Southlake Clinic currently has an exciting career opportunity for a
advertisement
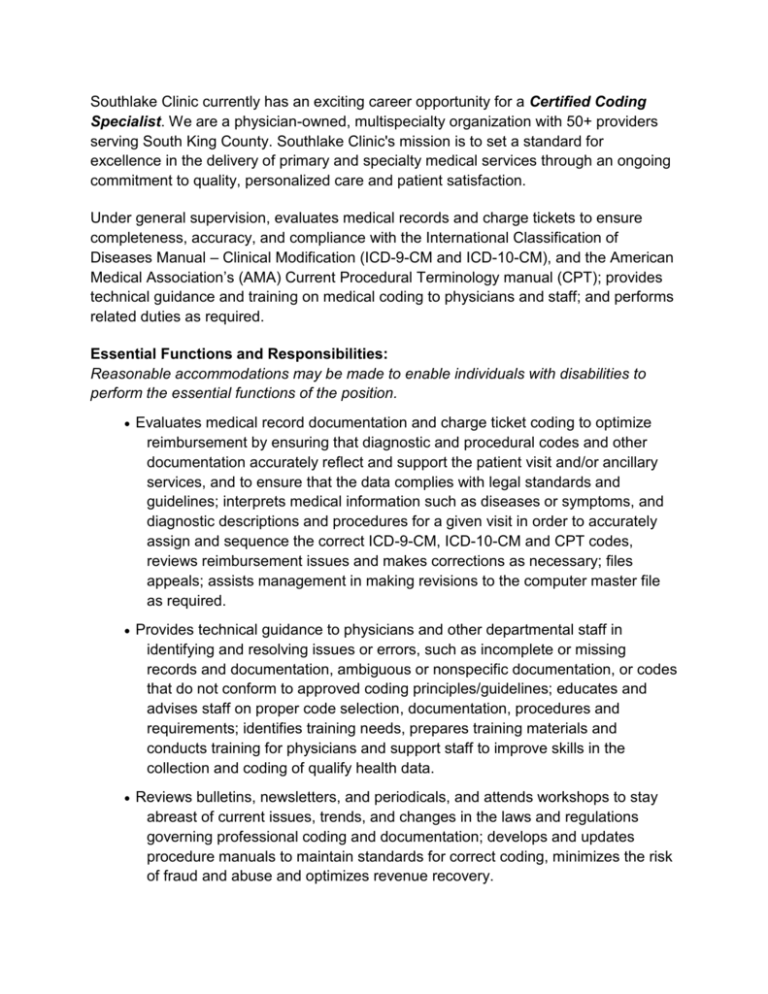
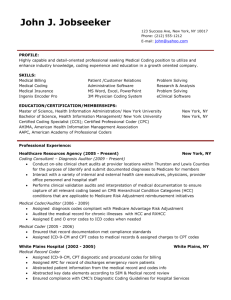
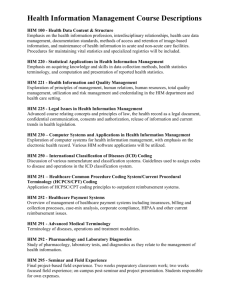
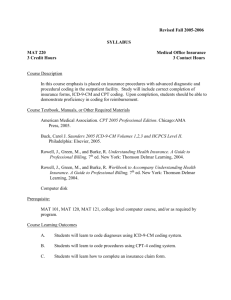
Southlake Clinic currently has an exciting career opportunity for a Certified Coding Specialist. We are a physician-owned, multispecialty organization with 50+ providers serving South King County. Southlake Clinic's mission is to set a standard for excellence in the delivery of primary and specialty medical services through an ongoing commitment to quality, personalized care and patient satisfaction. Under general supervision, evaluates medical records and charge tickets to ensure completeness, accuracy, and compliance with the International Classification of Diseases Manual – Clinical Modification (ICD-9-CM and ICD-10-CM), and the American Medical Association’s (AMA) Current Procedural Terminology manual (CPT); provides technical guidance and training on medical coding to physicians and staff; and performs related duties as required. Essential Functions and Responsibilities: Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions of the position. Evaluates medical record documentation and charge ticket coding to optimize reimbursement by ensuring that diagnostic and procedural codes and other documentation accurately reflect and support the patient visit and/or ancillary services, and to ensure that the data complies with legal standards and guidelines; interprets medical information such as diseases or symptoms, and diagnostic descriptions and procedures for a given visit in order to accurately assign and sequence the correct ICD-9-CM, ICD-10-CM and CPT codes, reviews reimbursement issues and makes corrections as necessary; files appeals; assists management in making revisions to the computer master file as required. Provides technical guidance to physicians and other departmental staff in identifying and resolving issues or errors, such as incomplete or missing records and documentation, ambiguous or nonspecific documentation, or codes that do not conform to approved coding principles/guidelines; educates and advises staff on proper code selection, documentation, procedures and requirements; identifies training needs, prepares training materials and conducts training for physicians and support staff to improve skills in the collection and coding of qualify health data. Reviews bulletins, newsletters, and periodicals, and attends workshops to stay abreast of current issues, trends, and changes in the laws and regulations governing professional coding and documentation; develops and updates procedure manuals to maintain standards for correct coding, minimizes the risk of fraud and abuse and optimizes revenue recovery. Research and analyze data, draw timely conclusions, and resolve issues; read, interpret and apply policies, procedures, laws and regulations; read and interpret medical procedures and terminology; develop reports and related documents; maintain working relationships with physicians and other staff; review the work of others; maintain confidentiality, influence/coordinate efforts of others over whom one has no direct authority. Other duties as assigned. Job Knowledge: Advance knowledge of medical terminology abbreviations, techniques and surgical procedures; anatomy and physiology, major disease processes, pharmacology, and the metric system to identify specific clinical findings, to support existing diagnoses, or substantiate listing of additional diagnoses in the medical record. Advance knowledge of medical codes involving selections of most accurate and descriptive codes using the ICD-9-CM, ICD-10-CM, Volumes 1-3, CPT, HCPCS and IHS coding conventions. Skill in correlating generalized observations/symptoms (vital signs, lab results, medications, etc.) to a stated diagnosis by assigning the correct ICD-9-CM and ICD-10-CM codes. Advance knowledge of medical codes involving selection of most accurate and descriptive codes using the CPT codes for billing of third party resources. Extensive knowledge of official coding conventions and rules established by the AMA and the Center for Medicare and Medicaid Services (CMS) for assignment of diagnostic and procedure codes. Knowledge of RPMS and IHS Electronic Health Record (EHR) in order to analyze encounters and notify providers of data that needs corrections through EHR broadcasts, notifications and templates. Must have good math skills; effective written and oral communication skills. Must be proficient in Microsoft Office Suite. Minimum of two years working in a Medical Clinical billing office Education and Experience: Must have good math skills; effective written and oral communication skills. Must be knowledgeable of the fiscal requirements, policies and procedures of federal, state and commercial payers. Must be proficient in Microsoft Office Suite Must be able to follow instruction and work independently.