011 ACC AHA CABG Guideline Intraoperative TEE PA Cath ECG Intraoperative Graft Assessment TEE : useful for evaluation of LVEDA/LVEDV EF and CO LVEDP Valve Function PHTN Shunts Complications Ischemia ( New RWMA) guide surgical therapy lead to revison of failed conduit placement of additional grafts not originally planned Potentially superiority over Swan PCWP or PADP in assessment of LVEDP in the early post op period Fontes ML, Bellows W, Ngo L, et al. Assessment of ventricular function in critically ill patients: limitations of PAC J Cardiothorac Vasc Anesth. 1999;13:521–7. Live 3DTEE Time to minimal regional volumes normal subject synchronous in a heart failure patient dispersed Translational Research Volume 159, Number 3 Doppler Tissue Imaging Real Time 3D TEE Speckle Tracking Cost effectiveness has not been determined Too complex for routine use Graft patency strongly influences early and late outcomes after CABG. Transit Time Flow Measurement quantitative volume flow technique, cannot define the degree of graft stenosis A randomized comparison of intraoperative ICG angiography and transit-time flow measurement to detect technical errors in coronary bypass grafts Journal of Thoracic and Cardiovascular Surgery,Volume 132, Issue 3, September 2006, Pages 585-594 Nimesh D. Desai LIMA Anastomosis LAD Diagnostic accuracy for detecting clinically significant graft failure ICG > Transit-time US flow measurement. LIMA Anastomosis High inter-rater reliability for graft patency between surgeons. For graft stenosis >50% Sn=100% Sp=100% LAD Desai JACC Vol 46, Issue 8, 18 Oct 2005, pp 1521-25 has the capability of serving both as: a complete surgical OR a cath laboratory. It allows for routine completion angiogram following CABG surgery identifies abnormal grafts, providing the opportunity to revise them with PCI surgery before leaving the OR. Semin Thorac Cardiovasc Surg 21:207-212 The Graft Imaging to Improve Patency (GRIIP) clinical trial results The Journal of Thoracic and Cardiovascular Surgery, Volume 139, Issue 2, February 2010, Pages 294-301.e1 * Steve K. Singh, MD, MS Is Routine intraoperative graft assessment safe? Does it lead to a marked reduction in graft occlusion 1 year after CABG? Yes No Subclinical Enzyme Leak Persistent Signs of Ischemia -Hemodynamically Sable ✓✓Persistent Signs of Ischemia-Hemodynamically Unstable Cardiogenic Shock /Cardiac Arrest Incidence 0.7-2.9% Potentially reversible If treated promptly has a high survival rate 54-79% Key to successful resuscitation Early resternotomy esp if + tamponade (external chest compression not effective) Cardiac Arrest Activate Surgical Team for Emergency Resternotomy Resuscitation based on 2010 ACC AHA or ESC CPR Guideline following Cardiac Surgery Initial Stabilization Hemodynamically Unstable TEE: + tamponade Early Resternotomy + Resumption of CPB TEE : No Tamponade + new Ischemia Coronary Angiography PCI vs Resternotomy depending on findings External chest compression should be started immediately in all patients who collapse without a pulse Correct reversible cause (K, volume, bleeding, O2, acidosis, ischemia) During CPR… IABP changed to pressure trigger If unable to attain SBP of at least 80mmHg with effective compression: may indicate tamponade Do early resternotomy 3 quick defibrillation 3 failed shocks Emergency Resternotomy Further defibrillation as indicated should be performed with internal paddles at 20 joules after resternotomy Amiodarone 300mg after 3rd failed defibrillation attempt (but don’t delay resternotomy) Correction of Ischemia, rather than giving Amiodarone, is more likely to achieve myocardial stability” An integral part of resuscitation after cardiac surgery Improved survival and QOL are well documented with rapid sternotomy Should be standard part of resuscitaton within 10 days after cardiac surgery Survival to discharge 3256%when CPB is reinstituted in the ICU Survival rates decline rapidly when procedure delayed for >24 hrs Indications: correct surgical bleeding Repair graft occlusion Rest myocardium Cardiac Arrest Activate Surgical Team for Emergency Resternotomy Resuscitation based on 2010 ACC AHA or ESC CPR Guideline following Cardiac Surgery Initial Stabilization Hemodynamically Unstable TEE: + tamponade + Acute Ischemia Early Resternotomy + Resumption of CPB Coronary Angiography Graft Revision / Evacuation of Effusion Hemodynamic Stability TEE : No Tamponade/Hypovolemia Unstable PCI vs Resternotomy depending on findings Optimal treatment demands the ff to prevent end organ failure and death: Hemodynamic support (improve systemic perfusion) Pharmacologic Mechanical Invasive hemodynamic monitoring Early Reperfusion 2010 ESC/EACTS Myocardial Revascularization Guideline 2009 ACC/AHA Guideline focused update on Heart Failure ECMO Used for cardiac arrest refractory to standard resuscitation measures 9 case series have reported improved survival after cardiac surgery Recommendation: “In post cardiac surgery patients who are refractory to standard resuscitation procedure, mechanical circulatory support ( ECMO and CPB) may be effective in improving outcome” (Class IIb,LOE B) 2010 AHA Guideline for CPR and ECC IABP in Perioperative Myocardial Dysfunction 2011 ACCF AHA CABG Guideline: Class II a (LOE B) In the absence of severe PAD, the insertion of IABP is reasonable to reduce mortality in CABG patients who are considered to be at high risk Undergoing reoperation LVEF<30% Left Main Disease Cardiac Arrest Activate Surgical Team for Emergency Resternotomy Hemodynamically Unstable Resuscitation based on 2010 ACC AHA or ESC CPR Guideline following Cardiac Surgery TEE: + tamponade + Acute Ischemia Early Resternotomy + Resumption of CPB Coronary Angiography Graft Revision / Evacuation of Effusion Hemodynamic Stability Initial Stabilization TEE : No Tamponade/Hypovolemi a Unstable Consider ECMO PCI vs Resternotomy depending on findings Usually have uneventful postoperative course but are at increased risk for adverse events and should be kept in a highly monitored environment (ICU) during their early postoperative periods. Prior to discharge to the ward, such patients should be medically optimized with: β blockers ACE inhibitors antiplatelet agents (aspirin ± clopidogrel), statins. Prevention of Perioperative Myocardial Injury BB should not be stopped to avoid acute ischemia Avoid NSAIDS Resumption of ASA 6 hours post op Complete Revasc Arterial Grafting to LAD Graft flow measurement /evaluation (Class 1C) Graft flow <20mL/min and PI >5 mandate graft revision Volatile Anesthetics protective in the setting of myocardial ischemia and reperfusion 2010 ESC/ EACTS Myocardial Revasc Guideline ✓✓Subclinical Enzyme Leak Persistent Signs of Ischemia -Hemodynamically Sable ✓✓Persistent Signs of Ischemia-Hemodynamically Unstable ✓✓Cardiogenic Shock /Cardiac Arrest Usually non-graft related Poor Myocardial Protection Inadequate cardioplegic perfusion Coronary Air Incomplete revascularization Global Ischemic Reperfusion Injury (IRI) induced by: Aortic cross-clamping and de-clamping SIRS from CPB Distal microembolization Surgical Manipulation of the Heart Genetic susceptibility to acute IRI Sometimes Graft Related Suboptimal graft flow Spasm Failure Goals: 1. 2. Is there recent infarction? If yes, Risk stratification to determine need for early vs conservative mgt • • • • Cardiac Enzymes ECG Non-invasive Imaging Role of MRI used to detect, characterize, and quantify PMI during CABG surgery. Helps in risk stratification in hemodynamically stable patients Electrocardiograms changes are difficult to interpret following surgery unless there is the appearance of a new Q-wave MI Echocardiography New RWMA which represent myocardial stunning rather PMI To predict graft failure :Sn=20% Sp=25% Myocardial nuclear scanning only detect obvious perfusion defects arising from graft or native coronary artery occlusion will not detect diffuse PMI Can be used to detect new loss of viable myocardium post-CABG surgery can therefore be used to detect perioperative MI. Delayed gadolinium contrast enhancement by cardiac MRI (DE-CMR) gold-standard imaging technique for visualizing myocardial fibrosis or infarction. Can also characterize, and quantify PMI. provide clues to the underlying aetiology of myocardial injury. three patterns of DE-MRI have been described: (i) a transmural MI in a coronary artery territory: early graft or native coronary artery occlusion (ii) a sub-endocardial MI: distal coronary embolization (iii) diffuse patchy areas of myocardial necrosis: acute global IRI or other causes. Pegg TJ, et al. A randomized trial of on-pump beating heart and conventional cardioplegic arrest in CABG patients with impaired LV function using CMRI and biochemical markers. Circulation 2008;118:2130–2138. “the presence of ne PMI on CMR following either CABG or PCI was associated with a 3.1-fold increase MACE Reduced event free survival Rahimi K et al Prognostic value of coronary revascularisation-related myocardial injury: a cardiac MRI study. Heart 2009;95:1937–1943. Preoperative MRI scan in short axis plane in a 76yo DM patient with dyspnoea. underwent CABG for 3VD Postoperative MRI short axis (B) Showed new inferior and infero-septal hyperenhancement (white arrow). He died of heart failure 12 months after Rahimi K et al Prognostic value of coronary revascularisation-related myocardial injury: a cardiac MRI study. Heart 2009;95:1937–1943. “MR examination of patients with sternal wires is generally considered to be safe.” Circulation. 2007; 116: 2878-2891 From the Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Council on Cardiovascular Radiology and Intervention: Glenn N. Levine MD, FAHA; P - post CABG PMI pts I - Acadesine infusion O - reduced Severity of PMI from IRI mortality rate after 2 yrs of ff up M - RCT Post-Reperfusion MI Long-Term Survival Improvement Using Adenosine Regulation With Acadesine Dennis T. Mangano, etal ,J Am Coll Cardiol 2006;48:206 –14 Hemodynamically Stable: with ECG changes suggest Ischemia or Infarct (new LBBB or Q wave) Biomarker Rise >/= 5x the URL (use rapid assay point of care test) Biomarker Rise <5x the URL (use rapid assay, point of care test) TTE Repeat after 8 hours Equivocal Cardiac MR or Nuclear MPI Confirms acute global IRI Consider Acadesine Infusion confirms early graft or native coronary artery occlusion Confirmed Ongoing Ischemia: New wall motion abnormality with large area of myocardium at risk+ worse LV fxn Biomarker rise <5x URL Coronary Angiography Repeat in 4 hours PCI vs Resternotomy for graft revision depending on findings Biomarker <5x URL Maximize Ischemic nd Post MI Regimen:+Early Antiplatelet and Statin Therapy Factors to Consider Hemodynamically unstable Concomittant tamponade or bleeder Unsuitable Vessels for PCI (High Syntax Score) Number of Occluded Bypass Grafts Available IMA for grafting totally occluded vessels Good Distal Targets 2011 ACCF AHA SCAI PCI Guideline Hemodynamically stable Limited areas of Ischemia Patent graft to LAD Suitable PCI targets (low syntax score) Mechanism of graft closure can be fixed by PCI Kinking Thrombosis Anastomotic stenosis Co-morbid conditions (High Euro or STS score) Increased risk of distal embolization MI and no reflow PCI of de novo SVG stenosis High risk bec: Atheroma is friable embolization GPI- less effective for SVG than native arteries Combined data support use of distal embolic protective device during SVG PCI (Class I-A) Class II a ; LOE B Hybrid coronary revascularization (defined as the planned combination of LIMA-LAD artery grafting and PCI of >/=1 non LAD coronary arteries) is reasonable in patients with 1 or more of the ff: Limitation to traditional CABG Heavily calcified prox aorta Poor target vessels for CABG (but amenable for PCI) Lack of suitable graft conduits Unfavorable LAD artery for PCI excessive vessel tortuosity or CTO 2011 ACCF AHA SCAI PCI Guideline Perioperative MI is associated with adverse short and long term clinical outcome PMI may present as asymptomatic enzyme leak to cardiogenic shock Goals of therapy depends on clinical presentation Early detection and intervention of graft failure is key to restore myocardial flow and prevent consequences of PMI Latest guideline recommends : PCI > Redo CABG in the mgt of graft failure heart team approach in the determining the optimal definitive mgt of graft failure Post CABG with Signs of Ongoing Ischemia Hymodynamically Unstable: Cardiac Arrest/Shock VT/VF,New Q/LBBB, ST, LCOS Hemodynamically Stable: With Signs of Ongoing Ischemia Without Signs of Ongoing Ischemia Vary depending on initial presentation the critical issue is : to determine whether there is acute severe ischemia/infarction due to Early Graft Failure Acute Native Coronary Thrombosis that warrants urgent intervention. Patients presenting with hemodynamic instability or signs of ischemia are more likely to have graft failure and warrant early intervention to save viable myocardium and reduce post op mortality risk Post CABG with Signs of Ongoing Ischemia Hymodynamically Unstable: Cardiac Arrest /Shock VT/VF, ST, LCOS Hemodynamically Stable: With Signs of Ongoing Ischemia Without Signs of Ongoing Ischemia Post CABG with Signs of Ongoing Ischemia Hymodynamically Unstable: Cardiac Arrest/Shock VT/VF, ST, New Q wave/ LBBB LCOS Hemodynamically Stable: With Signs of Ongoing Ischemia Without Signs of Ongoing Ischemia Urgent TEE to : Confirm ongoing ischemia Rule out Tamponade Hypotensive: with Signs of Ongoing Ischemia Mgt of ischemia Nitrates Optimize O2 Transfusion TEE arrhythmia LCOS Optimiize filling pressures Inotropic support IABP Tamponade /Hemodynamic Deterioration Re-exploration : Revision fo Graft / Evacuation of Clot or Hematoma; Ligation of Bleeders No Tamponade: Large area of myocardium at Risk/ Some Response to Conservative Mgt Aggressive Tx of Spasm + Urgent Coronary Angiography PCI vs Surgical vs Hybrid depending on anatomy CLASS I Intraoperative TEE should be performed for evaluation of acute, persistent and life-threatening hemodynamic disturbances that have not responded to treatment LOE B CLASS II Intraoperative TEE is reasonable for monitoring of hemodynamic status, ventricular fxn and RWMA and valvular fxn in patients undergoing cabg LOE B What’s the role of Hybrid Revascularization? Defined as planned combination of LIMA-to – LAD artery grafting and PCI of >/=1 non LAD coronary arteries Intended to combine the advantages of CABG ( durability of LIMA graft) and PCI May be performed in a hybrid suite in one operative setting or as a staged procedure Class II a ; LOE B Hybrid coronary revascularization (defined as the planned combination of LIMA-LAD artery grafting and PCI of >/=1 non LAD coronary arteries) is reasonable in patients with 1 or more of the ff: Limitation to traditional CABG Heavily calcified prox aorta Poor target vessels for CABG (but amenable for PCI) Lack of suitable graft conduits Unfavorable LAD artery for PCI excessive vessel tortuosity or CTO