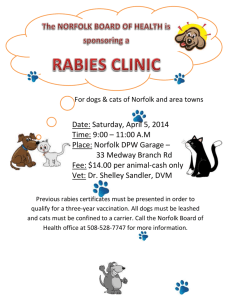
30 April 2014
advertisement

NCoA 05/14 NORFOLK COUNCIL ON AGEING Minutes of the Norfolk Council on Ageing Meeting held at 10.30am on Wednesday 30 April 2014 in the Training Room, Great House Training Centre, Age UK Norfolk, 300 St Faith’s Road, Old Catton, Norwich, Norfolk NR6 7BJ Members Present: Jonathan Bolton (Chair of Age UK Norfolk), John Bracey (Broadland Older People’s Partnership), Judith Brown (West Norfolk Carers), David Button (Age UK Norwich), John Carrick (Norfolk Rural Community Council), Colin Chambers (The Royal British Legion), Stephen Drake (Co-opted Member/Trustee of Age UK Norfolk), Margaret Drury (Age UK North Norfolk), Colin Futter (Norfolk County Council Unison Branch [Retired Members Section]), Joyce Hopwood (Norwich Older People’s Forum), Helen Jones (Vice-Chair of Age UK Norfolk), Pat Kingerlee* (U3A Wymondham Group), Dr Derek Land (Civil Service Pensioners Alliance [Norfolk]), Emily Millington-Smith MBE (President of Age UK Norfolk), Pam Spicer (Norfolk Deaf Association) – Proxy for Aliona Laker, Cllr Sue Whitaker (Norfolk County Council Adult Social Services Committee), Pat Wilson (Norfolk and Norwich Pensioners Association / Norfolk Older People’s Forum) and Dr Peter Woodhouse (Norfolk and Norwich University Hospitals NHS Foundation Trust) In Anne Bunting (The Norfolk and Norwich Association for the Blind), Dr Attendance: James Desborough (UEA), Hilary MacDonald (Chief Executive of Age UK Norfolk), Lin Mathews (Age UK Norfolk), Maggie Parsons (NHS Great Yarmouth and Waveney CCG), Angela Rayner (Age UK Norfolk), Paula Skelton (Age UK Norfolk) – minute taker, Alex Stewart (Norfolk Healthwatch) and Peter Walker Apologies: *Denotes Voting Member Ann Baker* (South Norfolk Older People’s Forum), Bett Barrett* (Coopted Member), Gaye Clarke* (Department for Work and Pensions), Dr Graeme Duncan* (Co-opted Member), Aileen Francis (Age UK Norfolk), Susan Fraser* (Co-opted Member/Trustee of Age UK Norfolk), Margaret Hardingham* (Vice-President of Age UK Norfolk), Polly Hauxwell-Baldwin* (Co-opted Member/Trustee of Age UK Norfolk), Aliona Laker* (Norfolk Deaf Association), Ann Leigh* (Coopted Member/Trustee of Age UK Norfolk), Barbara Lock* (Age Concern Swaffham and District), Rachel McLean* (Co-opted Member), Jacqueline Middleton* (Age UK Norwich), Catherine Morgan* (The Queen Elizabeth Hospital King’s Lynn NHS Foundation Age UK Norfolk is the operating name of Age Concern Norfolk, a Charitable Company limited by guarantee Registered in England No 03783205. Registered Charity No 1077097. The Registered Office is 300 St Faiths Road, Old Catton, Norwich, Norfolk NR6 7BJ Trust), Annie Moseley (Age UK Norfolk), Chris Mowle* (Co-opted Member/Trustee of Age UK Norfolk), John Perry Warnes, Jack Sadler* (Norfolk Association of Local Councils), Dr Charlotte Salter* (Norwich Medical School, UEA), Vernon Simmons* (Breckland Older People’s Forum), Paul Slyfield* (Treasurer of Age UK Norfolk), Richard Watson* (Co-opted Member/Trustee of Age UK Norfolk), Carole Williams* (Co-opted Member) and Jean Wilson* (Norfolk Federation of Women’s Institutes) The Chair welcomed everyone to the meeting and gave information on a number of housekeeping items. Action 1. Minutes of the Norfolk Council on Ageing Meeting held on Wednesday 22 January 2014 (NCoA 05/14) The minutes of the Norfolk Council on Ageing (NCoA) meeting held on 22 January 2014 had been circulated prior to the meeting and were agreed as a correct record and signed by the Chair. 2. Matters arising 2.1 Clause 48 The Chair reported that following a campaign led by Age UK to overturn Clause 48 of the Care Bill, there had been a successful outcome. The result meant that the loophole (Clause 48) would be closed for people who received care in their own home where this was arranged or paid for by the Local Authority. Up to now, this group of people had no protection under Human Rights Law. The Chair thanked everyone who had signed Age UK’s petition and the news was welcomed by members. 2.2 Adult Social Services The Chair invited Cllr Whitaker to update on the Norfolk County Council (NCC) budget. Cllr Whitaker reported that 60% of people who received support from the Adult Social Services Department (ASSD) at NCC received Personal Budgets. People in residential care usually received only a very small Personal Budget. It was normally people who had intensive home care needs and younger people who received more substantial Personal Budgets. Cllr Whitaker explained that some Personal Budgets included a care element and a “social” or “wellbeing” (discretionary) element. The care element would be unaffected by the re-assessments of Personal Budgets and it would be the “wellbeing” element that might be affected. Page 2 of 10 Cllr Whitaker reported that the Council was required to save £6,000,000 over two financial years with the bulk of changes to Personal Budgets taking place in the next financial year. In the current financial year, people who receive a Personal Budget will not see a change. Everyone who receives a Personal Budge will have a face-to-face assessment, with the exception of those in residential care who have a very small Personal Budget. Following the assessment, any changes would be made in the following financial year. Cllr Whitaker gave an example whereby an individual assessed in April would have the changes implemented the following April. To help meet the challenge of undertaking the assessments, an extra £1,000,000 was being used to resource the additional staffing required. Ms Brown commented that the number of face-to-face assessments would be very high and Cllr Whitaker said that the Council recognised this, hence recruiting additional staff to undertake the work. Ms Drury asked about the possible effect on day centres and Cllr Whitaker referred to Independence Matters, a joint staff and councilowned community interest company, which provided a range of care and support services to people across Norfolk. Ms Drury said price was often a factor in people choosing not to attend a day centre. Cllr Whitaker said that it was possible that the environment put some people off and investment could help with this. Mr Wells asked about the likely savings and Cllr Whitaker said that it was likely to be £11,000,000 over three years. This was out of a total of £205,000,000 budget on care for people in Norfolk. The Chair thanked Cllr Whitaker for her update. 2.3 Acle Day Support Club The Chief Executive reported that work was continuing to assess the needs around transport to Age UK Norfolk’s Acle Day Support Club. 3. Maggie Parsons, Cancer and End of Life Programme Manager for NHS Great Yarmouth and Waveney Clinical Commissioning Group (CCG): Update on the work of the Norfolk and Suffolk Palliative Care Academy The Chair introduced Ms Parsons and she thanked him for the invitation to speak at today’s meeting, which followed on from the presentation given by Sue Spooner at the April 2013 meeting of the NCoA. Ms Parsons explained that the Norfolk and Suffolk Palliative Care Academy had been established to improve palliative and end of life care through raised awareness and education. Ms Parsons explained Page 3 of 10 the structure of the Academy. Ms Parsons explained that palliative care was not currently commissioned but is delivered by hospitals because there is a need. The Academy’s activities included: Raise awareness: o “Be ready for it” campaign: www.bereadyforit.org.uk. o Sponsorship of the Norfolk Care Award for effective coordination of palliative care. Enhance the quality of education and training: o Education providers group. o Learning location for palliative care www.learncare.org. Enhance and align education and care commissioning: o Collaborative commissioners group. Promote involvement in research: o Improve the infrastructure for palliative care research. Ms Parsons explained that the “Be ready for it” campaign aimed to address the taboo surrounding discussion by people about death and dying, and their wishes surrounding their own death. This was also a challenge for those staff who worked in palliative care, dealing with patients at the end of their life. The campaign encouraged people who were at the end of their life to talk about their wishes when they died, to help their relatives cope and know what they want at a difficult time. Ms Parsons said a public awareness campaign might help with this. Ms Parsons commented that it was important not to be defensive about the Liverpool Care Pathway (LCP) and that lessons should be learned by medical staff around patients’ fears and concerns. Ms Parsons said that gaps in palliative care included Occupational Therapists (OTs) who had very little training around palliative care and training for medical staff, which included one week of training during their five year’s training. Ms Parsons said that implementation of key elements of the Academy’s work included investment plans for transformation of the workforce, care of older people, people affected by long-term conditions and dementia and more support for informal carers. Preparing for possible illness and death included: Making a will. Page 4 of 10 Putting in place guardianship wishes regarding the care of one’s children. Setting up a Lasting Power of Attorney (LPA). Setting up an advance directive. Talking about and informing relatives of wishes around treatment in the event of serious illness. Writing a “bucket list”. Ensuring that close relatives were aware of one’s wishes and where key documents such as an advance directive were held. Ms Parsons reported that future plans included participating in the Dying Matters Week taking place from 12 to 18 May 2014 and a major event at The Forum in Norwich on 14 May. Ways of working with Age UK Norfolk included linking in with the advocacy service and encouraging people to think ahead about their wishes. This could be done by mentioning the Be Ready for It campaign during talks. Ms Parsons said volunteers were required for their talks and invited members to consider volunteering. In response to a query, Ms Parsons confirmed that work was taking place in the West of the County where her contact was Hanna Lene Schierff, Commissioning Manager - West Norfolk, Integrated Community Health and Social Care. Ms Parsons said that the issue of assisted suicides was a very difficult one and the Academy hoped to create an environment where people did not have to think about suicide as an issue, because they were being adequately supported. Dr Land asked about support required to set up an LPA or advance directive which could be costly where solicitor’s needed to be involved. Dr Land said it would be helpful for solicitors to have resources available which would allow them to signpost people to organisations which could help. It was noted that if mental capacity was an issue, then it might be preferable to instruct a solicitor to ensure that the legality of any documents were not compromised. The Chair noted that a family solicitor was also likely to know about family circumstances which was helpful when dealing with sensitive issues. The Chief Executive noted that Age UK Norfolk provided a service for older people wanting help to complete paperwork for LPAs. The Chair thanked Ms Parsons for her presentation and wished the Academy well in its work. The Chief Executive also thanked Ms Spooner and Ms Parsons for the work they were undertaking on palliative care and end of life issues. 4. Board of Trustees Report to the NCoA (NCoA 06/14) 4.1 A report from the Board of Trustees prepared by the Chief Executive had been circulated prior to the meeting. Page 5 of 10 The Chair reported the sad news that Carole Williams’s, NCoA member, husband, David, had recently died. Mrs Williams hoped to return to her volunteering role on the Information and Advice Line in due course. Mr Button asked if Mrs Williams would be continuing with the work she had undertaken on buses and Mrs Hopwood said that she had discussed this with Mrs Williams who had confirmed that she no longer wished to continue this. Mrs Pat Wilson had confirmed she was willing to undertake this role and this was welcomed. Mrs Wilson said she would report on her work to the NCoA. 4.2 Ten-Minute Update – Results from the CAREMED Study (Multi-professional medication reviews in care homes for older people): Dr James Desborough, Lecturer in Pharmacy Practice, School of Pharmacy, University of East Anglia The Chair introduced Dr Desborough and he thanked the Chair for the invitation to the meeting to update on the work he had previously reported on at the April 2011 NCoA meeting, when the project was being established. Dr Desborough acknowledged the research teams, GPs and care home staff involved in the project. Dr Desborough reminded members about the background to the project: Management of medicines in care homes. Pharmacist led medication reviews show promise. Novel approach in Cambridgeshire. The aim of the project was to determine the clinical and cost effectiveness of CAREMED service. The objectives were to: Determine impact of CAREMED on: Number of falls. Potentially inappropriate prescribing. Medication costs. Primary care time (NHS resource use). Emergency hospital admissions. Mortality. Dr Desborough explained how the project had been undertaken and who had been involved and said his project had focussed on falls reduction and inappropriate prescribing. The need to encourage MFE consultants to intervene and avoid hospital admissions was highlighted. Dr Desborough reported that the CAREMED model currently costs £100 per patient but there were ways to reduce costs such as maintaining e-records and holding virtual meetings. GPs attending care homes was expensive. Page 6 of 10 In conclusion Dr Desborough reported that the research showed no statistical difference in falls but the quality of prescribing had improved. There was a discussion around a number of items: 5. It was agreed that the slides would be made available to NCoA members on Age UK Norfolk’s website. GP involvement in the project. Dr Desborough said that it was better for the patient where one team was responsible for one person. Over-medication issues outside care homes. Pharmacy teams visiting people in their own homes. Repeat prescriptions and annual reviews. Verbal Report from the Norfolk Older People’s Strategic Partnership Board (NCoA Representatives: Carole Williams, David Button and Dr Derek Land) Mrs Hopwood, Chair of the Norfolk Older People’s Strategic Partnership (NOPSP) Board, reported that the last NOPSP Board meeting had focussed on end of life care for people with dementia. The NOPSP’s paper on the dementia strategy had been adopted by the Norfolk Health and Wellbeing Board on 08 January 2014 and Mrs Hopwood agreed to send a copy to Ms Skelton for circulation to NCoA PS members. 6. Joint Health, Social Care and Voluntary Sector Strategic Forum and the Health and Wellbeing Board – Joyce Hopwood, NCoA Representative Mrs Hopwood reported that there was concern amongst the representatives sitting on the Joint Health, Social Care and Voluntary Sector Strategic Forum about the level of activity of the Forum. Mrs Hopwood reported that an additional meeting of the Health and Wellbeing Board took place on 01 April to discuss the Better Care paper before submitting it to NHS England. The paper had been drawn up by the five CCGs in Norfolk. Mrs Hopwood said that the Health and Wellbeing Board was driving forward work around health and social care integration. 7. Presentation: Alex Stewart, Chief Executive of Norfolk Healthwatch: Norfolk Healthwatch’s Priorities for 2014-2015 The Chair introduced Mr Stewart and he thanked the Chair for the invitation to talk about the work of Norfolk Healthwatch. Mr Stewart explained that Healthwatch had been established on 01 April 2013 as a result of the Care Bill (now Care Act), to help the Page 7 of 10 public, patients and users of social care influence the way that services are planned and delivered in Norfolk. Their partners included NHS England, NCC and the CCGs. Mr Stewart said that to help with a smooth transition from LINks (Local Involvement Networks) to Healthwatch, a shadow Healthwatch Board had been meeting for some time before the official launch on 01 April. Mr Stewart reported that Healthwatch covered all areas of care from pre-natal to death. The Chair of Healthwatch is William Armstrong and the office is based in Hethersett. Mr Stewart’s background was in health and social care. Mr Stewart reported that Healthwatch’s priorities for 2014-2015 were: Access to services by vulnerable groups. Avoiding unnecessary hospital admissions. Child and Adolescent Mental Health Services. Children and Young People’s engagement. Community Nursing Review. Dementia. East of England Ambulance Trust (including non-urgent patient transport). Handling of Complaints. Integration Agenda. Maternity Services. Mental Health Provision in Norfolk. Personal budgets. Residential provision for adults with learning difficulties. Unpaid family carers. Work had focussed on encouraging integrated care and specific research had been undertaken on: How individuals interacted with homeless people and people with drug and alcohol problems in Waveney. Bed availability for people under the age of 18 who have mental health illnesses. Mr Stewart responded to a number of items: Versatility of Personal Budgets. Healthwatch had no regulatory powers although it works closely with CQC (Care Quality Commission). Challenges around transport in such a rural county as Norfolk. Respite care was not included in the priorities. The number of priorities was raised as a potential issue and a question was raised as to whether this was realistic in terms of achieving them. Mr Stewart said that Healthwatch had worked with a number of organisations to formulate the priorities and surveyed Norfolk residents via the “Your Norfolk” magazine about their Page 8 of 10 perception of health and social care. A quality control panel checked each project and priority. Healthwatch was also working with a number of partners to undertake the work, as well as benefiting from 57 volunteers who were experts in their respective specialisms. Mr Stewart commented that he would be happy to attend another NCoA meeting next year to update members on the priorities and work of Healthwatch. The Chair thanked Mr Stewart and wished Norfolk Healthwatch well with its work. 8. Any Other Business 8.1 Bills Mrs Pat Wilson reported that she had noticed on a telephone bill she had recently received that she was being charged an additional £1.50 because she received a hard copy of her bill (rather than an electronic bill). It was felt that most older people would prefer to continue to receive a hard copy of their bills and there was a push by companies to force people into receiving electronic copies by making them pay for paper copies. It was agreed that the Chief Executive would contact Age UK to raise HM the issue. 9. Date of Next NCoA Meeting: At 10.30am on Wednesday 29 October 2014 (subject to confirmation at the Annual General Meeting) in the Training Room, Great House Training Centre, Age UK Norfolk, 300 St Faith’s Road, Old Catton, Norwich, Norfolk NR6 7BJ. There being no further business, the Chair closed the meeting at 12.40pm. Signed ……………………………… Position …………………………….. Page 9 of 10 Date …………………………………. Circulation: NCoA Members NCoA Non-Members Age UK Norfolk Website Page 10 of 10