endocrine system text
advertisement

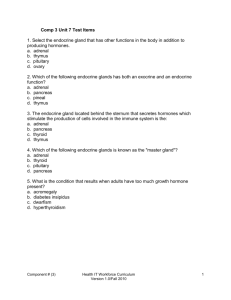
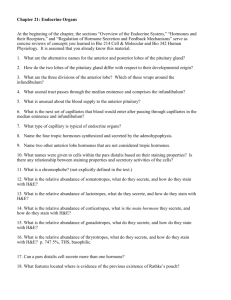
ENDOCRINE ORGANS. I. General background on endocrine organs. A. Endocrine glands are a group of organs that synthesize and release hormones into capillaries. These hormones affect the function of other target organs or tissues in the body. B. Often there are interactions between the hormone(s) and the nervous system. 1. So we can say that the nervous system and the endocrine system are each affected by and modulate the activities of the other. 2. Thus, the nervous and endocrine elements of control are often lumped together under the heading neuroendocrine system. II. Pituitary gland = Hypophysis - an endocrine organ with obvious neural and non-neural endocrine components A. Embryological development 1. Neural hypophyseal tissue (derived from a portion of the forming brain called the infundibulum of the diencephalon) 2. Non- neural hypophyseal tissue (derived from the external epithelial lining of a structure called Rathke’s pocket in birds and mammals) 3. Together these tissues form the hypophysis = pituitary gland a. Diencephalic infundibulum forms neurohypophysis * pars nervosa = neurohypophysis = posterior lobe * Continuous with hypothalamus of brain at the median eminence. median eminence b. The epithelial lining of Rathke's pocket forms the adenohypophysis = non-neural hypophysis = anterior lobe * This is composed of 3 major parts. ** pars distalis (anterior lobe) - largest component of adenohypophysis median eminence ** pars intermedia - lies between neurohypophysis and pars distalis. ** pars tuberalis - adenohypophyseal tissues that surround the stalk of the pars nervosa. B. Cardiovascular circulation to the pituitary gland 1. Since these tissues secrete hormonal substances, we would expect a well developed vascular system that would provide a means of circulating these hormones to other parts of the body. 2. Five arteries provide blood to the pituitary gland. these are, a. 2 superior hypophyseal arteries b. 2 inferior hypophyseal arteries. c. Trabecular artery 3. These arteries enter the pars nervosa, the pars tuberalis, and the median eminence region of the hypothalamus where they form a capillary network. 4. The capillaries merge to form venules and veins B. Cardiovascular circulation to the pituitary gland 5. In the case of the pars nervosa, the blood exits these tissues via neurohypophyseal veins. 6. Venules that form from capillaries in the median eminence extend through the pars tuberalis, enter the pars distalis, and form a second capillary network (a portal system) within its tissue = hypophyseal portal system. 7. These capillaries coalesce to form venules and veins that then leave the pars distalis via adenohypophyseal veins 8. Why might this be? The hypophyseal portal system carries hormones from the median eminence of the basal hypothalamus to the pars distalis where they have an effect on the secretion of hormones by cells in that part of the pituitary gland. Median eminence III. Adenohypophysis (pars distalis) Tissue structure and cell types. A. Has typical appearance of endocrine tissue, that is groups of cells organized into cords or follicles B. Through this tissue run fenestrated capillaries that are part of hypophyseal portal system. http://www.vh.org/Providers/Textbooks/ MicroscopicAnatomy/Section15/Plate15279.html C. Two major classes of cells are present in the pars distalis. These are the chromophobes and chromophils. Classification is based on staining characteristics. 1. Chromophobes a. cytoplasm doesn’t pick up stain b. cytoplasm appears white or clear in stained sectioned material c. This group of cells includes the * Cells that form a supporting meshwork for the tissues of the adenohypophysis. * Secretory cells that are thought to secrete hormones, but that are not well understood at present. ** One type of chromophobe in rats secretes adrenocorticotropic hormone that stimulates the adrenal gland. (However, in humans this hormone is produced by a basophilic chromophil - see below.) http://www.vh.org/Providers/Textbooks/ MicroscopicAnatomy/Section15/Plate15279.html http://www.lab.anhb.uwa.edu.au/mb140/ 2. Chromophils - these cells pick up basic or acidic stains basophils and acidophils a. Basophils * Gonadotropic cells ** Secrete hormones that affect reproductive organs (follicle stimulating hormone, FSH; leuteinizing hormone, LH; interstitial cell stimulating hormone, ICSH). *** FSH - glycoprotein that stimulates and supports early growth of follicles in ovary and spermatogenesis in testis. *** LH - glycoprotein that reaches peak during menstrual cycle. 24 hr after peak, ovulation occurs. *** ICSH = LH in males - stimulates interstitial cells of Leydig in testes to secrete testosterone http://www.lab.anhb.uwa.edu.au/mb140/ 2. Chromophils a. Basophils * Gonadotropic cells (cont.) ** Small round cells with dense, basophilic, secretory granuals ** Distributed throughout pars distalis. ** FSH and LH secreting cells test positive with the periodic acid schiff (PAS) stain because the hormones are glycoproteins. * Thyrotropic cells ** Secrete thyroid stimulating hormone =thyrotropin (TSH)- stimulates synthesis of thyroid hormones. ** Positive PAS because hormone is a glycoprotein. http://www.lab.anhb.uwa.edu.au/mb140/ b. Acidophils * Mammotropic cells - secrete prolactin ** Peptide hormone that triggers secretion of milk by mammary glands. * Somatotropic cells ** Secrete Growth hormone = somatotropin (STH)- protein hormone. *** Most marked affect is on epiphyseal cartilage of bone, hormone acts on liver to cause production of a peptide called somatomedin. This peptide stimulates growth of epiphyseal plate. Lack of this hormone results in hypopituitary dwarfism which can be treated in some cases with hormone injections. Overproduction of STH can cause gigantism and may eventually result in acromegaly. http://www.lab.anhb.uwa.edu.au/mb140/ D. As discussed earlier, secretion of hormones by cells of the pars distalis is caused by the action of hormonal factors synthesized in the hypothalamus and secreted in the median eminence. These are called releasing factors, e.g. growth hormone releasing factor (GHRF), gonadotrophic releasing hormone (GnRH). E. In many cases the hypothalamus, hypophysis, and affected organ work in concert with positive or negative feedback occurring between all three. F. READ ABOUT OTHER PARTS OF THE ADENOHYPOPHYSIS (pars intermedia, pars tuberalis) IN TEXT. IV. Neurohypophysis -Tissue structure and cell types of the pars nervosa A. This is the posterior lobe of the pituitary gland that is formed from the tissues of the diencephalic infundibulum. Recall that these tissues remain attached to the part of brain that is the hypothalamus. B. The body and stem of the pars nervosa are mainly composed of unmyelinated axonal processes and associated glial cells. 1. The axons arise from neuron perikarya that are located in the supraoptic and paraventricular nuclei of the hypothalamus. • Some axons from these neurons end blindly (no synapse) in the median eminence of the hypothalamus • Other axons extend into the lower regions of the posterior lobe of the pituitary where they also end blindly. Median eminence 2. These hypothalamic cells are neurosecretory neurons that synthesize hormones such as oxytocin, vasopressin (lower posterior lobe), and the various releasing factors (median eminence) mentioned above. These substances accumulate in the blind endings of these axons that are located in the pars nervosa or median eminence). In the case of vasopressin and oxytocin. a. Major effect of vasopressin is to increase permiability to water of the tubules of the kidney. Causes a higher rate of reabsorption of water by these tubules and thus concentrates the urine. b. Oxytocin promotes contraction of the smooth muscle of the uterine wall during copulation and parturition. Also, contraction of myoepithelial cells that surround ducts of the mammary glands. * In the case of child birth and intercourse, distension of the vagina excites stretch receptors in the vaginal wall. These cause action potentials to be sent to the CNS where the appropriate neurosecretory cells of the hypothalamus receive nervous stimulation and release oxytocin in the pars nervosa. This hormone enters the circulatory system and is carried to the muscles (myometrium) of the uterine wall where it causes these muscles to contract. Median eminence 3. So the the hypothalamus is actually a component of the posterior pituitary's endocrine function since the actual hormones are synthsized there and then released into or stored in the median eminence and pars nervosa respectively. C. Accumulations of oxytocin or vasopressin in the blind endings of axons in the pars nervosa form the Herring corpuscles (bodies) seen in the lower posterior lobe with the light microscope. http://www.lab.anhb.uwa.edu.au/mb140/ D. To sum it up - When appropriate neural stimulation of the neurosecretory cells occurs, the blind endings of the axons release their secretory products which enter capillaries in the pars nervosa (oxytocin, vasopressin) or median eminence region (releasing hormones). The hormones are then carried to their point of action in other parts of the body (oxytocin, vasopressin) or to the adenohypophysis (releasing hormones). E. In addition to axons, you will also find the nuclei of pituicytes in the tissues of the pars nervosa. 1. These cells are of irregular shape and often have numerous cytoplasmic processes. 2. They are considered a type of glial cell, but their function is not well understood. http://www.lab.anhb.uwa.edu.au/mb140/ V. Adrenal glands -Paired organs that usually lie on the superior poles of the kidneys, embedded in adipose tissue. A. General structure 1. Covered by capsule of dense collagenous connective tissue. 2. Thin septa or trabeculae extend from the connective tissue capsule into the interior of the gland. 3. Internally there are two major regions called the adrenal cortex and adrenal medulla. 4. The supporting framework of cortex and the medulla is collectively called the stroma. This framework is mainly composed of reticular fibers. http://www.ucs.mun.ca/~fking/adrenal/slide3.html http://education.vetmed.vt.edu/Curriculum/ VM8054/Labs/Lab24/Examples/exadrenl.htm B. Embryological development 1. In a sense, the adrenal cortex and medulla may be considered as 2 morphologically distinct endocrine organs. 2. Similar to what we saw in the hypophysis, the cortical and medullary portions of the adrenal glands have different embryonic origins. That is to say, they are derived from different basic tissue types in the embryo. 3. Again, we have a situation where neural and non-neural tissues become associated to form an organ (neural ectoderm and mesoderm). a. As an embryo develops, the cortex of the adrenal gland is derived from mesodermal cells in the region of the kidney. http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/ Lab24/Examples/exadrenl.htm b. The cells of the adrenal medulla are derived from a specialized group of neural ectoderm cells that are called the neural crest. * The neural crest cells separate from the developing CNS and migrate through the body's tissues giving rise to a number of different cell types including many of the peripheral ganglion neurons. * Some of the neural crest cells migrate to the developing adrenal cortex, penetrate this mesodermal tissue and lodge themselves centrally within it to form the adrenal medulla. * So, the secretory cells of the adrenal medulla can be thought of as postganglionic neurons that have lost their axons and dendrites and have become secretory cells. http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/ Lab24/Examples/exadrenl.htm C. Caridovascular circulation of the adrenyl gland. 1. Blood is supplied to the adrenal glands by a number of arteries. 2. These vessels enter through the capsule tissue and then branch out into a sub-capsular plexus of arterioles that give rise to capillaries that extend throughout the cortex. 3. The capillaries supply blood to a network of sinusoids in the cortex. 4. Some of the arterial branches do not form capillaries in the cortex, but rather run through it to the medulla. a. These are the medullary arteries. b. They form a dense capillary network around the cells of the medulla. http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/ Lab24/Examples/exadrenl.htm http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/adre nal/histo_overview.html 5. If we look at the endothelium of the capillaries, we find it is fenestrated with the fenestrations being occluded by a thin membrane (diaphragm). In the cortex, the basal lamina of the endothelium is not continuous - set-up for the exchange of materials between the blood and surrounding cells or visa versa. 6. Capillaries of medulla and cortex coalesce to form the adrenal veins that exit the adrenal glands. http://education.vetmed.vt.edu/Curriculum/ http://arbl.cvmbs.colostate.edu/hbooks/pathphys/ VM8054/Labs/Lab24/Examples/exadrenl.htm endocrine/adrenal/histo_overview.html D. Adrenal cortex http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/ Lab24/Examples/exadrenl.htm 1. Composed of 3 layers a. zona glomerulosa b. zona fasciculata c. zona reticularis http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/adrenal/histo_overview.html Adrenal http://www.lab.anhb.uwa.edu.au/mb140/ Corticosteroid Folded cords mineralocorticoids cortisol Straight cords cortisol, androgens, progesterone, estrogen irregular cords ______ 2a. Zona glomerulosa - structure a. Columnar to pyramidal cells that are arranged in folded cords surrounded by capillaries/sinusoids. b. Cells have spherical nuclei and basophilic granules in cytoplasm. c. Where cells are adjacent to the endothelium of the capillaries and sinusoids, there is a space between the cell plasmalemma and the endothelium. d. The plasmalemma of these cells is thrown into folds (microvilli) that extend into the space. http://www.medinfo.ufl.edu/year1/histo/images/f24b.jpg 2b. Zona glomerulosa - function a. The zona glomerulosa cells secrete mineralcorticoids, mainly aldosterone which is important in maintaining water balance. b. These and other corticoid hormones are steroid hormones that are lipid molecules derived from cholesterol. http://www.finchcms.edu/anatomy/histology/organology/endocrine/images/ff954.jpg http://www.leeds.ac.uk/bms/teaching/histology/pcd1855/img0014.jpg c. Ultrastructure is typical for cells involved in lipid synthesis (see 3. below). * Lots of smooth endoplasmic reticulum with a few short segments of RER. * Well developed Golgi body. * Mitochondria are spherical or oval and have tubular cristae. * Lipid droplets may be present in cytoplasm associated with smooth endoplasmic reticulum. 3a. Zona fasciculata - structure a. Cells are polyhedral and are arranged in straight cords (columns), 1-2 cells thick with capillaries running between. b. Cells have central spherical nucleus with basophilic cytoplasm. Microvilli in plasmalemma are present within the subendothelial space (next to the capillaries). c. Many lipid droplets present in cytoplasm. These are extracted during most embedding procedures, so the cells often appear highly vaculated. b. Ultrastructure is typical for cells involved in lipid synthesis and secretion (as discussed earlier) * However, these cells have more RER than those of the zona glomerulosa * This, in addition to the presence of many lipid droplets, is why the cytoplasm has a weak overall basophilic affinity - but usually does not stain heavily. http://www.finchcms.edu/anatomy/histology/organology/endocrine/images/ff958.jpg http://www.med.uiuc.edu/histo/small/atlas/image/tem8/21700a1.htm 3b. Zona fasciculata - function a. Zona fasciculata cells secrete glucocorticoids, mainly cortisol (important in regulation of lipid, protein and carbohydrate metabolism). Another type of steroid. Also sex hormones (e.g. androgens, estrogen, progesterone) b. Also may secrete a weak androgen dehydroepiandrosterone (DHEA). http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab24/Examples/exadcort.htm http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab24/Examples/exadcort.htm 4a. Zona reticularis - structure a. Cells are polyhedral with spherical nucleus and are arranged in irregular cords with capillaries and sinusoids between. b. Lipofuscin pigment granules in cells. c. Cytoplasm acidophilic. http://www.leeds.ac.uk/bms/teaching/histology/pcd1855/img0013.jpg 5. Secretion of steroids by adrenal cortex is good example of a feedback system between target organ and pituitary gland. a. A psychological stimulus such as stress, exercise, causes neurosecretory neurons in the hypothalamus to secrete adrenocorticotropic hormone releasing factor into the capillaries in the median eminence. b. The releasing factor is carried by the hypophyseal portal system from the median eminence to the pars distalis. c. This causes corticotrophic cells in the pars distalis to secrete adrenocorticotropic hormone (ACTH - also called adrenocorticotropin) into surrounding capillaries. d. The ACTH is carried to the adrenal glands where it causes an increase in cortisol secretion by adrenal cortex cells of the zona fasciculata and zona reticularis. e. As levels of cortisol increase in blood, these inhibit both the secretion of releasing factors by the hypothalamus and secretion of ACTH by pituitary. http://www.finchcms.edu/anatomy/histology/organology/end ocrine/o_e_4.html E. Adrenal medulla 1. Composed of irregular cords of polyhedral, epithelioid, secretory cells that form a compact irregular network surrounded by capillaries, venules, and a few sympathetic ganglion cells/neurons (blue arrows). 2. The epithelioid secretory cells are considered to be modified postganglionic sympathetic neurons. http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab 24/Examples/exadrmed.htm http://www.medinfo.ufl.edu/year1/histo/images/g4b.jpg 3. Axons from preganglionic sympathetic neurons synapse on the surface of the secretory cells. a. When stimulated , these axons release acetylcholine (cholinergic synapses) that causes the exocytosis of secretory granules at the apical end of the secretory cells. b. The secretory product consists of the catecholamines epinephrine (adrenaline), norepinephrine (noradrenaline) or dopamine. c. Three different types of cells, one for each catecholamine. http://webpages.ull.es/users/isccb12/ChromaffinCell/Primer.html d. Secretory granules stain a brown color with chromium salts - called chromaffin reaction. As a result, these cells are called chromaffin cells. http://www.finchcms.edu/anatomy/histology/organology/endocrine/o_e_4.html 4. Adrenal medulla secretes continuously into blood stream. a. The adrenal medulla cells secrete only small amounts of epinephrine and norepinephrine unless stimulated by nervous activity related to emotional reactions. b. Secretion of these substances prepares body to react to stressful situations. Blood vessels constrict, blood pressure rises, etc. VI. Thyroid A. Located below the larynx, partially encircling the esophagus. http://www.endocrineweb.com/thyroid.html http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrin e/thyroid/anatomy.html B. Thyroid is covered by layer of loose connective tissue. interfollicular 1. Surrounded by a connective tissue capsule that extends septa into the interior separating lobes (lobules) of follicles (interlobular C.T.) a. This C.T. also extends between the follicles separating them from each other (interfollicular C.T.). b. Septa that separate follicles are composed mainly of reticular fibers. 2. Arterioles and venules may be found within the C.T. These are connected by fenestrated capillaries amongst the follicles. http://www.lab.anhb.uwa.edu.au/mb140/ http://www.finchcms.edu/anatomy/histology/organology/endocrine/images/ff934.jpg C. The thyroid tissue of the lobes is composed of follicles, each containing a lumen filled with a gelatinous substance - colloid. 1. Each follicle consists of a simple cuboidal epithelium surrounding the lumen a. The epithelium changes to simple squamous if the follicle is inactive. http://www.vh.org/Providers/Textbooks/MicroscopicAnatomy/ Section15/Plate15287.html 2. Cells of follicles are responsible for synthesis of thyroid hormones, the most abundant of which is thyroxin. a. Colloid consists of mainly iodinated thyroglobulin. b. When hormones required, iodinated thyroglobulin in colloid is endocytosed. c. Endocytotic vesicles merge with lysosomes. d. Lysosomal enzymes break iodinated residues off and process thyroglobulin => thyroid hormones e. This liberates the thyroid hormones into the cytoplasm. f. These diffuse across the cell membrane into capillaries where blood carries them to target organs. http://arbl.cvmbs.colostate.edu/hbooks/ pathphys/endocrine/thyroid/anatomy.html g. Thyroxine stimulates mitochondrial respiration and oxadative phosphorylation. So, more ATP produced faster. http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/synthesis.html 3. In addition to follicle cells, parafollicular cells (C cells, clear cells) are found between the follicles in humans and other mammals. a. These cells secrete the polypeptide calcitonin that causes a reduction of calcium in the blood, in part by inhibiting the activities of osteoclasts. http://www.vh.org/Providers/Textbooks/MicroscopicAnatomy/S ection15/Plate15287.html 4. Control of thyroid hormone secretion: a. Stimuli provided by axons from parasympathetic and sympathetic ganglia can influence metabolism of thyroid cells. b. However, thyrotropin (thyroid stimulating hormone, TSH) is the major controlling factor. c. Thyrotropin is synthesized and secreted by cells of the adenohypophysis (pars distalis). d. Thyroid has feedback system with pituitary similar to adrenal cortex. * Releasing factors from the neurohypophysis cause the adenohypophysis to secrete thyrotropin. * This causes thyroid hormone production by the follicle cells of the thyroid. * As thyroxin level rises in the blood, it causes an inhibition of the secretion of releasing factors by the neurohypophysis and, thus, less thyroxin is secreted. Hyperthyroidism Excess of thyroid hormone resulting from an overactive thyroid gland (or taking too much thyroid hormone). Symptoms can include increased heart rate, weight loss, depression, and cognitive slowing. Histologically, the follicles are small and there is considerable scalloping around the edges of the colloid due to overproduction of thyroid hormones. Lymphatic nodules may also be present in the thyroid tissue. http://mspis.medsci.indiana.edu/c602web/602/C602web/endo/slide12.htm VII. Parathyroid glands http://arbl.cvmbs.colostate.edu/hbooks/ http://www.endocrineweb.com/thyroid.html pathphys/endocrine/thyroid/anatomy.html A. These are small, but important, organs that are embedded in the wall of the thyroid. 1. History - complete removal of the thyroid gland was noted to cause death because of spasms of the laryngeal and thoracic muscles that prevented breathing - called tetany 2. In 1892, the French physiologist Gley showed that it was actually the removal of the parathyroid glands that "rode" along with the thyroid that caused of these titanic seizures. (due to the lack of parathormone) 3. Thus, when the thyroid is removed, it is critical that the parathyroid glands be separated from it and left in the body. B. There are three cell types in the parathryroid glands 1. Adipose cells - increase in number as one grows older. http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrin e/thyroid/anatomy.html http://www.lab.anhb.uwa.edu.au/mb140/ 2. Chief cells a. polygonal with vesicular nucleus b. cytoplasm slightly acidiphilic, pale staining cytoplasm c. secrete parathyroid hormone (parathormone). 3. Oxyphil cells a. Not present at birth b. start appearing in parathyroid tissues at about age 7 in humans http://www.finchcms.edu/anatomy/histology/ organology/endocrine/images/ff941.jpg c. acidophilic cytoplasm (due to many mitochondria) d. no known function e. Similar to, but larger than chief cells. http://www.lab.anhb.uwa.edu.au/mb140/ C. Major function of parathyroid glands 1. Parathyroid hormone (parathormone) causes increase in calcium in the blood by promoting the activities of osteoclasts in the breakdown of calcified bone matrix. (Remember c-cells in thyroid that secrete calcitonin?) D. Calcitonin of thyroid parafollicular cells (C cells) and parathyroid hormone (parathormone) of chief cells balance and regulate calcium levels in the body.