Shedding Light On Restless Legs Syndrome Via The Human
advertisement

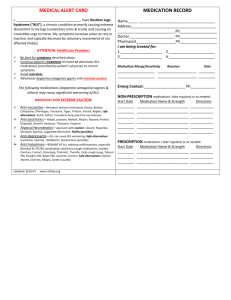
Shedding light on Human Genome Shedding light on Restless Legs Syndrome Restless via Legs Syndrome the Human Genome:via the Pharmacogenomic Implications David B. Rye Professor of Neurology David Rye, MD, PhD Director, Emory University Program in Sleepof Neurology Professor Atlanta, GA Director, Emory Healthcare Program in Sleep RLS Affects Tens of Millions in the United States alone RLS is more prevalent than originally believed1 – RLS affects approximately 10% of the US adult population, yet often goes undiagnosed2 – Approximately 12 million Americans suffer from moderate to severe ‘primary’ RLS2,3 1. Hening W. Clin Neurophysiol. 2004;115:1965-1974. 2. Hening W, et al. Sleep Med. 2004;5:237-246. 3. NINDS, NIH; 2001. NIH Publication No. 01-4847. Burden of RLS is Significant • Depressed mood (OR = 2.6) • Stroke & Cardiovascular disease (OR= 2.4-2.5) • Hypertension (OR = 1.5; *PLMs > 30/hr OR = 2.3) Ulfberg J, Nystrom B, Carter N, Edling C. Prevalence of restless legs syndrome among men aged 18 to 64 years: an association with somatic disease and neuropsychiatric symptoms. Mov Disord 2001;16:1159-1163. Winkelman J, Finn L, Young T. Prevalence and correlates of restless legs syndrome in the Wisconsin sleep cohort. Sleep 2005;28(Abst Suppl):A263-264. – Sleep Medicine 2006-May 30th (epub ahead of print) *Personal observations; Winkelman et al. (2008) Neurology 70:35-42 RLS PLM RLS remains a clinical diagnosis: IRLSSG/NIH Diagnostic Criteria for RLS • Urge to move legs, usually accompanied by uncomfortable leg sensations • Onset or worsening of symptoms at rest or inactivity, such as when lying or sitting • Relief with movement—partial or total relief from discomfort by walking or stretching • Worsening of symptoms in the evening and at night Allen RP, et al, for the International Restless Legs Syndrome Study Group. Sleep Med. 2003;4:101-119. Periodic leg movements in sleep (PLMs) in RLS appear to exhibit heritability (at least as much as, if not more than, sensory symptoms)! Iron is central to RLS symptomatology • RLS symptoms occur in > 40% of subjects with iron deficiency Akyol et al., Clin Neurol Neurosurg. 2003 Dec;106: 23-7. • In vivo and in vitro iron depletion in dopamine rich brain regions of RLS patients Allen et al., Neurology. 2001 Jan 56: 263-5. Connor et al., Neurology. 2003 Aug 61: 304-9. • Iron deficiency adversely affects dopamine signaling Allen et al, Sleep Med. 2004 Jul 5:385-91 • Oral and intravenous iron can ameliorate RLS symptoms. Earley, Heckler and Allen Sleep Med. 2004 May 5: 231-5. Iron trafficking appears to be awry in RLS/PLMs – A “leaky” bucket IRON RLS Patient Earley, Heckler and Allen, Sleep Medicine (2005) 6: 301 Treatment Options • Oral or intravenous iron repletion when iron deficiency confirmed (9-50% of cases) • Dopaminergics – 1st line treatment as per American Sleep Disorders Assoc. Standards of Practice Committee and the Medical Advisory Board of the RLS Foundation • Pramipexole (0.125-0.75mg) – Ropinirole (0.254.0mg) 90-120 minutes before typical symptom onset– FDA approved for idiopathic, moderate-severe RLS Off-label: • Opioids – • Anticonvulsants – gabapentin RLS Aggravators • Alcohol (tanins; GABAAReceptor modulation) • SNRIs > SSRIs >> SDRIs • Antidopaminergic medications – e.g., metaclopramide; prochlorperazine (compazine) • Anti-histamines (e.g., diphenhydramine) • Over-the-counter sleep aids and cold remedies (ephedrines) A genetic-linkage analysis of RLS in Iceland Funded in part by the Restless Legs Syndrome Foundation in collaboration with deCODE Genetics, Reykjavik, Iceland Homogeneity Excellent genealogic records Excellent record keeping in health care Highest literacy rate in the world Participation in clinical studies is high (80-85%) 4 recently identified gene variants account for at least 80% of the population attritubable risk for RLS To everyone’s surprise/dismay: • None of the implicated genes directly or indirectly affect iron or dopamine. • The implicated regions are intronic or intergenic and suggest regulatory roles. • The functions are in many cases not well known. SNPs associating to RLS are intimately related to the disease biology: • Multiple SNPs in at least the BTBD9 and Meis1 genes are related in a dose dependent fashion to PLMs – bearing ZERO relationship to RLS rating scales • Multiple SNPs in the BTBD9 gene are inversely related in a dose dependent fashion to low iron stores • At-risk SNP frequencies in disparate ethnic groups mirrors the large range of ethnic differences in RLS prevalence RLS at-risk variants are COMMON and considerably impact population risk for RLS Allele Frequency Gene OR BTBD9 1.4-2.3 0.73-0.82 (0.656) 0.47-0.61 7x10-7 – 1x10-18 MEIS1 ~0.20 1x10-3 – 8x10-16 1x10-2 – 6x10-5 1.7-2.1 0.18-0.21 (0.114) PAR MAP2K5 1.3-1.5 0.74-0.78 (0.692) ~0.34 PTPRD 0.17-0.20 (0.13) <0.10 1.3-1.4 (X.XX) = allele frequency in Icelandic population controls p value Homozygous for BTBD9 Younger or Asian Uremia Pondering the Genetics Landscape: Will genotypes correlate with specific phenotypes? Can genetic testing inform diagnosis and treatment decisions? What are the downstream molecular networks that effect disease expression? Pharmacogenics for RLS – targets? • Treatment stratification Dopaminergics vs. opioids vs. iron vs. ? • Complication stratification Dopaminergic augmentation Aggravators (e.g., antihistamines; metaclopramide) • Predictive Health End-Stage Renal Disease Pregnancy RLS pharmacogenomics - challenges • RLS genes Despite high ORs, commonality of at-risk SNPs necessitates large (600-1000) sample sizes Choice of (endo) phenotype Latent or incipient disease • Non-RLS genes Dissecting disease biology Acknowledgements Emory Program in Sleep Dr. Donald Bliwise Dr. Michael Decker Dr. Alex Iranzo Dr. Jeffrey Durmer Dr. Lynn-Marie Trotti Dr. Lisa Billars Dr. Reddiah Mumanenni Dr. Glenda Keating Dr. Amanda Freeman Dr. Tom Genetta J Max Beck Gillian Hue Daniel Miller Kaniyika Freeman Emory Dept. of Cell Biology deCODE Genetics Dr. S. Sanyal Dr. Hreinn Stefansson Dr. KristleifurKristjansson Emory Dept. of Genetics Dr. Andrew Hicks Dr. Steve Warren Dr. Larus Gudmundsson Dr. Mark Bouzyk Ingibjorg Eiriksdottir, RN Dr. Jeffrey Gulcher Dr. Kari Stefansson Emory Dept. of Neurology Dr. Allan Levey Landspitali Dr. Salina Waddy Ami Rosen Dr. Thordur Sigmundsson CRIN Staff Dr. Albert Pal Sigdursson Emory School of Public Health Dr. Harland Austin Funding RLS Foundation Arthur L. Williams Jr. Foundation Woodruff Health Sciences