Respiratory Motion Management Techniques for Chest and
advertisement

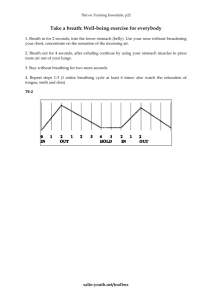
Respiratory Motion Management Techniques for Chest and Abdominal Radiation Therapy Leia Szwedo In partial fulfillment of RT 412 University of Wisconsin – La Crosse, Radiation Therapy Program Background • Issue1: ▫ Respiratory motion caused by patient breathing during radiation therapy treatment can cause displacement of the tumor location. 12 to 16 respiratory cycles every minute SI direction: three to 12 millimeters Anterior-posterior and lateral directions: five mm ▫ Causes difficulty localizing tumor Overdosing normal tissue, under dosing tumor Background cont. • Solution: ▫ Respiratory motion management Techniques: Immobilization of the diaphragm Breathing control Real-time tracking ▫ Consensus shows that in comparison to free breathing radiation treatments, all motion management techniques are beneficial in treating moving tumors.2-4 minimal statistical differences in motion management between the techniques.2-4 Immobilization of the Diaphragm • Utilizes devices to compress the abdomen • Limit the air intake of the patient ▫ Thereby reducing the amount the diaphragm can move and the tumor motion associated with it2 • More precise tumor localization1 • Smaller margins achievable1 Immobilization of the Diaphragm • Examples: ▫ BodyFix2 Dual-vacuum system Mold Plastic sheet Hose Compression Pillow ▫ Abdominal Compression Plate5 Stereotactic body frame Pressure plate Screw Immobilization of the Diaphragm • Advantages2: ▫ ▫ ▫ ▫ ▫ Simplicity Minimal technological devices Easy use Reduce respiratory motion Reusable • Disadvantages2: ▫ Increased setup time ▫ Slight discomfort to some patients ▫ Difficult for patients who experience claustrophobia.2 Breathing Control • Voluntary or machine-regulated breath holds.1 • Causes a cession of breathing during the duration that the beam is on.1 • Commonly used when treating breast, lung, and esophageal cancer.1,3,4 • Techniques: ▫ Deep-inspiration breath-holds (DIBH) ▫ Active breathing control (ABC) Breathing Control • Deep-inspiration breath-holds (DIBH)1,3,6 ▫ Breathing instructions given “Take a deep breath in, and hold it.” ▫ Beam is turned on during breath hold ▫ Patient instructed to breath when beam is turned off • Advantages:1,3,6 ▫ ▫ ▫ ▫ No additional equipments Cost effective Reduces tumor motion Decrease in cardiac treated volumes (V20 from 26.5 to 22.8 percent) and esophageal treated volumes (V50 from 25.5 to 22.6 percent).9 ▫ Increased doses and smaller tumor margins are possible • Disadvantages:1,3,6 ▫ Difficult to determine the breath hold reproducibility ▫ Unrealistic for many elderly or frail patients, or those with pulmonary disease Breathing Control • Active breathing control (ABC) ▫ Mouthpiece placed in the patient’s mouth Hooked up the ABC.7,8 ▫ Continuously monitors lung volume ▫ When the lung volume is at the ideal level, usually 70 to 80 percent of maximum inspiration, the valve on the mouthpiece is closed off Prevents the patient from inhaling or exhaling.6-8 Ensures breath hold reproduciblity.6-8 ▫ The radiation beam is turned on, and once the radiation is finished being delivered, the valve is reopened, allowing the patient to resume breathing.6-8 • Advantages: ▫ Guarantees reproducible breath holds3,6,8 ▫ Reduces tumor motion and cardiac and esophageal treated volumes9 • Disadvantages: ▫ More invasive6,8 ▫ Patient needs to hold their breath for a minimum of 15 seconds6,8 ▫ May require verbal training by the therapist6 Real-Time Tracking • Real time tumor localizations ▫ Techniques to track tumor position5: External respiratory surrogates Implanted radio-opaque fiducial markers Surface imaging • Once the tumor is accurately located, the radiation beam will turn on and begin treating5 • Examples: ▫ Real-time Position Management (RPM) System, AlignRT, and CyberKnife Real-Time Tracking • Real-Time Position Management System ▫ Utilizes an external respiratory surrogate5 A plastic box with infrared reflective markers Placed on top of the patient’s abdominal surface ▫ Infrared cameras detect the reflective markers5,10 ▫ During treatment, the tumor is tracked5 When the respiratory location matches the location predetermined, the beam will turn on. When out of the assigned location, the beam turns off Real Time Tracking • AlignRT11 ▫ Surface imaging ▫ Uses two infrared cameras to triangulate the location of the patient and derive depth information ▫ In order to precisely locate the patient position, an optical pattern is projected onto the patient to identify the corresponding points ▫ An algorithm is computed to use the points to create a surface image of the patient.11 ▫ From the surface image, the therapists can then make shifts to align the image to the original planning image. ▫ Throughout the entire treatment, AlignRT tracts the motion, and only allows the continuation of treatment when the tumor location is within the assigned tolerance location. Real-Time Tracking • CyberKnife5 ▫ Machine moves along with the tumor. ▫ Implements a lightweight 6MV linear accelerator fixed on a robotic arm.5 ▫ A real-time motion system tracks the motion of the tumor, and the robotic arm moves in synchrony to match the movement.5 ▫ Moves in six degrees of freedom to compensate for the true tumor motion.5 ▫ However, the beam output, energy and size are limited.5 Real-Time Tracking • Advantages: ▫ ▫ ▫ ▫ ▫ ▫ Accurate tracking of the tumor.5 Intrafractional movement regulation.1,5 Non-invasive and excludes rigid frames.5 Eliminates patient discomfort Requires no active patient participation.5 Patient receives no additional radiation dose.5 Infrared laser use • Disadvantages ▫ Significantly increased treatment times5 ▫ Tumor motion must be assumed to match the surface motion, unless the system uses internal markers.5 Clinical Implications • Study A2 (Han et al) : ▫ Compared: Free Breathing, BodyFix, Abdominal Compression Plate ▫ Looked at: Tumor motion and patient comfort ▫ Results: Tumor motion: FB = 6.1mm ACP = 4.7mm BodyFix = 5.3mm Patient comfort: 63% of patients preferred ACP Clinical Implications • Study B 3 (STIC 2003 project): ▫ Compared: Free Breathing, Active Breathing Control, Deep-Inspiration Breath-Hold, RPM ▫ Looked at: Target volumes, toxicities, survival, and local recurrence ▫ Results Gating Vs Free Breathing Target volumes: ▫ FB= 360 232 ml ▫ Gating=282 176 ml Acute toxicities: ▫ no notable difference except for pulmonary (48% FB vs. 36% gating) Late Toxicities: ▫ FB=9% ▫ Gating =6% Gating Techniques Survival: no difference Local recurrence: ▫ RPM: 13% ▫ DIBH= 36.7% ▫ ABC= 43.3% Clinical Implications • Study C 4 (Massachusetts General Hospital and Harvard Medical School): ▫ Compared: Deep-Inspiration Breath-Hold and AlignRT ▫ Looked at: Reproducibility ▫ Results: 22% of breath holds were out of 5mm tolerance Combined DIBH and AlignRT produce greatest reproducibility for breath holds. Conclusion • Respiratory motion management is beneficial in the reduction of intrafractional motion • Allows for a decrease in treatment volumes, resulting in a reduction of normal tissue toxicities while giving higher doses to the lesion • Still recommended to use interfractional imaging References 1. Gilin MT. Special procedures. In: Washinton CM, Leaver D, eds. Principles and Practice of Radiation Therapy. 3rd ed. St. Louis, MO: Mosby-Elsevier; 2010: 321-322. 2. Han K, Cheung P, Basran PS. A comparison of two immobilization systems for stereotactic body radiation therapy of lung tumors. Radiotherapy & Oncology. 2010;95(1): 103-108. 10.1016/j.radonc.2010.01.025. 3. Giraud P, Morvan E, Claude L, et al. Respiratory gating techniques for optimization of lung cancer radiotherapy. Journal of Thoracic Oncology. 2011;6(12):2058-2068. doi: 10.1097/JTO.0b013e3182307ec2. 4. Gierga DP, Turcotte JC, Sharp GC, et al. A voluntary breath-hold treatment technique for the left breast with unfavorable cardiac anatomy using surface imaging. Internation Journal of Radiation Oncology Biology Physics. 2012;84(5): 663-668. doi: 10.1016/j.ijrobp.2012.07.2379. 5. Giraud P, Houle A. Respiratory gating for radiotherapy: Main technical aspects and clinical benefits. IRSN Pulmonary. 2013(2013). doi:10.1155/2013/519602. 6. Wong J. Methods to manage respiratory motion in radiation treatment. American Association of Physicists in Medicine Wed site. http://www.aapm.org/meetings/03SS/Presentations/Wong.pdf. Accessed January 14, 2014. 7. Saving the heart of breast cancer patients. Mercy Hospital Web site. http://www.mercy.net/newsroom/2013-03-20/savings-the-heart-of-breastcancer-patients. March 20, 2013. Accessed January 25, 2014. 8. Brock J, McNair HA, Panaskis N, et al. The use of the Active Breathing Coordinator throughout radical non-small-cell lung cancer (NSCLC) radiotherapy. International Journal of Radiation Oncology, Biology, Physics. 2011;81(2): 369-375. doi: 10.1016/j.ijrobp.2010.05.038. 9. Sager O, Beyzadeoglu M, Dincoglan F, et al. Evaluation of active breathing conrol-moderate deep inspiration breath-hold in definite non-small cell lung cancer radiotherapy. Neoplasma. 2012;59(3). doi: 10.4149/neo_2012_043. 10. Real-time position management system respiration synchronized imaging and treatment. Varian Web site. http://varian.com/us/oncology/radiation_oncology/clinic/rpm_respiratory_gating.html. Accessed January 21, 2014. 11. 3D surface reconstruction. VisionRT Web site. http://www.visionrt.com/page-161.html. 2010. Accessed January 14, 2014.