mikes quick refernce..
advertisement

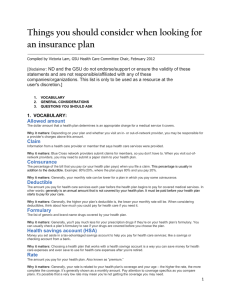
Medical Plan Definitions: Deductible—the amount of covered medical expense that is paid by the insured before plan benefits are paid. Coinsurance—the percent of the covered medical expense that is shared by the worker. Copay—the dollar amount of covered medical expense that is shared by the worker. Stop loss—the maximum amount of employee cost-sharing required each year. AD&D- Accidental Death & Dismember. FSAs- Flexible Spending Accounts FASB- Financial Accounting Standards Board GASB- Government Accounting standards Board TC- Tender Care FFS- Fee For Service RNC- Reasonable and Customary Medical Plans: Basic Plus major Medical, and Comprehensive Plan Basic Plus Major Medical: [ 100% for remainder of calendar year to lifetime max, 80%/20%, Deductible, Basic Plan Benefits.] Basic plan benefits typically include impatient hospital care covered at 100% UCR Deductible is the amt of covered medical exp. Paid by the insured, before Major Medical benefits are payable; typically $100- 200. Plans pay 80%, patient pays 20% up to stop loss Comprehensive Plan: [100% for remainder of calendar year to lifetime max, 80%/20%, Deductible] Deductible aid up front before entitlement to any impatient or outpatient benefits. All plan benefits (both in-patient and out-patient) are covered at the same cost-sharing level. Easier to administer and communicate to employees. Shifts more costs to employees. Cafeteria Plans: * Convert defined benefits plans to defined contribution plans by converting the former into “benefit dollars” which workers use to buy the benefits they want. * Multiple plan options offered to induce workers to select other benefits besides health care * Encourages adverse selection * Shifts inflation risk to workers * High cost plan is unsustainable * FSAs may help for child & LTC Any flexible benefit plan that offers a choice between cash or other taxable benefits and nontaxable benefits is a cafeteria plan. Qualified cafeteria plans protect participants from a tax concept called “constructive receipt.” When a flexible benefits program meets all of the Section 125 features, the dollar value of all program benefits are not considered taxable income to the employee. HMO, PPO, & POS: HMO’S - Three types. Group Model Key feature is the contractual tie between the HMO & medical group Comprehensive benefits provided by medical group. Small copay & deductibles. Limited Choice of doctors & hospitals. Employees must use med. Group except for emergency. Capitation goes to med. Group, hosp. paid negotiated rate. Employer & HMO sign a formal contract. Staff Model Key feature is that doctors are employees of the HMO & paid a salary; hospitals are paid a negotiated rate. Comprehensive benefits are provided by staff doctors. Staff copay & deductible. Limited choice of doctors and hospitals. Employees must use medical group, except in emergencies. Employer and HMO sign a formal contract. Independent Practice Association (IPA) Key feature is dominate role of private practice doctors in the delivery of care. IPA doctors keep fee-for-service patients, practice from own offices and are paid a capitated rate or FFs. More provider choices for employees. Less for quality control for HMO. Similar benefits and cost-sharing arrangements as other models. PPO - Preferred Provider Organization - Offers more choices for consumers and more independence for providers. Key feature is that employee has ability to access non-network specialists, subject to extra deductibles and copays. Wide choice of doctors & hospitals. Employees are motivated to use network providers. Doctors paid on discounted fee-for-service basis; hospitals paid on discount from charges. Employer and PPO sign master contract. POS- Point-of-Service - Melds together features of HMOs and PPOs Health Care industry consolidates From 1990 to 1993, the number of hospitals in the U.S. dropped from 6600 to 6400. From 1990 to 1993 the number of HMOs fell from 566 to 545, while HMO enrollment increased by 32% In April 1996, Aetna bought U.S. Healthcare for $8.9 Billion. IN June 1995, United Healthcare of MN bought Metra Health for $2.3 billion. Columbia/ HCA 9th Largest employer with 347 hospitals and revenues of $20 billion. In 1996 it agreed to buy BCBSO for $300 million and take their $200 million in reserves. Strategy: buy hospitals with good reputations for a good price and use that as a base to build a network of hospital, home care, ambulatory surgery and rehab services to attract managed care plans tan corps. Doctors are invited to invest in Columbia to gain loyalty and referrals for privately insured patients. Maternity wards and emergency rooms are closed to shift costs for those services elsewhere What Happened? The cost of care grew at sometimes two or three times the rate of inflations & became a major drag on total comp and government budgets. Employers adopted two strategies: 1) shift more cost and responsibility to employees, and 2) manage health care costs. Rising costs create climate for employee cost sharing No real wage increases Higher cost sharing Limits on certain benefits & coverage’s More “contract” employees More managed care Unmanaged vs Managed Care Traditional plans have limited agreements with providers. Managed care plans have extensive contracts. Traditional plans do not have gate keepers. Managed care plans do. Traditional plans reimburse doctors on a fee-for-service basis. Managed care plans reimburse doctors by capitations. Managed Care Traditional indemnity plans do not manage care. PPO plans typically manage unit pricing. POS plans typically have PCP direct care with an out-of-network option. HMOs have PCP direct care with no out-of-network option. Advantages (compared to Fee-For-Service) HMOs shift the focus from disease management to disease prevention by: Lowering out-of-pocket costs to see a doctor Standardizing and expanding benefit packages Establishing capitated payments to doctors to discourage unnecessary care and encourage timely necessary care Coordinating care through a them approach Centrally-held medical records Evaluation providers Disadvantages Diminished choice of providers Limited clinical decision-making Limited access to : Primary care doctors High-cost tests Specialists High-cost surgery Necessary in-patient care Necessary Rx drugs New Goals Maximize the potential promises and minimize the potential drawbacks Maintain plan focus on access and quality, not just cost Enhance the doctor/patient relationship Maintain a degree of clinical independence for the attending doctor