path 158 to 167 [10-4
advertisement

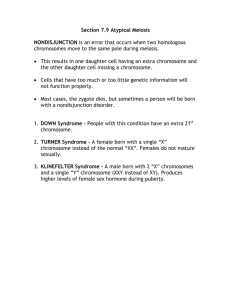
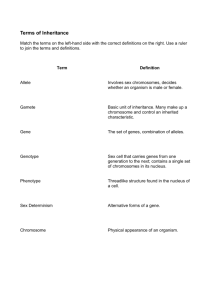
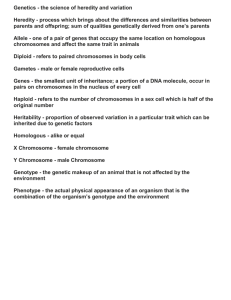
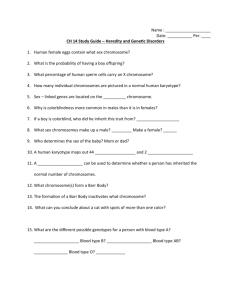
path 158 to 167 Chromosomal Disorders Karyotyping – usual procedure is to arrest dividing cells in metaphase with mitotic spindle inhibitors and stain chromosomes – in metaphase spread, the chromosomes take the form of two chromatids connected at the centromere – chromosomes are then arranged longest to shortest with the sex chromosomes at the end o G banding (Giemsa stain) can be used to stain cells so they can be sorted by their distinctive pattern of alternating light and dark bands o G banding resolution is better obtained when cells are arrested in prophase Karyotype nomenclature o 46,XY is format for normal karyotype o 47,XX,+21 is format for trisomy (in this case, Down syndrome) o Within the karyotype, gene location can be described by gene number, then short or long arm, then region, then band, then sub-band – example Xp21.2 means the chromosomal segment located on the short arm of the X chromosome, in region 2, in band 1, in sub-band 2 Euploid – any exact multiple of the haploid number of chromosomes Usual causes for aneuploidy are nondisjunction and anaphase lag o In anaphase lag, one homologous chromosome in meiosis or one chromatid in mitosis lags behind and is left out of cell nucleus, resulting in one normal cell and one monosomy Occasionally, mitotic errors in early development give rise to two or more populations of cells with different chromosomal complement in the same individual (mosaicism) – can occur during cleavage of fertilized ovum or in somatic cells o Phenotypic expression of mosaicism depends on number and distribution of odd cells o Phenotype is then listed 46,XY/47,XY,+21 in the case of mosaic Down syndrome o Mosaicism usually occurs from Turner’s/XXX syndrome or other sex-linked syndromes – autosomal mosaicism is very rare Fluorescence in situ hybridization (FISH) – can be used to detect changes as small as kilobases in translocation problems Deletion notation 46,XY,del(16)(p11.2p13.1) would be a normal boy with deletion between position 11.2 and 13.1 on the short arm of chromosome 16 o Ring chromosome – produced when break occurs at both ends of a chromosome with fusion of the damaged ends – expressed as 46,XY,r(14) if a normal boy with a ring chromosome 14 Do not behave normally in meiosis or mitosis and usually result in serious consequences Inversion involving only one arm of the chromosome is paracentric – if breaks are on opposite sides of the centromere, it is called pericentric – often fully compatible with normal development Isochromosome formation results when one arm of chromosome is lost and remaining arm is duplicated, resulting in a chromosome consisting of only two short arms or two longs arms o Most common isochromosome present in live births involves long arm of X chromosome and is designated i(X)(q10) – Xq isochrome associated with monosomy for genes on short arm of X and trisomy for genes on long arm of X Translocation between long arm of chromosome 2 and short arm of chromosome 5 written 46,XX,t(2;5)(q31;p14) – because there is no actual loss of genetic material, individual is likely to be phenotypically normal (balanced translocation) but has increased risk of producing abnormal gametes o Robertsonian translocation – occurs between 2 acrocentric chromosomes – breaks occur close to centromeres of each chromosome and transfer causes one very large chromosome and one very small one (long arm attaches to other side of other chromosome’s long arm and short arm attaches to other side of other chromosome’s short arm) – usually small product is lost, but because this is only highly redundant genes, the phenotype is still compatible with life Trisomies other than 21 have been observed (8, 9, 13, 18, and 22), but only trisomy 18 and trisomy 13 are common enough to know much about o Trisomy 18 – Edwards syndrome o Trisomy 13 – Patau syndrome o Both are caused by nondisjunction, and mother’s age plays a part in this o Both rarely survive beyond the first year of life with most living only weeks to months Chromosome 22q11.2 Deletion Syndrome – spectrum of disorders that result from small deletion of band q11.2 o Often missed because of variable clinical features o Can have congenital heart defects, abnormalities of palate, facial dysmorphism, developmental delay, and variable degree of T-cell immunodeficiency and hypocalcemia o Originally classified as two separate syndromes – DiGeorge syndrome and velocardiofacial syndrome DiGeorge syndrome was patients with thymic hypoplasia with resultant T-cell immunodeficiency, parathyroid hyperplasia giving rise to hypocalcemia, a variety of cardiac malformations affecting outflow tract, and mild facial anomalies Velocardiofacial syndrome was patients with prominent nose, retrognathia, cleft palate, cardiovascular anomalies, and learning disabilities o Overlap of symptoms caused interest in similar cytogenetic abnormalities, which lead to karyotyping o Individuals at high risk for psychotic illnesses such as schizophrenia and bipolar disorders o 30%-35% of children with this syndrome develop ADHD o Can only be diagnosed by FISH o 30% of people with conotruncal cardiac defects but no other features of this syndrome also have this deletion o Suspected reason why deletion is the way it is is because of a TBX1 gene on the deletion Cytogenetic Disorders Involving Sex Chromosomes Far more common than autosomal aberrations Much better tolerated than imbalances of autosomes o Because of lyonization or inactivation of all but one X chromosome and modest amount of genetic material carried by Y chromosome Lyon hypothesis states o Only one of X chromosomes is genetically active o Other X of either maternal or paternal origin undergoes heteropyknosis and is rendered inactive o Inactivation of either maternal or paternal X occurs at random among all the cells of the blastocyst on or about day 16 of embryonic life o Inactivation of the same X chromosome persists in all the cells derived from each precursor cell Because of this, normal females are mosaics of populations of paternal and maternal X chromosomes o XIST – gene that causes inactivation of one X chromosome – this allele is switched off in the active X – product is noncoding RNA that is retained in nucleus where it coats the X that is to be transcribed from and initiates gene-silencing process by chromatin modification and DNA methylation o Many genes escape X inactivation o At least some of the genes that are expressed from both X chromosomes important for normal growth and development – proof is that Turner syndrome (45,X) have severe somatic and gonadal abnormalities o Barr body X is selectively reactivated in oogonia before first meiotic division (both X’s are necessary for normal oogenesis) SRY – sex-determining region Y gene – dictates testicular development and is on distal short arm of Y chromosome o Many gene families in MSY region (male-specific Y) – all of these believe to be testes-specific genes involved in spermatogenesis The greater the number of X chromosomes, the greater the likelihood of mental retardation Klinefelter syndrome – XXY – one of the most common causes of hypogonadism in male – rarely diagnosed before puberty o Many have distinctive body habitus with increase in length between soles and pubic bone, creating the appearance of an elongated body o Eunuchoid body habitus with abnormally long legs, small atrophic testes and a small penis o Lack secondary male characteristics (deep voice, beard, male distribution of pubic hair) o Gynecomastia may be present o Mean IQ is lower than normal, but mental retardation is uncommon o Increased incidence of type 2 diabetes and metabolic syndrome o Mitral valve prolapse seen in about 50% of adults with Klinefelter o Plasma gonadotropin concentrations, particularly FSH, are consistently elevated and testosterone levels reduced o Mean plasma estradiol levels elevated o Ratio of estrogens and testosterone determines degree of feminization o In some patients, testicular tubules are totally atrophied and replaced by pink, hyaline, collagenous ghosts In others, apparently normal tubules are interspersed with atrophic tubules In some, tubules are primitive and appear embryonic, consisting of cords of cells that never developed a lumen or progressed to mature spermatogenesis o Leydig cells appear prominent as a result of atrophy and crowding of tubules and elevation of gonadotropin concentrations o Higher risk of developing breast cancer, extragonadal germ cell tumors, and autoimmune diseases such as systemic lupus erythematosus o Maternal and paternal nondisjunction at first meiotic division roughly equally involved o No phenotypic difference between those that get the extra X from mother or father o 15% of patients have variety of mosaic patterns, most of them being 46,XY/47,XXY o Some 47,XXY/48XXXY have been found o Gene encoding androgen receptor, through which testosterone mediates its effects, maps on X chromosome Androgen receptor gene contains highly polymorphic CAG repeats Functional response to androgens is dictated in part by number of CAG repeats With shorter CAG repeats, effect of androgens is more pronounced In Klinefelter syndrome, X with shortest CAG repeat is preferentially inactivated, leaving X with longer CAG repeat active, resulting in hypogonadism Turner syndrome – 45,X – characterized by hypogonadism in phenotypic females o Most common sex chromosome abnormality in females o 57% are 45,X, 14% have structural abnormalities of X chromosomes, and 29% are mosaics Structural abnormalities may include Isochromosome of long arm 46,X,i(X)(q10) resulting in loss of short arm Deletion of portions of both long and short arms resulting in formation of ring chromosome 46,X,r(X) Deletion of portions of short or long arm, 46X,del(Xq) or 46X,del(Xp) o Mosaic patients can have 45,X/46,XX 45,X/46,XY 45,X/47,XXX 45,X/46,X,i(X)(q10) o Because 99% of 45,X conceptuses are nonviable, many believe that there are no truly nonmosaic Turner syndrome patients o Lots of karyotypes of Turner are responsible for significant variations in phenotype – the higher number of cells with 45,X, the more severe the phenotypic changes o Those with 45,X/46,XY are at risk for developing gonadal tumor o Those most severely affected present during infancy with edema of dorsum of hand and foot due to lymph stasis and sometimes swelling of the nape of the neck Neck webbing due to markedly distended lymphatic channels, producing so-called cystic hygroma Swelling subsides as infant develops, but neck webbing stays o Congenital heart disease affects 25%-50% of patients Left-sided cardiovascular abnormalities, particularly preductal coarctation of aorta and bicuspid aortic valve, are most frequently seen Cardiovascular abnormalities most important cause of increased mortality in Turner children o At puberty, there is failure to develop normal secondary sex characteristics o Genitalia remain infantile, breast development is inadequate, and there is little pubic hair o Mental status is usually normal, but subtle defects in nonverbal, visual-spatial information processing have been noted o Rarely exceed 150 cm in height o Single most important cause of primary amenorrhea o About 50% of patients develop autoantibodies that react with thyroid gland, and up to half of these develop clinically manifest hypothyroidism o Minority of patients have glucose intolerance, obesity, and insulin resistance Of note because therapy with GH (often used in these cases) worsens insulin resistance o Absence of second X chromosome leads to accelerated loss of oocytes, so oocytes completely gone by age 2, and ovaries are reduced to atrophic fibrous strands, devoid of ova and follicles (streak ovaries) o SHOX (short stature homeobox) involved in Turner syndrome – on gene at Xp22.33 – one of several genes that remain active in both X chromosomes and has active homologue on short arm of Y chromosome – haploinsufficiency of this gives rise to short stature and excess copies of this gene give rise to tall stature Expressed during fetal life in growth plates of several long bones, including radius, ulna, tibia, and fibula Expressed in 1st and 2nd pharyngeal arches Hermaphroditism and pseudohermaphroditism o Genetic sex – presence or absence of Y chromosome o Gonadal sex – based on histologic characteristics of gonads o Ductal sex – depends on presence of derivatives of müllerian or wolffian ducts o Phenotypic (genital) sex – based on appearance of external genitalia o True hermaphrodite – presence of both ovarian and testicular tissue o Pseudohermaphrodite – disagreement between phenotypic and gonadal sex (female pseudohermaphrodite has ovaries but male external genitalia, and male pseudohermaphrodite has testicular tissue but female-type genitalia) o True hermaphroditism – extremely rare – can have a testis on one side and ovary on the other – may be combined ovarian and testicular tissue, referred to as ovotestes Karyotype is 46,XX in 50% of patients and rest are mosaics with 46,XX/46,XY Rarely is constitution 46,XY Those with 46,XX may possess SRY gene somewhere else in chromosomal material o Female pseudohermaphroditism – always XX, and development of ovaries and internal genitalia is normal – only external genitalia are ambiguous or virilized Basis is excessive and inappropriate exposure to androgenic steroids during early part of gestation, most commonly derived from fetal adrenal affected by congenital adrenal hyperplasia, transmitted as autosomal recessive trait Biosynthetic defects in pathway of cortisol synthesis present in these patients, which lead secondarily to excessive synthesis of androgenic steroids by fetal adrenal cortex o Male pseudohermaphroditism – most complex of all disorders of sexual differentiation – possess Y chromosome, and thus gonads exclusively testes, but genital ducts or external genitalia are incompletely differentiated along male phenotype External genitalia are either ambiguous or completely female Extremely heterogeneous with multiplicity of causes Common to all is defective virilization of male embryo, which usually results from genetically determined defects in androgen synthesis or action or both Most common form (complete androgen insensitivity syndrome or testicular feminization) results from mutations in gene encoding androgen receptor, located at Xq12 (X-linked recessive)