Neuwelt_Lecture_5.28.09
advertisement

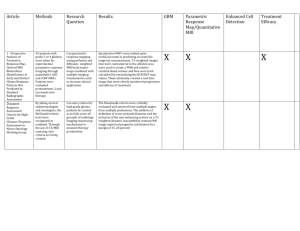
The problem of the BBB The Blood-Brain Barrier limits delivery of chemotherapy and other therapeutics to the CNS Edward Neuwelt, MD Advanced Topics in Cancer Biology Oregon Health & Science University May 28, 2009 Cerebral Circulation 675 km of veins, arteries, and capillaries BBB consortium clinical research 1. Increase chemotherapy delivery and efficacy in brain tumors Example: PCNSL 2. Decrease chemotherapy side effects Example: ototoxicity 3. Imaging vascular targeted therapies with iron oxide nanoparticles: Is “less” better? Treatment of Patients with Newly Diagnosed PCNSL: BBBD Consortium Results Introduction to PCNSL • An aggressive non-Hodgkin’s lymphoma, usually B-cell origin • Diffuse CNS disease; may involve the brain, spinal cord, leptomeninges and eyes at presentation • Represents approx. 4% of intracranial neoplasms Treatment of PCNSL patients • The optimal treatment is unknown • HD Methotrexate (MTX) widely accepted as the most effective chemotherapy • Combined-modality therapy (HD MTX and WBRT) has improved response rates, PFS and OS • However, combined therapy is associated with a high incidence of delayed neurocognitive toxicity, especially in patients > 60 years Introduction to BBBD PCNSL lesion (leaky BBB) PCNSL lesion after BBBD (temporary opening of brain around tumor) Neuropsychological Outcome in Primary CNS Lymphoma Patients Multi-Center BBBD Study Eligibility Criteria: • BBBD treatment (MTX-based) within 90 days of diagnosis • No prior WBRT • No evidence of systemic lymphoma at diagnosis • HIV-1 negative J Clin Oncol in press 2009 Patient characteristics • N = 149 (78 Female/71 Male) • Disease site: CNS (131 pts, 88%), CNS and IO (15 pts), intra-ocular only (3 pts) • CSF cytology: Neg (96 pts, 64%), atypical (14 pts), Pos (11 pts), Unknown (28 pts) J Clin Oncol in press 2009 Outcome • Overall response rate: 81.9% (57.8% CR; 24.2% PR) • Median OS: 3.1 yrs (41% est. at 5 yrs; 25% at 8.5 yrs) J Clin Oncol in press 2009 J Clin Oncol in press Efficacy and MRI of rituximab and methotrexate treatment in a nude rat model of CNS lymphoma Neuro-Oncology. Epub ahead of print. January 21, 2009 MRI and histology of the rat CNS lymphoma model In vitro toxicity of methotrexate MTX was toxic in MC116 human B-lymphoma at low doses in vitro Efficacy of tumor treatment Rituxan reduced rat CNS lymphoma tumor volume on MRI MTX blocked tumor growth Combination therapy was NOT effective Does IV methotrexate decrease response to IV rituxan by restoring the BBB? Q: Does Rituxan cross the BBB? A: Yes and No Summary • BBBD chemotherapy can be conducted with acceptable toxicity, however the treatment is complex and should be undertaken only by trained teams • Results with BBBD/IA MTX demonstrate comparable if not superior outcomes (durable response rates, PFS, OS) to HD IV MTX as well as to combination MTX and WBRT without the neurocognitive sequelae of WBRT • BBBD provides the opportunity to deliver effective monoclonal antibody/chemotherapy regimens and other novel agents to the CNS In press, J Clin Oncol 2009 Cisplatin ototoxicity • Overall incidence cisplatin ototoxicity: 50-70% • High frequency hearing loss initially, progresses with continued treatment • Unable predict hearing loss based on dose or plasma levels of platinum Blakely 1993 Treatment Dilemma • Ototoxicity is dose-limiting • Reducing the cisplatin dose stabilizes hearing loss • However, dose reductions may affect efficacy of treatment • Need strategies that can reduce/prevent hearing loss without interfering with chemotherapy Patients Received Carboplatin, No STS Maximum AC Cochlear Potential STS Otoprotection Carboplatin in the Guinea Pig 500 400 300 200 100 0 STS 2 hrs STS 4 hrs STS 8 hrs STS 24 hrs saline Problems with Chemoprotection Potential to reduce the anti-tumor activity of chemotherapy Anti-tumor Efficacy in the Presence of Chemoprotection Tumor volumes were assessed 6 days after nude rats with intracerebral tumors were treated with or without BBBD chemotherapy alone or in combination with thiols NAC and/or STS. Bar graph shows tumor volumes in n = 8 per group. Tumor volume (mm3) Anti-tumor Efficacy in the Presence of Chemoprotection 30 20 TREATMENT GROUPS 1: Tri-drug BBBD 2: Tri-drug + STS 3: NAC + Tri-drug 4: NAC+ Tri-drug +STS 5: Untreated 10 0 1 2 3 4 5 Treatment Group Bar graph shows tumor volumes in n = 8 per group. Do Thiols Protect Tumor? Not if separated from chemo in time and space Metastatic Ovarian Patient Received Carboplatin + STS STS Otoprotection in Adults Historical patients, no STS (n = 19) STS 2 hr after carboplatin (n = 24) STS 4 hr after carboplatin (n = 17) Hearing loss (dB) 50 40 4&8 kHz 30 20 10 0 1 2 3 4 5 6 7 Treatment with Carboplatin + BBBD Neuwelt et al Chemoprotection may be valuable in the clinical setting if chemotherapy and chemoprotectant can be physically or temporally separated. ACCL0431 A Randomized Phase III Study of Sodium Thiosulfate for the Prevention of Cisplatin-induced Ototoxicity in Children SIOPEL 6 A Randomized Phase III Trial of the Efficacy of STS in Reducing Ototoxicity in Patients Receiving Cisplatin Chemotherapy for Standard Risk Hepatoblastoma Iron oxide nanoparticles as MRI contrast agents Iron oxide nanoparticles Iron oxide core Coated with dextran or other carbohydrate. Molecular Model: Combidex® MRI Iron histochemistry EM reduces toxicity alters plasma half life OHSU experiences with • Iron oxide nanoparticles – Superparamagnetic Iron Oxide (SPIO) – Feridex® – Ultrasmall SPIO (USPIO) – Combidex® (ferumoxtran-10) – Ferumoxytol Imaging inflammatory cells with USPIOs • Iron oxide nanoparticles are taken up by inflammatory cells (B-cells, dedritic cells, macrophages) • Also taken up by activated glial cells in and around CNS tumors GBM Gadolinium vs. Ferumoxtran-10 Presentation number: 10 MAGNETIC RESONANCE IMAGING USING FERUMOXYTOL AND GADOTERIDOL IN PATIENTS WITH CENTRAL NERVOUS SYSTEM INFLAMMATORY DISEASES: PRELIMINARY RESULTS • Dósa E, Hamilton BE, Njus JM, Haluska M, Varallyay CG, • Rooney WD, Nesbit G, Muldoon L, Neuwelt E Departments of Neurology and Neuroradiology, AIRC Oregon Health & Science University, Portland, Oregon, USA May 18, 2009 Benign brain tumor - meningioma Baseline - SWI & T1-w GBCA Ferumoxytol (15 minutes) Ferumoxytol (24 hours) CNS vascular malformation - telangiectasia & cavernoma Baseline - SWI & T1-w GBCA Ferumoxytol (15 minutes) Ferumoxytol (24 hours) Gd vs. USPIO for imaging 9/6/03 T1 9/6/03 T1 Gadolinium 9/16/03 T1 Ferumoxtran-10 12/15/03 T1 Gadolinium Gd vs. USPIO for imaging 10/14/03 10/14/03 Coronal T1 T1 Gadolinium 10/20/03 2/4/04 Coronal T1 Ferumoxtran-10 T1 Gadolinium Demyelinating disease Baseline - T2w GBCA Ferumoxytol (15 minutes) Ferumoxytol (24 hours) Ferumoxytol Ferumoxytol USPIO is a blood pool agent in the early phase • Appropriate for Dynamic MRI • Perfusion measurement is not confounded by BBB permeability • Suggesting more accurate rCBV values Ferumoxytol: an alternative imaging agent for patients at risk for NSF – 1,700 ferumoxytol patients to date (too small to accurately evaluate risk of NSF or other complications) – Ferumoxytol previously tested in patients with renal failure • Over 1700 patients exposed, 1500 with CKD in Phase III iron replacement studies- only 1 patient has experienced anaphylactoid reaction CNS imaging in kidney disease patients: Enhance d safety Ferumoxytol MRI clinical trials Protocol 1. 3 Tesla versus 7 Tesla MRI Dynamic imaging at 3 vs 7 Tesla Ferumoxytol versus gadolinium contrast Protocol 2. Early assessment of tumor response to therapy Dynamic MRI during the course of radiochemotherapy 12 GBM patients Protocol 3. Ferumoxytol in CNS inflammation Ferumoxytol versus gadolinium contrast Utility of ferumoxytol to differentiate inflammatory and neoplastic lesions Subjects include MS, stroke, cardiac surgery Ferumoxytol imaging at 7T in human brain Prior to ferumoxtyol After ferumoxytol What is a perfusion MRI? What contrast agent should we use during perfusion MRI? Signal Intensity MR perfusion: Repeated scans of the same regions after iv. contrast bolus injection Blood Volume Assumes no extravasation Mean Transit Time Time Comparison of gadodiamide and ferumoxytol perfusion Shown is an example using highly vascular and permeable human glioma (U87) rat model in a 12 Tesla MRI. Gadolinium chelates underestimate CBV, perfusion measurement assumes no extravasation. Time of Flight (TOF) Angiography Without contrast 15 min. after GBCA 15 min. post ferumoxytol Perfusion MR, time-intensity curves Signal Intensity Signal Intensity Time gadolinium - leak Time 24 h later ferumoxytol - no leak Hypothesis: Ferumoxytol will show a good safety profile, as well as enhanced imaging, in patients where improved imaging of CNS lesions may improve patient management Preliminary results using DSC-MRI with Ferumoxytol for the purpose of differentiating pseudoprogression from true tumor progression “Pseudoprogression” Subacute treatment-related reactions in human gliomas, showing edema and sometimes new or increasing contrast enhancement on magnetic resonance imaging (MRI) Brandsma, stalpers, Taal et al : Lancet Oncol 2008; 9:453-61 Dynamic Imaging and high Grade glioma Cerebral blood volume is an important prognostic factor Low rCBV High rCBV Materials and Methods • 18 patients with biopsy proven WHO Grade IV glial tumors were prospectively studied in 3 different IRB-approved protocols evaluating dynamic imaging using Ferumoxytol on 3T MRI • In 14 patients, after radiochemotherapy, Gd enhanced MRI and DSC-imaging using Gd and Ferumoxytol were obtained MRI Imaging methods Day 1: Gadolinium injection Anatomical MRI, DSC, DCE, DWI, and MRA Day 2: Ferumoxytol injection Anatomical MRI, DSC, DCE, DWI, and MRA Day 3: No injection Anatomical MRI Treatment of patients with pseudoprogression • Asymptomatic patient continue temozolomide • Symptomatic patient: temozolomide + •Steroid •Bevacizumab (Avastin) •Surgery Pseudoprogression followed by true tumor progression after radiochemotherapy (RCT) 2 mo after RCT Before RCT 25 mo after RCT 28 mo after RCT No contrast A C G J B D H K GBCA E F Gd-rCBV L Fe-rCBV M Gd-rCBV Fe-rCBV Mixed response 1 month after radiochemotherapy (RCT) followed by 2 courses of Bevacizumab Before surgery Before RCT 1mo after RCT After 1 Tx After 2 Tx Gadoteridol A C B Gd-rCBV Fe-rCBV F G Regression after radiochemotherapy (RCT) No contrast Gadoteridol Gd-rCBV Fe-rCBV Before RT A B C D E F G H J K After RT 14 months after RT Comparison of rCBV acquired by DSC-MRI using Ferumoxytol vs Gadoteridol: Tumor vs Pseudoprogression vs Mixed response * * * ** * * P < 0.00001 by ANOVA test ** * * * P = 0.01 by ANOVA test ** Rapidly growing tumors are associated with rCBV > 1.7 in the literature Comparison of rCBV acquired by DSC-MRI using Ferumoxytol vs Gadoteridol GBM cases: Ferumoxytol-rCBV vs Gadoteridol-rCBV 16 14 12 rCBV 10 Fe-rCBV 8 Gd-rCBV 6 p = 0.002 4 * 2 0 1 2 3 4 5 6 7 Patients * Rapidly growing tumors are associated with rCBV > 1.7 in the literature Conclusion • rCBV measurement is possibly more accurate with ferumoxytol than using Gadolinium contrast agents • Increasing gadolinium enhancement on MRI with decreasing rCBV on DSC-MRI using Ferumoxytol may represent pseudoprogression • Improvement can be achieved in symptomatic patients with pseudoprogression by using bevacizumab Avastin versus Steroid Varallyay C, Muldoon LL, Gharamanov S, et al. Dynamic MRI using a blood pool agent ferumoxytol and gadodiamide in evaluating early vascular effects of dexamethasone and bevacizumab in an intracerebral glioma model. J Cereb Blood Flow Metab, In press, 2009. rCBV: Avastin vs. Steroids Permeability: Avastin vs. Steroids Permeability: Avastin vs. Steroids Avastin at 24 h dramatically decreases CNS tumor delivery of Methotrexate 0.1 0.09 0.08 DPM/gm 0.07 0.06 0.05 0.04 MTX alone mean MTX+bev mean 0.03 0.02 0.01 0 Tumor Brain Brain Distal Left Adjacent to to Tumor Hemisphere Tumor Location of Sample Avastin: Is less chemotherapy delivery better? Jahnke K, Muldoon LL, Varallyay CG, et al. Bevacizumab and carboplatin increase survival and asymptomatic tumor volume in a glioma model. Neuro Oncol 2008 Sep 4. [Epub ahead of print] Efficacy of Avastin and Chemotherapy Group Survival (days) Control 16 Bevacizumab 23 Carboplatin 22 BEV + Carbo 36 Avastin synergistically increased the efficacy of chemotherapy in a rat glioma model Increased survival with asymptomatic tumor growth in a rodent model Progression-free survival in patients Questions: • Does Avastin decrease chemo delivery? • Why do patients live longer after Avastin? • Is carbo better than ironotecan? Conclusion Is more better? Depends Future directions in targeting the tumor vasculature Imaging, efficacy, and prophylaxis with anti- VEGF and anti-integrin mAb in intracerebral tumors: Preclinical Studies. Project Aims Aim 1. To determine the effects of antibodies targeting existing tumor vasculature in nude rat brain tumor models. Aim 2. To evaluate the efficacy of targeting antibodies for brain tumor therapy. Aim 3. To assess the potential for antibodies targeted to the CNS vasculature to block the development of CNS metastases. CNS tumor cell localization in the hematogenous metastasis model Vascular localization of Q-dot labeled 231BR-HER2 human breast cancer cells 3 days after intra-carotid infusion. Infiltration of Q-dot labeled 231BR-HER2 breast cancer cells into cerebellum 7 days after intracarotid infusion. MRI of breast cancer brain metastasis model 231BR-HER2 human breast cancer cells were labeled with Feridex SPIO and injected into the carotid artery, in a female nude rat with cytoxan pretreatment. Tumor formation in the breast cancer brain metastasis model MRI (T1 + gadolinium, 3T) and histology (cytokeratin) show multiple breast cancer metastases in rat brain 6 weeks after intracarotid tumor cell infusion. Hypotheses Antibodies targeting CNS vasculature will have antiangiogenic and/or angiolytic activity in established brain tumor vasculature. Antibodies targeting integrin and/or VEGF will block metastatic cell adhesion, brain infiltration, and/or angiogenesis in a hematogenous model of breast cancer brain metastasis. BBB Program Acknowledgements Hatton Institute Robert Albright Nancee Albright Hadassah Medical Center Tali Siegal Edna Shalom Ohio State University John McGregor Sue Bell Cleveland Clinic Foundation Gene Barnett David Peereboom Lily Angelov Glen Stevens University of Minnesota Matthew Hunt Stephen Haines Katie Halbert Patti Bruns University of Oklahoma Mary Kay Gumerlock Carol Young Disclosure Drs. Neuwelt and Muldoon, Oregon Health & Science University (OHSU), Portland Veterans Affairs Medical Center (PVAMC) and the Department of Veterans Affairs have a significant financial interest in Adherex, a company that may have a commercial interest in the results of this research and technology. This potential conflict of interest was reviewed and managed by the OHSU Integrity Program Oversight Council and the PVAMC Conflict of Interest in Research Committee. Dr. Neuwelt has divested his financial interests in Adherex. The studies were entirely funded by Veterans Administration and NIH research grants, with the ferumoxytol USPIO nanoparticles donated by AMAG pharmaceuticals. In light of the results from this study, and subsequent to completion of the manuscript, OHSU has received a sponsored research agreement from AMAG to conduct clinical trials of MRI with ferumoxytol. None of the authors has financial interest in this agent or in its developer AMAG. The following grants helped fund this research: • NIH: – NINDS Grants NS33618, NS34608, NS44687, NS53468 • Veteran’s Administration Merit Review