Psychological Disorders Affecting Women
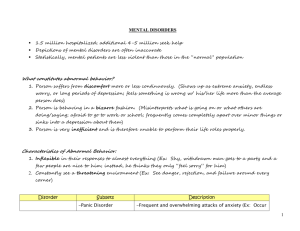
advertisement

Women & Mental Illness The Facts • Despite being common, mental illnesses are under-diagnosed or mis-diagnosed • Less than half of those who meet diagnostic criteria for psychological disorders are identified by doctors Gender Specific Risk Factors • Gender specific risk factors for common mental disorders that disproportionately affect women include: – – – – – gender based violence, socioeconomic disadvantage, low income and income inequality, low or subordinate social status and rank and unremitting responsibility for the care of others (World Health Organization) Examples of Disorders Specific to Women • Premenstrual Dysphoric Disorder • Major Depression during conception and pregnancy • Postpartum Depression • Depression during the transition to menopause Mood Disorders Depression • Depression in women is often more severe than in men; affects twice as many women as men • Many factors influence depression. In women these may include: • biological factors – differences in brain functioning between women and men – women’s unique hormones and reproductive functions • psychological factors – ways in which women are socialized as “women” – how they learn to think, feel and act Unipolar/Major Depression Marked by: • Extreme lethargy • Disturbed sleep, early waking, difficulty getting to sleep and waking up tired • Permanent sense of anxiety • Sensation of utter despair, hopelessness or uselessness • Irritability and physical exhaustion • The disturbance is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition Associated Features: • Lack of concentration Lack of sexual drive Irrational fears such as fear of death, thoughts of suicide, or fear of committing suicide (American Psychiatric Association) Unipolar/Major Depression • Many of the same symptoms as hypothyroidism; hypothyroidism can also trigger depression • Unipolar depression, predicted to be the second leading cause of global disability burden by 2020, is twice as common in women (World Health Organization) Seasonal Affective Disorder (SAD) • The symptoms of SAD differ from clinical depression and include: – Low mood, reduced interest in normally pleasurable activities, decreased concentration – Oversleeping (often an increase of 4 hours or more each day) – Low energy and fatigue – Weight gain and carbohydrate/sweets craving – Withdrawal from social contacts – Depression (Mood Disorders Society of Canada) Seasonal Affective Disorder con’t ... • Most people with SAD have unipolar depression, but as many as 20% may have or go on to develop a bipolar disorder • women are eight times more likely to suffer from SAD than men (Mood Disorders Society of Canada) Adolescence • Before adolescence, there is little difference in the rate of depression in boys and girls • Between the ages of 11 and 13 there is a rise in depression rates for girls • By the age of 15, females are twice as likely to have experienced a major depressive episode as males – Females have significantly higher rates of depression, anxiety disorders, eating disorders, and adjustment disorders; males have higher rates of disruptive behaviour disorders (National Institute of Mental Health) Adulthood: Relationships & Work • Stress in general can contribute to depression in persons biologically vulnerable to the illness • The higher incidence of depression in women is not due to greater vulnerability, but to the particular stresses that many women face – e.g., responsibilities at home and work, single parenthood, and caring for children and aging parents • Lack of an intimate, confiding relationship, as well as marital disputes, are often related to depression in women – rates of depression are highest among unhappily married women (National Institute of Mental Health) Adulthood: Reproductive Events • Reproductive events include: menstrual cycle, pregnancy, the post-pregnancy period, infertility, menopause, and sometimes, the decision not to have children • Many women experience certain behavioural and physical changes associated with phases of their menstrual cycles – in some women, these changes are severe, occur regularly, and include depressed feelings, irritability, and other emotional and physical changes (i.e, premenstrual syndrome [PMS] or premenstrual dysphoric disorder [PMDD]) • Postpartum mood changes can range from transient "blues" immediately following childbirth to an episode of major depression to severe, incapacitating, psychotic depression Adulthood: Reproductive Events con’t ... • Pregnancy itself seldom contributes to depression, and having an abortion does not appear to lead to a higher incidence of depression – Women with infertility problems may be subject to extreme anxiety or sadness, though it is unclear if this contributes to a higher rate of depressive illness – Motherhood may be a time of heightened risk for depression because of the stress and demands it imposes • Menopause, in general, is not associated with an increased risk of depression – women more vulnerable to change-of-life depression are those with a history of past depressive episodes (National Institute of Mental Health) Abuse & Depression • women molested as children are more likely to have clinical depression at some time in their lives than those with no such history • a higher incidence of depression among women who have been raped as adolescents or adults • women who experience other commonly occurring forms of abuse, such as physical abuse and sexual harassment on the job, also may experience higher rates of depression • abuse may lead to depression by fostering low self-esteem, a sense of helplessness, self-blame, and social isolation • there may be biological and environmental risk factors for depression resulting from growing up in a dysfunctional family (National Institute of Mental Health) Poverty • Women and children represent seventy-five percent of the North American population considered “poor” • Low economic status brings with it many stresses, including isolation, uncertainty, frequent negative events, and poor access to helpful resources • Sadness and low morale are more common among persons with low incomes and those lacking social supports (National Institute of Mental Health) Later Adulthood • At one time, it was commonly thought that women were particularly vulnerable to depression when their children left home and they were confronted with "empty nest syndrome" and experienced a profound loss of purpose and identity – most studies show no increase in depressive illness among women at this stage of life • However, more elderly women than men suffer from depressive illness – being unmarried (which includes widowhood) is a risk factor for depression (National Institute of Mental Health) Suicide • Four times as many men as women die by suicide; however, women attempt suicide two to three times as often as men (National Institute of Mental Health) Suicide con’t ... • Suicides and attempted suicides are very rare in the absence of current major psychiatric disorders • More than 90% of suicide victims and attempters have at least one current Axis I (mainly untreated) major disorder, most frequently major depressive episode (56-87%), substance use disorders (26-55%) and schizophrenia (6-13%). • Comorbid anxiety and personality disorders as well as serious medical disorders are also frequently present, but they are quite rare as principal (or only) diagnoses (Rihmer, 2007) Suicide (data from Harvard University and the World Mental Health Survey) • Risk factors for suicidal thoughts, plans and attempts are consistent across countries, and include having a mental disorder and being female, younger, less educated, and unmarried • The risk of suicidal thoughts increased sharply during adolescence and young adulthood in every country studied • The strongest risk factor associated with suicidal thoughts and behaviours were mood disorders in high income countries and impulse control disorders in low- and middle-income countries • The risk of making an attempt was highest among those with substance abuse and impulse-control disorders (17 countries: Nigeria, South Africa, Colombia, Mexico, USA, Japan, New Zealand, China, Belgium, France, Germany, Italy, the Netherlands, Spain, Ukraine, Israel, and Lebanon) Anxiety Disorders Post-traumatic Stress Disorder • Violent personal assault, such as rape or mugging, car or plane accidents, military combat, industrial accidents and natural disasters, such as earthquakes and hurricanes, are stressors which have caused people to suffer from PTSD • In some cases, seeing another person harmed or killed, or learning that a close friend or family member is in serious danger has caused the disorder. (Canadian Mental Health Association) Post-traumatic Stress Disorder • The high prevalence of sexual violence to which women are exposed and the correspondingly high rate of Post Traumatic Stress Disorder (PTSD) following such violence, renders women the largest single group of people affected by this disorder Posttraumatic Stress Disorder • The essential feature of posttraumatic stress disorder (PTSD) is the development of characteristic symptoms following exposure to a traumatic event that arouses "intense fear, helplessness, or horror," or in children, "disorganized or agitated behaviour" (American Psychiatric Association 1994, p. 428) • A host of stressors, both natural and manmade, can be traumatizing. • Naturally occurring stressors include natural disasters and medical illnesses. • Man-made events include accidents and acts of violence (e.g., rape, war) Posttraumatic Stress Disorder A. The person has been exposed to a traumatic event in which both of the following were present: (1) the person experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others (2) the person's response involved intense fear, helplessness, or horror. Note: In children, this may be expressed instead by disorganized or agitated behaviour Posttraumatic Stress Disorder B. The traumatic event is persistently re-experienced in one (or more) of the following ways: (1) recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions. Note: In young children, repetitive play may occur in which themes or aspects of the trauma are expressed. (2) recurrent distressing dreams of the event. Note: In children, there may be frightening dreams without recognizable content. (3) acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur on awakening or when intoxicated). Note: In young children, traumaspecific reenactment may occur. (4) intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event (5) physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event Posttraumatic Stress Disorder C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three (or more) of the following: (1) efforts to avoid thoughts, feelings, or conversations associated with the trauma (2) efforts to avoid activities, places, or people that arouse recollections of the trauma (3) inability to recall an important aspect of the trauma (4) markedly diminished interest or participation in significant activities (5) feeling of detachment or estrangement from others (6) restricted range of affect (e.g., unable to have loving feelings) (7) sense of a foreshortened future (e.g., does not expect to have a career, marriage, children, or a normal life span) Posttraumatic Stress Disorder D. Persistent symptoms of increased arousal (not present before the trauma), as indicated by two (or more) of the following: (1) difficulty falling or staying asleep (2) irritability or outbursts of anger (3) difficulty concentrating (4) hyper-vigilance (5) exaggerated startle response E. Duration of the disturbance (symptoms in Criteria B, C, and D) is more than 1 month. F. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. Other Anxiety Disorders • Generalized Anxiety Disorder 55-60% of sufferers are women • Panic Disorder approximately two thirds of those who seek treatment are women • Specific Phobias – 75 to 90% of individuals with animal, natural environment, and situational types of specific phobias are women – 55 to 70% of individuals with fear of heights and bloodinjection-injury phobias are women (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) Generalized Anxiety Disorder A. Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least 6 months, about a number of events or activities (such as work or school performance). B. The person finds it difficult to control the worry. C. The anxiety and worry are associated with three (or more) of the following six symptoms (with at least some symptoms present for more days than not for the past 6 months). Note: Only one item is required in children. (1) restlessness or feeling keyed up or on edge (2) being easily fatigued (3) difficulty concentrating or mind going blank (4) irritability (5) muscle tension (6) sleep disturbance (difficulty falling or staying asleep, or restless unsatisfying sleep) • The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. Panic Disorder (with or without Agoraphobia) A. Both (1) and (2): (1) recurrent unexpected Panic Attacks (2) at least one of the attacks has been followed by 1 month (or more) of one (or more) of the following: (a) persistent concern about having additional attacks (b) worry about the implications of the attack or its consequences (e.g., losing control, having a heart attack, "going crazy") (c) a significant change in behaviour related to the attacks B. The presence or absence of Agoraphobia. Phobias A. Marked and persistent fear that is excessive or unreasonable, cued by the presence or anticipation of a specific object or situation (e.g., flying, heights, animals, receiving an injection, seeing blood). B. Exposure to the phobic stimulus almost invariably provokes an immediate anxiety response, which may take the form of a situationally bound or situationally predisposed Panic Attack. Note: In children, the anxiety may be expressed by crying, tantrums, freezing, or clinging. C. The person recognizes that the fear is excessive or unreasonable. Note: In children, this feature may be absent. D. The phobic situation(s) is avoided or else is endured with intense anxiety or distress. Phobias E. The avoidance, anxious anticipation, or distress in the feared situation(s) interferes significantly with the person's normal routine, occupational (or academic) functioning, or social activities or relationships, or there is marked distress about having the phobia. F. In individuals under age 18 years, the duration is at least 6 months. Specify type: Animal Type; Natural Environment Type (e.g., heights, storms, water); Blood-Injection-Injury Type ; Situational Type (e.g., airplanes, elevators, enclosed places); Other Type (e.g., phobic avoidance of situations that may lead to choking, vomiting, or contracting an illness; in children, avoidance of loud sounds or costumed characters) Personality Disorders Borderline Personality • Girl, Interrupted • Fatal Attraction Borderline Personality Disorder • One in every 33 women, compared with one in every 100 men, are diagnosed with Borderline Personality Disorder • 75% of those diagnosed are women • 75% have been physically or sexually abused (National Institute for Mental Health) Borderline Personality Disorder • Still a controversial diagnosis • Has been one of the most diagnosed and most researched of the personality disorders • The main feature of borderline personality disorder is a pervasive pattern of instability in interpersonal relationships, self-image, and emotions • The road to recovery is long • Often comorbid with other disorders (The Psychiatric Times) From: www.thelastpsychiatrist.com • First, borderline is a heuristic of countertransference: if the psychiatrist feels frustrated, or exasperated, then the patient is borderline. • Second, borderline is meant as a synonym for any of the following: needy, argumentative, touchy/hypersensitive. • Third, it is generally reserved for the following four types: 1. Very attractive female, who comes for problems the psychiatrist considers ordinary: men, work/school, problems with parents, etc. It is diagnosed here most often by female psychiatrists, and carries the connotation: "Grow up.“ 2. Overweight, typically white, female, who needs/wants benzos, especially Klonopin. The implications are lack of self-control, and reliance on external supports. 3. Thin female with a lot of anger. By example, the woman who comes for treatment of "depression" but describes most life events in terms of attacks, sleights, harm, etc.-- i.e., power differentials. 4. Gay man. Borderline Personality Disorder Diagnostic Features: Borderline Personality Disorder is a condition characterized by impulsive actions, rapidly shifting moods, and chaotic relationships. The individual usually goes from one emotional crisis to another. Often there is dependency, separation anxiety, unstable self-image, chronic feelings of emptiness, and threats of self-harm (suicide or selfmutilation). This disorder is only diagnosed when these behaviours become persistent and very disabling/distressing. Borderline Personality Disorder Complications: Completed suicide occurs in 8%-10% of individuals with this disorder, and self-mutilative acts (e.g., cutting or burning) and suicide threats and attempts are very common. Recurrent job losses, interrupted education, and broken marriages are common. Comorbidity: Very stressful or chaotic childhoods are commonly reported (e.g., physical and sexual abuse, neglect, hostile conflict, and early parental loss or separation). Mood disorders, Substance-Related Disorders, Eating Disorders (usually Bulimia), Posttraumatic Stress Disorder, Attention-Deficit/Hyperactivity Disorder, and other Personality Disorders frequently co-occur with this disorder. Eating Disorders Eating Disorders • Eating disorders affect far more women than men, however, the numbers for men are increasing with more gay men than heterosexual men suffering from the disorders (International Journal of Eating Disorders) • Ratio of women to men suffering from anorexia nervosa is estimated at 20:1 • most commonly begins during puberty Axorexia Nervosa • Symptoms include: • Losing a lot of weight. • An inability to maintain a weight that is normal for one’s age and height • An obsessive desire to be thinner • Fear of gaining weight or becoming "fat” • Distorted perception of one’s own body • Allowing weight and shape to overly influence how one feels about themselves • A powerful desire to take control of one’s life and feel competent (National Eating Disorder Information Centre) Bulimia Nervosa • Ratio of women to men suffering from anorexia nervosa is estimated at 20:1 • Symptoms include: • Eating large amounts of food frequently and in one sitting • Feeling out of control and unable to stop eating • Eating quickly and in secret • Feeling uncomfortably full after eating • Feeling guilty and ashamed of the binges (National Eating Disorder Information Centre) Pro-ana (pro-anorexia) and Pro-mia (pro-bulimia) • Fading Obsession – 57 Reasons – Thinspiration – Includes an extensive Tips & Tricks section, including: • Distractions (i.e., things you can do instead of eating) • Fasting • Purging • Secrecy (i.e., how to keep people from being suspicious) 1. General feedback: Midterm projects 2. Discussion: Monster/Violence Against Women 3. Disorders: continued 4. Sexuality Somatoform Disorders Somatoform Disorders • Shared characteristics of somatoform disorders: – physical symptoms or complaints for which there is no organic basis – symptoms may include sensory or motor disability, hypersensitivity, and pain Somatization Disorder • • • • four pain symptoms two gastrointestinal symptoms one sexual symptom one psuedo-neurological symptom Conversion Disorder • Physical, emotional, or sexual abuse can be a contributing cause • Women diagnosed with conversion disorder outnumber men by a 2:1 to 10:1 ratio • Risk of addictions may be high in somatoform disorders because of medications used to manage physical pain History of “Hysteria” • Hysteria comes from the Greek word, hystera, meaning womb • Originally designated a link between certain nervous disorders and diseases of the female sexual and reproductive organs • Therefore, hysteria was thought of as something to which women were exclusively susceptible • Hippocrates’ theory on the wandering womb had a great impact on feelings about the female body and sexuality Hippocrates • Hippocrates, as well as generations of medical thinkers after him, viewed the womb as an independent creature • Because female bodies were thought to crave warmth and moisture, frequent sexual activity was needed to stabilize the uterus • It was thought that unnatural behaviour, such as celibacy or an excess of “male activities,” would drive the uterus to distraction and cause it to wander freely throughout the body • There were various consequences to these travels depending on how far the uterus wandered and where it chose to attach itself, but when the roving organ ultimately came to rest next to the brain, it caused hysteria (Phillips, 2006) The Victorian Era • Estimated that a quarter of all women suffered from hysteria (not surprising since the list of symptoms was 75 pages long) • In the 19th century, female sexual arousal did not have a name, it had a diagnosis • Genital massage was the treatment for hysteria • the vibrator was developed to automate a function that doctors had been performing for their female patients – the relief of physical, emotional and sexual tension through external pelvic massage, culminating in orgasm Further Prevalence Stats from the American Psychiatric Association Prevalence • Depressive disorders account for close to 41.9% of the disability from neuropsychiatric disorders among women compared to 29.3% among men • Leading mental health problems of the elderly are depression, organic brain syndromes and dementias—a majority are women • An estimated 80% of 50 million people affected by violent conflicts, civil wars, disasters, and displacement are women (and children) • Lifetime prevalence rate of violence against women ranges from 16% to 50% • At least one in five women suffer rape or attempted rape in their lifetime Prevalence • 1 in 5 women will experience an episode of major depression during her lifetime • 1 in 3 will experience an anxiety disorder • Anxiety/panic disorder occurs more often in women than men • 85-95 % of people with anorexia or bulimia are women • The risk of PTSD following traumatic experiences is two-fold higher in women than men • Four times as many men as women die by suicide; women attempt suicide 2-3 times more often as men (American Psychiatric Association) The Politics of Diagnosis • Labelling a cluster of symptoms will affect how the individual views the problem – e.g., if a person is told that they are suffering from depression they may ignore other factors that could be contributing to exhaustion, such a lack of sleep, poor exercise and dietary habits • Diagnostic categories are also influenced by stereotypes – Men predominate in aggressive and antisocial disorders; women are most often diagnosed with depression and anxiety (involving passivity and helplessness) The Politics of Diagnosis • Stereotyped descriptions were given to psychologists and psychiatrists who were asked to provide diagnoses (they were also told that the cases might be ‘normal’) – – – – Lower-class men: antisocial Married, middle-class woman: dependent Single, middle-class woman: histrionic/hysterical Married, upper-class man: normal *both male and female therapists were influenced by the stereotypes about gender and class The Politics of Diagnosis: PMDD • Premenstrual Dysphoric Disorder • The woman experiences 5 symptoms during the prementrual phase: – depressed and hopeless feelings, marked anxiety and tension, tendency toward sudden sadness and crying, persistent anger or irritability, lethargy, decreased interest in activities, appetite changes, insomnia, a sense of being out of control, and physical symptoms (e.g., bloating, headache) • APA Committee on Women unanimously opposed the inclusion of PMDD in the DSM, as did more than 6 million others (evidenced by letters, petitions)