Anticoagulation: Review of Best Practices
advertisement

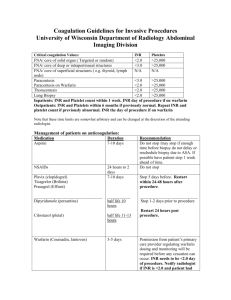
Anticoagulation: review of best practices INTERMACS 9th Annual Meeting May 16, 2015 Salpy V. Pamboukian MD MSPH University of Alabama at Birmingham, Birmingham, AL Outline • • • • • Perioperative Post-operative/long term • • • • INR goals Anti-platelets Monitoring Management Complications • GI bleed • Stroke • • • • Hemorrhagic Ischemic Pump thrombosis Infection Guidelines Durable, continuous flow devices Early practice: 2000’s • Immediate post operative heparin (or alternative) bridging on POD 0-1 or when CT drainage < 50ml/hr • Target PTT 45-50, then stepwise to 55-65 • Warfarin • ASA 81-325mmHg • Other anti-platelets • Dipyridamole 75mg TID • HeartMate II warfarin target 2-3 • HeartWare warfarin target > 1.7, changed to 2-3 in 2011 Pump design changes • HeartWare sintered pump spring 2011 Najjar S et al. JHLT 2014; 33:23-34 Pump design changes • Heart Mate II • pre-clotted graft phased in 2011 • Bend relief recall in Feb 2012 • device labeling revised to provide instructions on how to verify the bend relief is fully engaged with the sealed outflow graft at the time of implant Use of IV heparin post operatively: do we really need it? • HeartMate II BTT LVAD patients -418 patients -3 groups -35 centers • Retrospective analysis of patients enrolled in the clinical trial • Groups were defined based on PTT on days 3,5,7,10,14 • Outcomes: ischemic, hemorrhagic stroke, pump thrombosis, bleeding > 2U • Average duration of support was 293 + 263 days Slaughter et al. JHLT 2010; 29:616-24 Bleeding or Thrombotic Adverse Event Many centers moved away from use of IV heparin bridging post operatively What do the guidelines say…. Feldman D, Pamboukian SV, Teuteberg JJ et al. JHLT 2013 Feb;32(2):157-87 Feldman D, Pamboukian SV, Teuteberg JJ et al. JHLT 2013 Feb;32(2):157-87 Long term anticoagulation: considerations • Balancing bleeding and thromboembolism risk • GI bleeding risk up to ~30% • Stroke risk 8-18% • Co-morbid conditions • Mechanical valves • Atrial fibrillation • Pulmonary embolism What are ideal INR targets? Optimal INR Boyle A et al. JHLT 2009;28: 881–7 Although the initial concerns related to continuous flow LVADs were related to the risk of thrombosis and thromboembolism, it is apparent that thrombotic events are significantly overshadowed by the frequency of hemorrhagic events. The appropriate target INR range for HeartMate II patients should be chosen to minimize the risk of devastating hemorrhagic and ischemic strokes, while reducing the incidence of major bleeding. The original protocol suggested a target INR of 2 to 3. This analysis shows that most patients were actually managed in the INR range of 1.5 to 2.5 and that in this range, the risks of thrombosis and hemorrhage seem balanced. This therefore seems like an appropriate target INR range for most HeartMate II patients. Observed increase in pump thrombosis Kirklin et al. JHLT 2014; 33: 12-22 What do the guidelines say…. Feldman D, Pamboukian SV, Teuteberg JJ et al. JHLT 2013 Feb;32(2):157-87 Feldman D, Pamboukian SV, Teuteberg JJ et al. JHLT 2013 Feb;32(2):157-87 Antiplatelet therapy • ASA 80-325mg daily • Clopidogrel 75mg daily • Dipyridamole 75-100mg three times daily Axial Flow Kreuziger et al. Journal of Thrombosis and Hemostasis, Mar 2015 Axial Flow • TE events were lower in patients with ASA/D vs. ASA • 10% vs. 19%, RR 0.50 (CI 0.36-0.68) • Stroke was lower in ASA/D vs. ASA • 6% vs. 10%, RR 0.58 (CI 0.37-0.93) • VAD thrombosis was lower in ASA/D vs. ASA vs. None • 4% vs. 11% vs. 5% • Three studies of patients treated without ASA reported similar rates of TE, stroke as those with ASA use • Hypothesis generating: different devices, INR goals and patient characteristics Kreuziger et al. Journal of Thrombosis and Hemostasis, Mar 2015 Centrifugal Kreuziger et al. Journal of Thrombosis and Hemostasis, Mar 2015 Newer agents • Newer oral anticoagulant and anti-platelet agents such as rivaroxaban (Xarelto®), dabigatran (Pradaxa®), apixaban (Eliquis®), ticagrelor (Brilinta®) and prasugrel (Effient®) have not been studied in MCS patients and cannot be recommended Monitoring of therapy • Heparin: PTT vs anti Xa • Warfarin • INR • Frequency • MCS team, Anti-coagulation clinic • Home monitoring machine • Alere device had moderate correlation with venous INR values of 0.83 with median difference of 0.391 • Majority recorded higher INR’s with Alere • ASA • TEG • Platelet aggregation 1. Dionizovik-Dimanovski et al. ASAIO April 2015 Feldman D, Pamboukian SV, Teuteberg JJ et al. JHLT 2013 Feb;32(2):157-87 What to do when…. • Subtherapeutic • enoxaparin bridging • Supratherapeutic • Reversal with vitamin K • FFP • Prothrombin complex concentration (PCC) • Factor VII • In a small series of 25 patients, 1/38 reversal attempts resulted in TE event • Patient received high dose Factor VII • Majority received IV vitamin K 10mg and FFP • 5/25 died, 3 from ICH, 2 from sepsis Jennings et al. ASAIO 2014; 60:381-384 Interruption of therapy for procedures • In a meta-analysis of ~ 2100 patients undergoing CIED uninterrupted use of OAC w/ therapeutic INR was associated with reduced risk of bleeding compared with heparin bridging with no difference in TE rates1 Sant’anna et al. Pacing Clin Electrophysiol. 2015 Apr;38(4):417-23. What to do when complications arise…. • GI bleed • Stroke • Ischemic • Hemorrhagic • Pump thrombosis • Infection GI bleeding Guha et al. Methodist Debakey Cardiovasc J. Jan-Mar 2015 Observations • • • • ISHLT MCS guidelines reflect current practice Little supporting evidence Non- randomized data may lead us astray Need standardized protocols that can be prospectively tested • This will be best accomplished if centers collaborate • Given the “high stakes” nature of MCS therapy, ultimately clinicians will need to balance evidence versus individual considerations It’s complicated