20110404092025_bbp
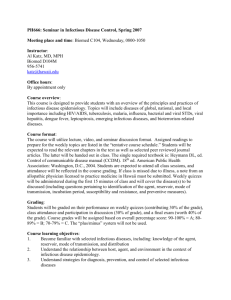
advertisement

MIEMSS INFECTIOUS DISEASE PREVENTION Saving the Lives of Our Providers 1 Infectious Disease Prevention Awareness Prevention General infection control principles and practices Specific diseases Immunizations Infectious disease laws & guidelines Notification laws MAIS run report Infection control plan Designated infection control officer 2 Infectious Disease Prevention Public health concern 45 40 35 Health care providers 30 AIDS HBV HCV TB 25 20 15 Understanding 10 5 0 1992 1993 1994 1995 CASES PER 100,000 POPULATION 3 Infectious Disease Prevention Routes of Transmission: • • • • • Direct contact Indirect contact Droplet contact Airborne transmission Common vehicle transmission 4 Infectious Disease Prevention Infectious Agent Susceptible Host Means of Entry Reservoir Means of Exit Mode of Transmission Chain of Infection 5 Infectious Disease Prevention Bloodborne Pathogen OSHA / MOSH Update • Occupational Safety and Health Act MOSH 09.12.31 Maryland • OSHA Standard 29 CFR 1910.1030 6 Infectious Disease Prevention Make sure your department has an accessible copy of the Bloodborne Pathogen Standard 29 CFR 1910.1030 7 Infectious Disease Prevention Develop a general understanding of the epidemiology & symptoms of bloodborne pathogens 8 Infectious Disease Prevention Bloodborne Pathogens • microorganisms that can cause disease in humans • can be transmitted from one person to another Exposure occurs through broken skin: percutaneous or through a mucous membrane: mucocutaneous 9 Infectious Disease Prevention Bloodborne Pathogens of Special Concern To Health Care Providers • • • • HBV: Hepatitis B virus HCV: Hepatitis C virus Other emerging viral hepatitis HIV: Human Immunodeficiency virus 10 Infectious Disease Prevention Hepatitis B (HBV) • Infection of liver caused by HBV • Virus is in blood and other body fluids • Spread by exposure to blood and body fluids • Some people are at higher risk of HBV 11 Infectious Disease Prevention Hepatitis B (HBV) Symptoms: Tiredness Loss of appetite Fever Vomiting Yellow skin & eyes (jaundice) Dark-colored urine. Light colored stool 12 Infectious Disease Prevention HBV Treatment No cure Fluids Rest Right diet Avoid alcohol & some medicines 13 Infectious Disease Prevention Hepatitis B Prevention Avoid exposure Get complete vaccination series 14 Infectious Disease Prevention Hepatitis C (HCV) Infection of the liver Virus is in blood and other body fluid HCV mainly spread by exposure to blood and blood products Certain people are at higher risk of getting HCV 15 Infectious Disease Prevention Hepatitis C (HCV) Symptoms: Tiredness Loss of appetite Abdominal pain Nausea Vomiting Yellow skin & eyes (jaundice) Urine that is dark in color 16 Infectious Disease Prevention Hepatitis C (HCV) Treatment No cure Treatment limited Rest & fluids Avoid alcohol & some medicines 17 Infectious Disease Prevention Hepatitis C (HCV) Prevention Avoid exposure No vaccine 18 Infectious Disease Prevention Human Immunodeficiency Virus (HIV) AIDS is caused by the HIV virus Some people at higher risk than others HIV is in blood and other body fluids HIV is spread by exposure to HIV infected blood and HIV infected body fluids 19 Infectious Disease Prevention AIDS annual rates per 100,000 population United States, January - December 1996 4.0 14.5 3.9 MD. 44.4 6.1 26.6 D.C. 232.3 12..0 30.1 25.3 50.9 13.4 14.2 20 Infectious Disease Prevention HIV Certain symptoms & conditions may be associated with HIV/AIDS Fever Weight loss Swollen lymph nodes White patches in mouth (thrush) Certain cancers eg. Kaposi’s sarcoma, certain lymphomas Infections eg. pneumocystis pneumonia, TB, etc. 21 Infectious Disease Prevention HIV A blood test may tell if you have HIV infection or AIDS HIV treatment No cure Treatment includes drug “cocktails” Combination therapy with a variety of medications help people with HIV by slowing the disease process 22 Infectious Disease Prevention HIV and AIDS are Preventable There is NO vaccine however Avoid exposure Follow standard (universal precautions) such as the use of: gloves, eye protection, gowns, etc. 23 Infectious Disease Prevention Transmission of Bloodborne Pathogens Percutaneous: through the skin Mucocutaneous: through a mucous membrane 24 Infectious Disease Prevention Chain of Infection Infectious Agent Reservoir Means of Exit Mode of Transmission Means of Entry Susceptible Host 25 Infectious Disease Prevention Local Exposure Control Plan How can each member get a copy? 26 Infectious Disease Prevention Identify tasks and other activities that may involve exposure to blood or other potentially infectious body materials 27 Infectious Disease Prevention Patient assessment Airway management Assisting respirations Bleeding control Contact with body fluids Clean-up of scene & equipment Establishing an IV Emergency childbirth Other patient care activities where contact with blood or body fluids occur 28 Infectious Disease Prevention Methods that will prevent or reduce exposure include: Engineering controls Work practices Personal protective equipment 29 Infectious Disease Prevention Engineering Controls That Help Prevent Contact With Blood & Body Fluids Include: Isolation supplies Hand washing facilities Waterless hand cleaners Sharps containers Ventilation Medical waste containers Self sheathing needles or needleless systems 30 Infectious Disease Prevention Work Practice Controls Include: Washing hands Prohibited in work areas (ambulance) • Eating, drinking, smoking, applying cosmetics or lip balm, handling contact lenses Never bend, break or recap needles Avoid causing splashes and splatters of blood or body fluids Properly handle contaminated items 31 Infectious Disease Prevention Personal Protective Equipment (PPE) must be used when in contact with blood or other body fluids. Examples include: Gloves Gowns Face shields or masks Eye protection Mouth pieces or pocket masks Disposable resuscitation bags Lab coats 32 Infectious Disease Prevention Personal protective equipment: types, storage location, removal, handling and disposal Each department may have some variation (different manufacturer) of PPE. Discuss your department’s PPE types, storage location, etc. 33 Infectious Disease Prevention Following use, PPE should be removed and properly decontaminated or disposed of in an approved container Handle contaminated PPE as little as possible 34 Infectious Disease Prevention Review your department’s policy on the proper decontamination, storage and disposal of contaminated PPE 35 Infectious Disease Prevention Selection of Personal Protective Equipment: PPE shall be provided at no cost to the provider Considered “appropriate” if it does not permit blood or other potentially infectious materials to pass through 36 Infectious Disease Prevention Standard Precautions Hand washing Patient care Gloves equipment Gown Environmental control Mask, eye protection, face shield Linen Respiratory protection (N95 or (9508) HEPA, (99%)) 37 Infectious Disease Prevention Hepatitis B (HBV) Immunization Three shot series over six months Vaccine determined to be safe by the Centers for Disease Control & Prevention Majority of vaccine recipients develop adequate antibodies against HBV 38 Infectious Disease Prevention HBV Immunization is provided at no cost to the member Should be provided prior to working in an area where occupational exposure could occur Discuss HBV vaccination availability in your department 39 Infectious Disease Prevention Other Common Vaccines Td - Tetanus diphtheria MMR - Measles, Mumps & Rubella Influenza Varivax - Varicella virus vaccine (Chicken pox) 40 Infectious Disease Prevention Appropriate actions to take & persons to contact following an exposure incident Each department has a written Infection control plan. Discuss your department’s plan and determine appropriate contacts and actions. 41 Infectious Disease Prevention Appropriate actions to take after an exposure incident typically include: Contacting your immediate supervisor and / or infection control officer Go to an approved treatment facility or provider Complete all required written reports 42 Infectious Disease Prevention Procedure to follow if an exposure incident occurs: Discuss your departments policy on post exposure evaluation In general, always report the incident & document the route of exposure 43 Infectious Disease Prevention Medical Follow-Up & Treatment Should be provided as soon after exposure as possible (within one to two hours with HIV exposure) Shall be consistent with U.S. Department of Health & Human Services, Public Health Service, and CDC Prevention Guidelines 44 Infectious Disease Prevention General Post Exposure Evaluation & Follow-Up Guidelines: Document route of exposure & circumstances under which the exposure occurred Identification & documentation of source individual information 45 Infectious Disease Prevention Obtain source individual’s blood testing for HBV, HCV, and HIV (if source gives consent). If obtained, results of source individuals blood test provided to exposed provider 46 Infectious Disease Prevention Exposed provider baseline blood testing as soon after exposure as possible (with consent) Post exposure prophylaxis shall be provided when medically indicated, according to the U.S. Public Health Service (CDC) Standards 47 Infectious Disease Prevention Signs, Labels and / or Color Coding Required by the Bloodborne Pathogen Standard: Communications of hazards to employees (members) shall be accomplished by the use of signs and labels 48 Infectious Disease Prevention Warning labels shall be affixed to containers of regulated waste Universal biohazard symbol (orange or red-orange in color) Red bags or red containers may be substituted for labels Contaminated sharps containers and bags must be labeled appropriately 49 Infectious Disease Prevention Signs shall be posted at the entrance of work areas where occupational exposure may occur, e.g. areas used for cleaning and decontamination, or storage of medical waste 50 Infectious Disease Prevention Maryland’s Run Sheet (MAIS) A “runsheet” box for reporting an exposure is located next to the “hospital signature” section This is for tracking purposes ONLY and does not meet the documentation necessary to report an exposure incident 51 Infectious Disease Prevention Notification Laws Federal Law: 1990 Ryan White Comprehensive AIDS Resources Emergency Act Subtitle B, 42 U.S.C 300 ff-80 Maryland Notification Law: Health General 18-213 52 Infectious Disease Prevention Hospitals are required to: • develop written procedures • make copies available upon request • provide notification of possible exposure within 48 hours of confirmation of diagnosis • protect the confidentiality of the patient and the “first responder” 53 Infectious Disease Prevention HG §18-213 • Disease notification – All forms of viral hepatitis including but not limited to Hepatitis A,B,C,D,E,F, and G – HIV – Meningococcal meningitis – Tuberculosis – Mononucleosis – Diphtheria – Plague – Hemorrhagic fevers – Rabies 54 Infectious Disease Prevention HG §18-213 • Provides notification after contact with a person with certain diseases. – Notification 48 hours after confirmation of the disease by the hospital • Hospital makes notification in writing to Infection Control Officer. 55 Infectious Disease Prevention Communicable Disease Fact Sheets This program includes a series of “fact sheets” on more than forty communicable diseases Provided by the Maryland Department of Health & Mental Hygiene with Web Site: www.edcp.org/html/index.html 56 Infectious Disease Prevention Tuberculosis 57 Infectious Disease Prevention MMWR MORBIDITY AND MORTALITY WEEKLY REPORT October 28, 1994 / Vol. 43 / No. RR-13 Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Facilities, 1994 58 Infectious Disease Prevention Who does this document apply to? Health Care Workers (HCWs) “HCWs refers to all paid and unpaid persons working in health-care settings who have the potential for exposure to M. tuberculosis. This may include... emergency medical service (EMS) personnel.” 59 Infectious Disease Prevention Specific measures to reduce the risk for transmission of M. tuberculosis include assigning responsibility: Designated Officer 60 Infectious Disease Prevention Specific measures to reduce the risk for transmission of M. tuberculosis include: Conducting a risk assessment to evaluate the risk for transmission of M. tuberculosis in your community and work setting Develop a written TB Infection Control Program based on your risk assessment 61 Infectious Disease Prevention Periodically repeating the risk assessment to evaluate the effectiveness of the TB Infection Control Program 62 Infectious Disease Prevention Developing, implementing, and enforcing policies and protocols to ensure early identification of patients who may have infectious TB 63 Infectious Disease Prevention A diagnosis of TB should be suspected in any patient with the following: Productive cough (<2 to 3 wks duration) Fever - Chills Night sweats Easily fatigable Loss of appetite (anorexia) weight loss Hemoptysis (bloody sputum) 64 Infectious Disease Prevention Managing patients who may have TB in ambulatory care setting and emergency departments: Attempt to identify any potentially TB infected patient e.g. history, signs & symptoms, any previous positive TB treatment, or any current anti-tuberculosis medications 65 Infectious Disease Prevention Utilize engineering controls where possible and use of approved PPE when treating and transporting a patient suspected of having TB TB patients, if medically stable, should remain in the transport unit (with a provider) until receiving facility is notified and ready to accept the patient 66 Infectious Disease Prevention Developing, implementing, maintaining, and evaluating a respiratory protection program: Personal Protective Equipment (PPE): Respiratory Protection (NIOSH approved mask e.g. N-95 or HEPA and other PPE as per local protocol) Meets adequate filtration standards 67 Infectious Disease Prevention Qualitatively or quantitatively fit tested Respirators available in at least three sizes Ability to be checked for face piece fit (OSHA) Must comply with CFR 1910.134 (OSHA Respiratory Standard) 68 Infectious Disease Prevention Use precautions while performing cough-inducing and other high hazard procedures: Characterized by potential to generate airborne / droplet secretions Aerosolized medication treatment Endotracheal Intubation Suctioning Transporting a patient with active TB disease in a closed vehicle 69 Infectious Disease Prevention Educating and training HCWs about TB, effective methods for preventing transmission of M. tuberculosis, and the benefits of medical screening programs. Tuberculosis Training Program 70 Infectious Disease Prevention What Is Tuberculosis? Mycobacterial disease Caused by the infectious agent: Mycobacterium tuberculosis Transmitted by infected airborne particles called droplet nuclei 71 Infectious Disease Prevention What Is infectious? Capable of causing infection Caused by a pathogen Illness resulting from an invasion of a host by a disease producing organism 72 Infectious Disease Prevention TB Infection can result from exposure to infectious droplet nuclei Positive PPD but, no clinically apparent signs or symptoms of TB Negative CXR & negative smears and cultures which means usually not infectious May develop into TB disease 73 Infectious Disease Prevention TB disease develops in a person with tuberculosis infection Usually is infectious if not treated Signs and symptoms apparent with positive lab test 74 Infectious Disease Prevention Develop and implement a program for routine periodic counseling and screening of HCWs for active and latent TB infection: PPD skin testing is used to detect TB infection 75 Infectious Disease Prevention Skin test conversion from negative to positive indicates a new infection with TB A person with a positive PPD should be clinically evaluated for active tuberculosis A person with a positive PPD should be evaluated for preventive therapy if no active disease is present If TB disease is detected, begin treatment per local policy 76 Infectious Disease Prevention Interpretation of TB Skin Test Indurations of: 5 mm or larger considered positive after close personal contact, abnormal CXR or in known HIV infected persons 10 mm or larger considered positive in persons with other known risk factors (HCW) 15 mm or larger considered positive in all other populations 77 Infectious Disease Prevention Promptly evaluate possible episodes of M. tuberculosis transmission in your health care setting An exposure to TB is defined as: Potential exposure to the exhaled air of an individual with suspected or confirmed TB disease Exposure to high hazard procedure performed on persons with suspected or confirmed TB disease 78 Infectious Disease Prevention Risk Factors for TB Disease Development Only about 1 in 10 people infected ever suffer active disease Reactivation of TB is likely if the host has impaired immunity, including diabetes, chronic renal failure, malnourished, high-dose corticosteroid therapy, some hematologic disorders, or HIV infection 79 Infectious Disease Prevention Treatment of Tuberculosis Drug susceptibility testing should be performed on all initial isolates from patients with TB Until results are known, two basic principles of therapy apply: 1) Start with the four primary drugs used in the treatment of TB until sensitively and resistance are known 2) Continue treatment regimen with at least two drugs known to be effective on the isolate 80 Infectious Disease Prevention Drug Resistant Tuberculosis Where therapy is not continuous or incomplete, multi-drug resistant tuberculosis can develop (MDR-TB). MDR-TB can be treated but, treatment is with second line drugs that are less effective. MDR-TB requires longer treatment regimens: 18 to 24 months (due to lower efficacy) 81 Infectious Disease Prevention TB Surveillance & Reporting Skin test conversions among personnel PPD done at time of employment and (annually) periodic re-testing thereafter Evaluation of exposure incidents Evaluations & management of positive PPD skin tests or symptoms of TB Follow-up of personnel with positive PPD skin test 82 Infectious Disease Prevention Follow-up After TB Exposure Clinically evaluate for active TB Negative PPD in preceding 3 months - repeat 12 weeks after exposure Negative PPD longer than 3 months ago, repeat baseline and if this one is negative, repeat in 12 weeks A positive PPD requires clinical evaluation and management 83 Infectious Disease Prevention Tuberculosis Prevention & Control Unit ventilation: keep adequate ventilation in the treatment area of the transport vehicle e.g., windows, exhaust fans, air out vehicle after run Work practices to prevent the spread of airborne droplets When treating and transporting HIV infected patients, IVDAs, foreign born, and other high risk groups for TB, PPE should routinely include airborne protection 84 Infectious Disease Prevention TB Prevention & Control - Continued Face & eye protection during exposure prone activities, e.g. endotracheal intubation, suctioning, positive pressure demand valve ventilation Decontamination with E.P.A. approved hospital grade detergent disinfectant Tuberculosis screening program Preventive therapy or treatment Documentation 85 Infectious Disease Prevention Preventive Therapy Coordinating activities with the local public health department, emphasizing reporting, and ensuring adequate follow-up and continuation and completion of therapy 86 Infectious Disease Prevention Preventive drug therapy substantially reduces the risk of developing clinically active tuberculosis in infected persons If an infected person is a candidate for preventive therapy he/she could be placed on six to twelve months of daily (specific) anti-tuberculosis drug therapy 87 Infectious Disease Prevention 5.3 - 10.4 0.0 - 5.2 > 15.6 Wash. DC >15.6 0.0 - 5.2 5.3 - 10.4 > 15.6 Alaska - 5.3 - 10.4 Hawaii - >15.6 10.5 - 15.6 10.5 - 15.6 Tuberculosis in the U.S. Rates per 100,000 Population by State 88 Prevention and Vigilance is Your Only Cure 89