File
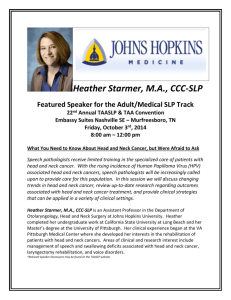
advertisement

EXAM REVIEW S CONDITIONS Part II S WHIPLASH S Definition: S Rapid acceleration or deceleration injury of the head and neck. S AKA: WAD – whiplash associated disorder S 4 categories: 1) neck pain without musculoskeletal signs, 2) pain with musculoskeletal signs, 3) pain with musculoskeletal and neurological signs, 4) pain with all signs and cervical fracture or dislocation WHIPLASH S Causes: S S S S S S Compressive or tensile stress from rapid acceleration or deceleration. Auto accidents, recreational or occupational activities. Rear impact collision is the most common cause: hyperextension - flexion Side impact from left: Left lateral flexion – right lateral flexion Longus colli and scalenes most often injured. History: S S S S S S S S S S Report a head or neck trauma Symptoms may appear immediately or be delayed weeks or months. Localized cervical pain which may refer to thoracic, lumbar or upper extremity. Dull, aching pain from spasm or TPs Sharp pain from acute spasm. Stiffness limiting ROM Edema, paresthesia, numbness Dizziness, vertigo or disorientation Bite problems, TMJ pain Nausea, headache, breathing difficulties. WHIPLASH S S S Observation: S Obvious movement limitations. S Apprehension of movement due to possibility of pain. S Signs of face or head trauma: bruising. Palpation: S Palpable heat or swelling. S Severe inflammation: visible redness. S Tissues expected to be tender. S Hypertonicity and referred TP pain. S Palpable defect or disruption in muscle fibres. S Misalignment of landmarks indicates possible dislocations. S Adhesions or scar tissue from chronic strain injury. Testing: S AROM: S Limited ROM due to spasm, pain avoidance or vertical displacement of facet joint dysfunction. S Pain or restriction in extension: anterior tissues indicated. In flexion: posterior tissues. S Compression on facets may present neurological symptoms. S Motions may produce vascular compression: symptoms of dizziness, vertigo, disorientation, ringing in ears, blurred vision, sensory impairment caused by lack of blood flow to brain. WHIPLASH S PROM: S S S MRT: S Pain due to reactive muscle guarding, spasm and hypertonicity. S Severe: pain from muscles pulling on vertebrae – fracture or facet dysfunction. S Weakness due to reflex inhibition, joint dysfunction, nerve compression or tension. Special Tests: S S Pain at end range as tissues are stretched. Otherwise S/A None Contraindications: S Potential absolute contraindication based on severity. S Referral to physician for additional evaluation encouraged. WHIPLASH S Treatment Goals: S Reduce fascial restrictions through gentle myofascial work. S Reduce spasm and neurological activity in affected tissues. S Restore ROM through stretching and massage. S Reduce inflammation and tension. S Re-educate posture S Hydrotherapy: S Acute: S Ice and cold applications especially useful for treating spasm. (slows nerve conduction rate) S Chronic: S Heat to reduce tension and reduce excessive sympathetic nervous system activity. S Self-Care: S Stretch: Gentle ROM stretching for 10 mins every day. S Strengthen: Shoulders, neck isometrically. S Educate: Proper work ergonomics, general good posture. Take breaks from prolonged periods in one position. Don’t hold phone between head and shoulder, carry less weight, lift properly from the knees. SPINAL LIGAMENT SPRAIN S Definition: S S Sudden force overload to the spine causing damage and tearing to ligament. Causes: S WAD, traumatic injuries. S Overwhelming sudden tensile load S Ligaments can be weakened by prolonged stress making them more susceptible to injury from less severe trauma. S More prevalent in persons with systemic disorders which involve connective tissue weakness: Ehlers-Danlos or Marfan syndromes. S Women in late pregnancy are more susceptible due to relaxin. S Hypermobility is often a precursor SPINAL LIGAMENT SPRAIN S S S S History: S Client describes a sudden force load to head or neck. S Ask about mechanics of injury, previous sprains, injuries or accidents and systemic disorders. Observations: S Rarely visual clues. S Severe cases: vertebral dislocation – spinous processes will appear misaligned. Palpation: S Palpation of superficial ligaments may cause pain. S Deep ligaments are sometimes difficult or impossible to palpate. S Hypertonicity and tenderness of local muscles due to muscle splinting. S Edema if sprain is of a superficial ligament. Testing: S AROM: S Pain when motion is in direction ligament is designed to resist. S Motions that shorten affected ligaments may reduce pain or have no effect. SPINAL LIGAMENT SPRAIN S S PROM: S S/A MRT: S Fascial connections between ES and supraspinous ligaments lead to possible pain with resisted extension. S Special Tests: S None S Contraindications: S None S Treatment Goals: S Increase collagen production with deep friction. S Reduce muscle spasm and pain. S Hydrotherapy: S Ice in first 72 hours after injury. 3 times a day for 20 mins. S Contrast therapy after acute stage. SPINAL LIGAMENT SPRAIN S Self-Care: S Ligaments usually eventually heal themselves. S Rest from offending activities. S Stretch: muscles which may be splinting. S Strengthen: opposite side muscles that are not being used due to guarding. TORTICOLLIS S “Wry Neck” (acute) or twisted neck S Involuntary muscle contractions that lead to abnormal positions/tremors of the head and neck S Typical torticollis position = Head and neck side-bent towards affected side, face turned away from affected side, shoulder on affected side raised S Acute Acquired: S Most common S SCM, trapezius, levator scapulae, splenius capitis and cervicis, scalenes S PAINFUL unilateral shortening/spasm of neck muscles = abnormal head position S Muscles in short position for extended periods (ex. Sleeping, holding phone, reading in bed) S Activation of latent trigger points, sublux of C1 and C2 (whiplash, turning head too hard), infection (tonsillitis, ear infection), emotional stress, facet joint irritation, cervical DDD) TORTICOLLIS S S Congenital: S Onset infancy, birth, or shortly after S Not necessarily painful S Contracture of one SCM, fibrosis, scarring, palpable mass S Birth trauma, tissue ischemia (intra-uterine pressure or position), cranial bone torsion, sublux of C1 or C2, imbalance in cranial membranes (faux and tent), spinal cord abnormalities S Scoliosis develops S Medical treatment – muscle stretching, physiotherapy, surgically divide muscle S If not treated, permanent deformity Spasmodic: S Localized dystonia – involuntary spasm of cervical muscles and abnormal head position S Idiopathic, dysfunction of basal ganglia (controls movement), reaction to medication or infection, depression/stress, malformation of atlanto-occipital articulation, scoliosis, trauma to head and neck S Jerk and twitch in neck, affected shoulder shrugs uncontrollably (intermittent or permanent) TORTICOLLIS - ACUTE S Definition: S S S Painful unilateral shortening or spasm of neck muscles resulting in an abnormal head position Causes: S Activated latent trigger points in cervical muscles. S Subluxation (dislocation) of C1 on C2 due to trauma S Facet joint irritation S Infection S Disc-related pain Symptoms: S Sudden onset S Neck and head are in typical torticollis position S Affected muscles are shortened and in spasm S Pain is present, especially on movement, breathing is rapid and shallow S Muscle trigger points in SCM are affected - tinnitus, nausea or tearing of the eye on shortened side may be present S Facet Joint Irritation (FJI) - came on suddenly after abrupt movement; there may also be pain between the scapulae. Person is usually under 30 S Degenerative Disc Disease (DDD) - pain has gradual onset, person wakes up with torticollis after sleeping in awkward position TORTICOLLIS - ACUTE S Observation: S S S Muscle spasms keep head in non-neutral position, with chin rotated to opposite direction, head may be held in extension, hyperextension, or lateral flexion, muscle spasm may be visible in SCM Palpation: S Heat, point tenderness, firmness and increased tone. S Contractured muscle may be tender and feel cool due to ischemia and be hard and fibrous. Testing: S AROM: S S PROM: S S Painful and restricted Pain and restriction MRT: S Pain felt when engaged, possible weakness due to shortened muscle length TORTICOLLIS - ACUTE S S S Special Tests: S Cervical Distraction Test - to differentiate a nerve root compression that may underlie an acute acquired torticollis S Vertebral Artery Test - rules out vascular insufficiencies S Spurling's Test - performed after the spasm has reduced may indicate facet joint irritation Contraindications: S Avoid full stretch to SCM if vertebral artery is positive S Do not passively stretch spasmodic muscles Treatment plan (stage-dependent): S S Reduce pain, spasm, and abnormal positioning Hydrotherapy: S Cold therapy is used to reduce pain S Heat is used to increase circulation and flush metabolites TORTICOLLIS - ACUTE S Self-care: S Diaphragmatic breathing S Hydrotherapy S Self-massage S Stretching Due to muscle imbalances Due to capsular dysfunction TORTICOLLIS - CONGENITAL S Definition: S S S Contracturing of one SCM muscle resulting in on abnormal head position Causes: S Presents in infancy S Possible trauma in birth process due to forceps, caesarean section or breach birth S Position in the womb S Torsion of fetus’ bones S Tissue ischemia S Causes are not clearly understood and still considered theoretical Symptoms: S May develop over days to three weeks after birth S Contracture, thickening and shortening of one SCM and scalenes and associated fascia; may be palpable mass in muscle S Unable to move neck S Not painful TORTICOLLIS - CONGENITAL S Observation: S S S Head and neck are in typical torticollis position Palpation: S Heat, point tenderness, firmness and increased tone. S Contractured muscle may be tender and feel cool due to ischemia and be hard and fibrous. Testing: S AROM: S S PROM: S S Movement is restricted Is very restricted with leathery feel MRT: S Possible weakness of contralateral and anterolateral neck muscles TORTICOLLIS - CONGENITAL S S Special Tests: S Cervical Distraction Test - to differentiate a nerve root compression that may underlie an acute acquired torticollis S Vertebral Artery Test - rules out vascular insufficiencies S Spurling's Test - performed after the spasm has reduced may indicate facet joint irritation Contraindications: S S lf working with infants, use reduced pressure when treating the contractures. Avoid full stretches to SCM if Vertebral Artery Test is positive Treatment plan (stage-dependent): S Lengthen contractured structures S Reduce abnormal positioning S Restore ROM of head and neck S Strengthen weak structures TORTICOLLIS - CONGENITAL S Hydrotherapy: S S Heat is applied to affected structures Self-care: S ln infants - educate parents in passive stretching and repositioning of the head. ROM retraining (at three months of age) - infant is supine and an object is placed in the infant's line of vision about a foot away from the head. Allow the infant to focus on the object. Have parent stabilize object and slowly move the object away from the affected side. Restart each time the infant loses focus on the object until maximum ROM is achieved. TORTICOLLIS - SPASMODIC S Definition: S S S Localized dystonia resulting in an involuntary spasm of cervical muscles and an abnormal head position Causes: S Most cases are idiopathic - linked to depression, severe stress, occupational position of the head S CNS lesions - encephalitis and basal ganglion disease S Postural dysfunctions (scoliosis) S Trauma to head and neck S Iatrogenic with treatment of Parkinson's by the drug levodopa Symptoms: S Adult onset S Presents in typical torticollis position S Unaffected muscles in neck jerk and twitch and unaffected shoulder shrugs uncontrollably. May spread to facial and arm muscles. S May be intermittent or permanent S Stress may exacerbate the condition S Raising arms and applying straight pressure to the chin with one finger may improve factors as does carrying something on the shoulder TORTICOLLIS - SPASMODIC S Observation: S S S Head and neck are in typical torticollis position Palpation: S Heat, point tenderness, firmness and increased tone. S Contractured muscle may be tender and feel cool due to ischemia and be hard and fibrous. Testing: S AROM: S S PROM: S S Painful and restricted Pain and restriction MRT: S Pain felt when engaged, possible weakness due to shortened muscle length TORTICOLLIS - SPASMODIC S S S Special Tests: S Cervical Distraction Test - to differentiate a nerve root compression that may underlie an acute acquired torticollis S Vertebral Artery Test - rules out vascular insufficiencies S Spurling's Test - performed after the spasm has reduced may indicate facet joint irritation Contraindications: S Painful techniques, joint play and direct massage are contraindicated as they may make spasm more pronounced. S Avoid full stretches to SCM if Vertebral artery test is positive. Treatment plan (stage-dependent): S Reduce SNS firing and spasm S Reduce abnormal positioning S Restore ROM of head and neck TORTICOLLIS - SPASMODIC S Hydrotherapy: S S Heat is used to reduce hypertonicity Self-care: S Diaphragmatic breathing, pain-free ROM of the neck, slow passive stretches HEADACHES S a. Tension: S Muscular origins, associated trigger points and myofascial pain syndrome S Two categories: c. Primary – headache is condition S Secondary – headache result of underlying condition Cervicogenic S b. S Unilateral, frontal, arising from neck structures Spinally mediated S Trigger point origins in neck or thorax S Hyperactivity of SNS at vertebral level S “Spinal facilitation” Chronic daily headache S Daily, constant with fluctuations in pain S Causes are trigger points, trauma, infection, lack of sleep, postural imbalance, TMJ dysfunction, stress S Treated with analgesics S Warning sign is new headaches later in life HEADACHES S S Bilateral, diffuse, constant pain (dull or vice-like) S Begins in adulthood S Onset in late afternoon S Duration: 30 minutes to weeks S Frequency variable S Muscle tenderness, stiffness, hypertonicity, loss of appetite S Caused by stress, poor posture, fatigue S Person can still function Migraine: A. Migraines S Paroxysmal (sudden onset) neurological disorder with many signs and symptoms S “Hemicranias” – half of the head S Different theories: vascular model (vasoconstriction of cranial arteries followed by vasodilation), neurogenic theory (disorder of CNS, reduction of cerebral blood flow and wave) S Genetics, triggering factors HEADACHES B. S Remedies include peppermint oil, acupressure headache band, feverfew, willow bark extract, fish oil; Chinese medicine emphasized acupuncture, herbs, diet, and lifestyle change S Prescription drugs – Imitrex, Midrin Mixed/Transformational Headaches S Shared tension- and migraine-type headaches C. Cluster Headaches S Abnormal hypothalamic function S Grouping of headaches, 1x/day for weeks D. Drug-Associated Headaches S “Rebound headaches” because of continual use of OTC medications (analgesics, caffeine) S Begin in early morning when in need of a “fix” E. Trauma-Related Headaches S Unilateral, dull ache that localizes to intense pounding S Begins in childhood, adolescence, or adulthood S Early morning onset HEADACHES S Duration 4 to 72 hours S Frequency less than once per week S Sore muscles, hypersensitivity to light and sound, nausea, cold extremities, sweating S Many triggering factors S Person withdraws from activity TENSION HEADACHES S Headaches can range from a life-threatening disease to a minor complaint. If you suspect that the headache may be a red flag to an underlying pathology, be sure to refer the client for medical diagnosis. S Observations: S S Palpation: S S We should do a full postural assessment. We are looking for a head forward position, hyperkyphosis, hyperlordosis, scoliosis or pes planus Be sure to palpate the neck, shoulders, and thoracic muscles. Also muscles of mastication may be hypertonic and tender. The diaphragm, intercostals, scalene, and SCM may also be hypertonic. ROM Testing: S AROM and PROM – are performed on the neck, thorax and shoulder. There is reduced cervical and thoracic mobility in both of these ROM due to trigger points. There may be reduced ROM in the mandible as well. S MRT – the affected neck, head, and shoulder girdle muscles may be weaker TENSION HEADACHES S S Special Tests: S Motion and static palpation are performed in the cervical and thoracic spine S Differential tests – Spurling’s, cervical compressin and cervical distraction tests are used to differentiate a facet joint irritation Treatment: S (During the headache): the context of the treatment is relaxation. Can use diaphragmatic breathing. We want to reduce sympathetic nervous system firing, pain, hypertonicity, trigger points, joint dysfunction, and to increase ROM. S Effleurage on pectorals, posterior neck muscles such as upper trapezius and levator scapulae, are used to reduce hypertonicity. Petrissage can be used on the muscles of mastication, facial muscles and the scalp. Trigger points can be addressed with stripping and compression. You must remember to work within the client’s pain tolerance and check to see if the treatment is making the headache better or worse. Remember to flush the neck, shoulders and upper thoracic area. S (Between headaches): the treatment can be very similar. You may be able to work with more vigor and perhaps a little deeper. TENSION HEADACHES S Hydrotherapy: S S Heat can be used as a pre-treatment to the affected muscles. Cold may also be placed on the referral pattern for an analgesic effect. Heat can also be used after trigger point therapy. Contrast therapy can be applied to the neck and head to relieve a tension headache. This can be done by using warm and cool towels. Self-Care: S The client should rest after trigger point therapy. The client can use hydrotherapy to relieve headaches. Diaphragmatic breathing can be used to promote relaxation, reduce stress and relieve pain. Self massage can be applied in the form of stripping, compression and stretching. The client can also begin to strengthen weak muscles. The client can also work on correcting any postural distortions. TENSION HEADACHES – HOME CARE S S Etiology (Causes): S Recognized causes include hypertonicity of cervical muscles, trigger points within muscles that refer into the head and neck, and postural imbalances. Risk factors include: S Trauma to head, neck or spine S Infection (e.g. Sinusitis) S Emotional Stress S Postural Imbalances (e.g. Scoliosis, head forward posture, hyperkyphosis) S Temporomandibular joint dysfunction S Allergies or Sinusitis S Sleep disturbances S Others Purpose of Home Care S Lengthen muscles associated with tension headache S Decrease hypertonicity within those muscles S Increase cervical Range of Motion S Strengthen weak, overstretched muscles S Correct postural imbalances S Research shows that exercise is important for headache prevention and treatment TENSION HEADACHES – HOME CARE S General Home Care Instructions S Keep your neck muscles warm and avoid drafts on your neck (i.e.: wear a scarf) S Suggestions for sleeping S S Sleep on your side with a pillow under your head and neck, or on your back. S Avoid sleeping on your stomach as this puts too much pressure on your neck. S Use a pillow that is able to conform to the shape of your neck S Keep your jaw relaxed, teeth apart, and your tongue on the roof of your mouth just behind (but not touching) your front teeth. (lf you have a night guard, wear it.) Proper biomechanics when sitting are extremely important to avoid stress on your joints and muscles - sit up straight, with shoulders back and down. S Change positions often S When reading, raise you reading material to eye level S Ensure your chair is neither too high nor too far away from your work S Keep your jaw relaxed, teeth apart, and your tongue on the roof of your mouth just behind (but not touching) your front teeth. S When watching television, support your head by sitting up straight as though your body is being pulled by a string towards the ceiling (as opposed to laying on your side) S When reading in bed sit up as straight as possible with the book raised to eye level, propped using pillows or other supports (as opposed to lying on your stomach with your head tilted up or rotated to one side) TENSION HEADACHES – HOME CARE S Other suggestions S Anti-inflammatories (see your doctor) S Mouth guard if grinding/clenching teeth is a contributing factor (see your dentist) S Acupuncture S Progressive muscle relaxation (PMR) S If postural imbalances are job related, assessment of work area is important S Hydrotherapy S Contrast Neck/Upper Back Compress S Apply a hot compress to neck and upper back for 3 minutes S Place a cold compress to the neck and upper back for no longer than I minute, make sure the rest of the body is warm and dry to avoid chilling S Repeat the procedure 3-5 times S Finish with cold to avoid congestion S Contrast can be repeated 2 to 3 times per day S Make sure temperatures are not too extreme. Heat and cold packs should be wrapped in a thin dishtowel to prevent damage to the skin S For hot compress: soak a towel in hot water (about 40 degrees Celsius) or use a heating pad. S For cold compress: soak a towel in cold water (1 degree Celsius) or use a cold pack. TENSION HEADACHES – HOME CARE S S Stretching Exercises S Tissues respond best when warmed prior to stretching. It is ideal to actively warm-up with physical activity such as a stationary bike or passively warm-up with a warm shower or by applying heat to the area to be stretched. S All movements should be pain-free, and performed in a smooth, un-hurried manner. Sit/stand tall with breastbone lifted, head straight, tongue on the roof of your mouth, just behind (but not touching) your front teeth. S With all stretches, move until you feel a gentle stretch, hold until the stretch feeling goes away (usually 30 seconds), take up the slack until you feel the next gentle stretch and repeat until you have completed 3 stretches. Do all stretches 2-3 times per day. 1. “CHIN TUCK” (Stretch for posterior neck muscles). S This exercise can be performed sitting or lying on your back. Start in a head forward position. The chin is then tucked, and the head pulled back while the chin stays at the same level. Head should not tilt up or down during this activity, keep your eyes at horizon level. Chin must remain parallel to the floor TENSION HEADACHES – HOME CARE S 2. Stretch for lateral neck muscles (Scalenes) S These stretches are best performed lying on your back so that the neck muscles are relaxed and proper alignment is achieved. The arm on the side being stretched is anchored under the hip and the opposite hand is placed over the top of the head and above the ear on the stretch side. S Slowly bring your ear toward your shoulder. Be sure to keep shoulders fixed, and do not lean your body to the side. S This stretch is done with 3 head positions to isolate the anterior, middle, and posterior scalene muscles. Repeat 3 times in each position. Once finished on one side of the neck repeat the entire procedure to opposite side. S 3. "DOORWAY STRETCH" (Pectoralis Major/Minor Stretch) S Stand in doorway. S Position palm of side to be stretched on doorframe with fingers pointing upwards, full forearm in contact. S Step slightly forward while keeping low back neutral (no arching), bringing the shoulder blades together S Avoid jutting your chin/head forward. S Move to where you feel a gentle stretch and hold until it releases. Then move further until the next gentle stretch is felt, repeat for 3 stretches. S The stretch is to be done 3 times in each position to isolate all muscle fibre directions: S Elbow slightly lower than shoulder S Elbow same height as shoulder S Elbow slightly higher than shoulder TENSION HEADACHES – HOME CARE S 4. “TOWEL ROLL” (Positional Stretch for Anterior Thorax) S Place a foam roll or rolled up hand towel (rolled from top to bottom) lengthwise along the center of your spine. S Lie on top of the roll facing the ceiling with your palms upward. S Arms can be placed at varying angles as shown. S Stay in this position at least 15 minutes for maximum benefit. S If needed place a small towel roll under your neck for support. S Strengthening Exercises S 1.”HEAD LIFT” (Cervical Flexion Exercise) S Lie on your back, with a pillow or roll under your knees. S In a SLOW, controlled motion, tuck your chin and then bring chin to chest, slightly lifting your head. S Hold for 10 seconds. Release. S Repeat until muscles in the front or the back of the neck start to feel fatigued. S Repeat 2-3 times each day. TENSION HEADACHES – HOME CARE S 2. “WALL ANGELS” (Middle and Lower Back Strengthening Exercise) S Sit on a stool with back against wall. S Place back of elbows, forearms and wrists against the wall. S Keep upper back straight, press head back with chin down and in, and gently flatten low back by pulling up and in with lower abdominal muscles. S Bring arms up and down slowly in a small arc of motion while keeping elbows in contact with wall. S Repeat until muscles start to feel fatigued. S This exercise can also be done standing, with heels approximately 3 inches from the wall. MIGRAINE HEADACHES S S There are two main categories for migraines: S Migraine without Aura (common migraine) – This condition affects 85% of people with migraines. In the 24-48 hour period before the migraine, the person experiences premonitory symptoms. This may include mood changes, food cravings, altered sensory perception, excessive yawning, and memory dysfunction. These may develop in the hypothalamus S Migraine with Aura (classic migraine) – This affects 15% of people with migraines. The aura is associated with a reduction in the cerebral blood flow. It develops gradually over 5 to 20 minutes, lasting for less than one hour and resolving with the headache. Auras are usually visual, often perceived as flashing lights, zig-zags lines, or visual distortion. They may also be sensory, such as pins and needles around the lips and hands. Auditory disturbances include hissing or rumbling noises. Observation: S A full postural assessment, looking for head forward posture, hyperkyphosis, hyperlordosis, scoliosis or pes planus MIGRAINE HEADACHES S Palpation: S S S The neck, shoulder and thoracic muscles and muscles of mastication may be hypertonic and tender. The muscles of respiration are also likely to be hypertonic including the diaphragm, intercostals, scalene, and SCM. Ischemia produces coolness in the skin of the neck or thorax. ROM Testing: S AROM and PROM – are performed on the neck, thorax, shoulder and mandible, There is reduced cervical and thoracic mobility. There may be reduced ranges in mandibular motion. S MRT – it may reveal the neck and shoulder girdle muscles to be weaker and overused Special Tests: S Vertebral Artery Test, Spurling’s Test MIGRAINE HEADACHES S S S Treatment: S (During an attack) – The treatment is limited to 30-45 minutes and in the context of a relaxation massage. The treatment goals are to decrease pain and hypertonicity. You may not be able to work directly on the head or neck. In fact you may not be able to massage them at all during an attack. If they can tolerate the work, MLD for the head and neck is indicated. Swedish work to the shoulder girdle, neck and scalp may be done. Be sure that the pressure is gentle. S (Between attacks) – You are trying to reduce the sympathetic nervous system firing, hypertonicity, trigger points, increase ROM and tissue health. The treatment is similar to what you would perform during the attack but the therapist can be more vigorous. You may also be able to address trigger points and hypertonicity. Hydrotherapy: S During an attack, hydrotherapy is cold or ice to the head and neck S Between attacks, hydrotherapy is now heat Self Care: S Self massage of the neck, face, and scalp can abort a migraine in progress. Hydrotherapy can be used for self care. Aerobic exercise between attacks may help to decrease the frequency of migraines. Stretching the neck and shoulder muscles, regulating sleep, regular meals and exercise, avoiding food triggers, and managing stress may also be beneficial. BREAK S STRENGTHENING EXERCISES FOR THE NECK S LONGUS COLLI, SCM, AND LONGUS CAPITIS S The purpose of this exercise is to increase neck strength and muscular endurance. The benefits are improved stability, functional strength and injury prevention. S Begin by lying on the back with the head extended off the table, maintaining a chin tuck position. S Slowly extend the head back towards the floor and then raise the head, returning to the initial neutral starting position and repeat as instructed. S Move slowly through the range of motion. Slowly return to start position. Repeat for prescribed repetitions and sets. ISOMETRIC STRENGTHENING S LATERAL FLEXORS OF THE NECK S Place the middle of the theraband around the side of your head. S Grasp the ends of the band at the other side of your head. S Keep your neck in a neutral position with chin slightly tucked. S Extend your elbows, stretching the band to the side of you. S Slowly return, and keep your neck stable. S Can repeat with the band on the other side of your head. CERVICAL ROTATORS S Place the middle of the band around the back of your head. S Cross the ends of the band over your forehead and grasp the ends of the band at eye level near your head. S Keep your neck in a neutral position with your chin slightly tucked. S Extend your elbows outward to the side, stretching the band away from your head. S Slowly return, and keep your neck stable. S Repeat with other hand. CERVICAL FLEXORS S Place the middle of the band around the front of your head, holding each end of the band at the side of your head, near eye level. S Keep your neck in a neutral position with the chin slightly tucked. S Pull the ends of the band backward. S Slowly return, and keep your neck stable. CERVICAL EXTENSORS S Place the middle of the band around the back of your head. S Grasp the ends of the band in front of your head. S Keep your neck in a neutral position with the chin slightly tucked. S Extend your elbows, stretching the band in front of you. S Slowly return and keep your neck stable. LAB In partners, practice Strengthening Exercises for the Neck S LUNCH S INSTRUCTOR DEMOS Demo Neck treatment with the following structures treated: Upper traps, platysma, SCM, Scalenes, Levator Scapula, Pectoralis Minor, Suboccipitals, Longus Colli, Digastric/hyoids, Vertebral Translation, Traction, Stretches, Effleurage to flush from head S LAB In partners: practice neck treatment with the following structures: Upper traps, platysma, SCM, Scalenes, Levator Scapula, Pectoralis Minor, Suboccipitals, Longus Colli, Digastric/hyoids, Vertebral Translation, Traction, Stretches, Effleurage to flush from head S REVIEW FOR MIDTERM EXAM S