ENDOCRINE SYSTEM
advertisement
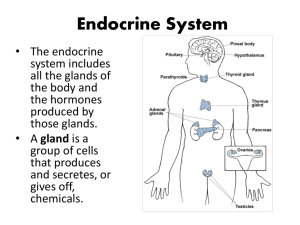
ENDOCRINE SYSTEM Ⅰ. Introduction A. Consists of individual endocrine glands, and diffuse endocrine cells that are present i n other organs. Together with the nervous system, it regulates different functions of th e body. B. Endocrine glands -- thyroid, parathyroids, adrenals, pituitary and pineal glands 1. Endocrine glands are ductless. 2. Cells arranged in glomerulus, cords, reticulum or in follicles. 3. Rich in blood and lymphatic capillaries between cells. 4. Release hormones either into the vascular system (endocrine), or to their surroundin gs (paracrine), and bind to specific receptors of target cells. C. Endocrine cells – 2 types according to chemical nature of hormones released 1. Nitrogen-containing hormone-secreting cells a. Found in thyroid, parathyroids, adrenal medulla, pituitary and pineal glands, etc. b. Contain RER, Golgi complex and membrane bound secretory granules. c. Hormones are secreted by exocytosis. 2. Steroid hormone-secreting cells a. Found only in adrenal cortex and ganads. b. Contain abundant SER, mitochondria with tubular cristae and lipid droplets. c. Hormones are secreted by diffusion. Ⅱ. Thyroid – largest endocrine gland A. General structure 1. Thin capsule of loose connective tissue sends septa into parenchyma, dividing the gl and into lobules. 2. Each lobule consists of follicles, which are functional units and varied in size. 3. Between follicles is a delicate connective tissue rich in fenestrated capillaries. 4. The thyroid also contains parafollicular cells. B. Thyroid follicles 1. Composed of a simple epithelial sphere whose lumen contains colloid. 2. Follicular epithelial cells a. Height of cells ranges from squamous to columnar, depending on the functional acti vity of follicles. b. The cytoplasm is weakly basophilic or acidophilic. c. Ultrastructure: ①Apical surface is covered by numerous microvilli. ②Cytoplasm rich in RER in basal part, well-developed Golgi complex in supranuclear ar ea, secretory granules and pinocytotic colloid vesicles in apical part and abundant lysos omes. ③Cells are joined laterally by junctional complexes, preventing thyroglobulin leakage fro m follicles into surrounding stroma. 3. Colloid a. Homogeneous, acidophlic, gelatinous substance. b. Chemical composition is iodinated thyroglobulin. c. Vacuoles at the periphery may represent pinocytosis of colloid. 4. Function: synthesis and release of thyroid hormones (T3, T4) a. The process involves: ①Synthesis of thyroglobulin (TG) in RER and Golgi apparatus. TG is transported in secr etory granules and released into lumen of follicles. ②Iodination of TG. Follicular cells take up circulating iodide, which is activated via oxid ation by peroxidase and combines at the microvillus-colloid interface with tyrosine resid ues of TG. ③Storage. The iodinated TG is stored as colloid in the follicular cavity. ④Pinocytosis. When stimulated by thyrotropin, follicular cells take up iodinated TG from the cavity, forming pinocytotic vesicles. ⑤Liberation of T3 & T4. Pinocytotic vesicles then fuse with lysosomes and iodinated TG is degraded by proteases into free thyroxine (T4) and triiodothyronine (T3), which are released into fenestrated capillaries. b. T3 and T4 increase rate of metabolism and influence development of central nervous system during fetal and neonatal life. C. Parafollicular cells or C cells 1. Located between follicular epithelial cells or between follicles as isolated clusters. 2. Large and pale stained with H & E, argyrophilic granules with silver staining. 3. Under EM, many small secretory granules. 4. Secrete calcitonin, which lowers blood calcium level by inhibiting bone resorption of osteoclasts and osteocytes. Ⅲ. Parathyroid glands A. Consist of 2 types of cells: Chief cells are small, pale stained and contain secretory granules; oxyphil cells are large, acidophilic because of many mitochondria. B. Parathyroid hormone secreted by chief cells elevates blood calcium by increasing act ivity of osteoclasts. Ⅳ. Adrenal glands A. General description 1. Covered by a capsule of dense connective tissue, which, with abundant sinusoids, ex tends into the interior of glands. 2. Parenchyma consists of an outer adrenal cortex derived from mesoderm, and an inn er adrenal medulla from the neural crest. 3. The cortical cells are steroid-secreting, and the medullar cells are nitrogen hormonesecreting. B. Adrenal cortex -- subdivided into three layers according to cell arrangement 1. Zona glomerulosa a. Beneath the capsule, occupy 15% of total volume of the glands. b. Composed of round clusters of columnar cells surrounded by capillaries. c. Secrete mineralocorticoids, primarily aldosterone, which maintain electrolyte and wat er balance by acting on distai renal tubules and stimulating resorption of sodium. 2. Zona fasciculata a. Most thick layer in middle account for 65% of total volume of glands. b. Composed of straight cords of large, polyhedral cells with acidophilic, sponge cytopla sm. c. Cells have typical ultrastructural characteristics of steroid-secreting cells. d. Synthesize glucocorticoids: mainly cortisol and corticosterone, which regulate carboh ydrate, protein and lipid metabolism, and also suppress immune responses. 3. Zona reticularis a. Innermost layer of smaller cells arranged in anastomosing cords, 7% of total volume. b. Produce sex hormones, mainly androgens, and small amounts of cortisol. C. Adrenal medulla 1. Composed of polyhedral cells arranged in nests or short cords. 2. Cells contain chromaffin granules, so called chromaffin cells. 3. Synthesize and release epinephrine and norepinephrine by 2 different groups of cells. 4. Epinephrine increases the heart rate. Norepinephrine increases the blood pressure an d blood flow to the heart, brain and skeletal muscle. Ⅴ. Pituitary Gland (hypophysis) – master gland regulating other endocrine glands A. Introduction 1. Consists of two parts: adenohypophysis develops from oral ectoderm, and neurohyp ophysis from neuroectoderm. 2. The adenohypophysis includes 3 parts: pars distalis or anterior lobe, pars intermedia, and pars tuberalis. 3. The neurohypophysis includes 3 parts: pars nervosa or posterior lobe, infundibular st alk and median eminence. Pars nervosa and pars intermedia make up posterior lobe. B. Pars distalis – largest part containing 3 types of cells interspersed with sinusoids 1. Acidophil cells – 40% a. Round or ovoid, exhibiting acidophilic, and numerous coarse secretory granules unde r EM. 2 types of acidophil cells. b. Somatotrophs synthesize and release growth hormone, which stimulates body growt h, particularly growth of long bones. c. Mammotrophs secrete prolactin, which initiates and maintains the milk secretion afte r pregnancy. 2. Basophil cells – 10% a. Slightly larger than acidophil cells, with basophilic cytoplasm. 3 types with EM and i mmunohistochemical techniques. b. Thyrotrophs secrete thyrotropin or thyroid stimulating hormone (TSH), which stimula tes growth of thyroid follicles and synthesis and release of thyroid hormones. c. Corticotrophs secrete adrenocorticotrophic hormone (ACTH), which stimulates secretio n of glucocorticoids from zonae fasciculata and reticularis of adrenal cortex. d. Gonadotrophs secrete follicle-stimulating hormone (FSH) and luteinizing hormone (L H). FSH promotes ovarian follicle development in females and spermatogenesis in male s. LH promotes ovulation and development of the corpus luteum in women and, Leydin g cell stimulation and androgen secretion in men. 3. Chromophobe cells – 50% a. Clusters of small cells without distinct boundaries, and pale stained. b. Few secretory granules, indicating they are undifferentiated precursor cells or degran ulated chromophils. C. Pars intermedia 1. Composed of chromophobes and basophil cells arranged either in cords or in colloidcontaining follicles. 2. Secretes melanocyte stimulating hormone (MSH) in fish and amphibia. D. Pars tuberalis 1. Surrounds the infundibulum, and cells arranged in cords separated by sinusoids. 2. Most cells secrete FSH and LH in humans. E. Relationship between pars distalis and hypothalamus 1. Activities of the cells in the pas distalis are controlled by hypothalamic neuroendocri ne neurons that produce peptide releasing hormones and inhibitory hormones, which ar e transported to the pars distalis through the hypophyseal portal system. 2. Hypophyseal portal system includes a. Primary capillary plexus in the stalk and median eminence, formed by superior hypo physeal arteries. b. Hypophyseal portal veins joined in pas tuberalis from primary plexus. c. Secondary capillary plexus in pas distalis, formed from portal veins. F. Neurohypophysis 1. Contains large numbers of unmyelinated nerve fibers, sinusoids, pituicytes. 2. Unmyelinated nerve fibers contain neurosecretory granules, which often accumulate i n dilated portions, Herring bodies, of the axons. They originate from neurons of hypoth alamic supraoptic and paraventricular nuclei. 3. Pituicytes are glial cells with irregular shape and short processes contain lipid drople ts and pigment granules in their cytoplasm. 4. Function: stores and releases vasopressin (antidiuretic hormone, ADH) and oxytocin. a. Vasopressin stimulates water resorption in kidneys and contraction of vascular smoot h muscle. b. Oxytocin promotes contraction of uterine smooth muscle during parturition and contr action of myoepithelial cells in mammry glands during lactation.