Pain in Endometriosis
advertisement

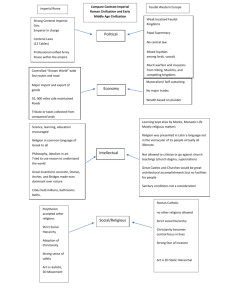
WHY DOES ENDOMETRIOSIS CAUSE SO MUCH PAIN? Dr Michael W Platt MA MB BS FRCA Lead Clinician in Pain Medicine, Consultant in Anaesthetics, Honorary Senior Lecturer, Faculty of Medicine, Imperial College London, Department of Anaesthetics St Mary's Hospital, Imperial College Healthcare NHS Trust Praed Street, London W2 1NY • The pain associated with Endometriosis is the most difficult symptom to cope with for most women. For many, the pain they suffer severely interferes with every day life. It can be constant or it can be cyclical and coincide with a woman’s period. 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College What is pain? • • • • • • Emotional Sensory Acute or Chronic Totally subjective Can be described qualitatively Can be graded quantitatively 2007 Dr Michael W Platt Imperial College What is pain? 2007 Dr Michael W Platt Imperial College What is pain? • Can be graded quantitatively: 2007 Dr Michael W Platt Imperial College Why do we have pain? • • • • • Recognition of self Protection from trauma Reduction of trauma Warning sign of illness Warning sign of infection 2007 Dr Michael W Platt Imperial College What happens when pain is absent? • Congenital insensitivity to pain • Sensory nerve damage secondary to disease – – – – – 2007 Diabetes Stroke Trauma Syphilis Leprosy Dr Michael W Platt Imperial College Pain • Acute (physiological) Pain: – An unpleasant sensory and emotional experience associated with actual or potential tissue damage. • Chronic (pathological, intractible) Pain: – Pain in the absence of, or persisting following the removal of, a noxious stimulus. 2007 Dr Michael W Platt Imperial College PAIN • Acute: Post-trauma, surgery etc. • Chronic: – – – – Neuropathic pain Mechanical pain Chronic inflammation Complex regional pain syndrome • Cancer pain 2007 Dr Michael W Platt Imperial College Complicated neurobiology of pain • Not a simple ‘hard-wired’ system. • Long-term changes occur in the PNS and CNS following a noxious stimulus. • This ‘plasticity’ changes the body’s response to further stimuli 2007 Dr Michael W Platt Imperial College Pain Pathways • • • • • • • Nociceptor Axon Dorsal Root Ganglion Dorsal Root Internuncial neurones Cross-over to opposite side Thalamus and Cortex 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College Peripheral sensitisation • Inflammatory response: Release of mediators from mast cells etc: – – – – Substance P neurokinin A calcitonin gene-related peptide lead to further release of ‘inflammatory soup’: • K, 5-HT, bradykinin, histamine etc • Act to sensitise high-threshold receptors 2007 Dr Michael W Platt Imperial College ‘Neuropathic pain’ • Burning, sharp, stabbing sensations • eg diabetic neuropathy, post-amputation pain etc. • Treatment of peripheral neuropathic pain include tricyclic antidepressants, anticonvulsants, clonidine, opioids, local anaesthetics and anti-arrhythmic agents. 2007 Dr Michael W Platt Imperial College Sympathetic nervous system • Important role in generation and maintenance of chronic pain states. • ‘Complex regional pain syndromes: – Sympathetic dysfunction: • • • • 2007 vasomotor & sudomotor changes abnormal hair & nail growth osteoporosis sensory symptoms: burning, hyperalgesis, allodynia Dr Michael W Platt Imperial College Gate Theory of Pain 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College Central sensitisation • Changes that occur in the dorsal horn in response to an injury, following barrage of stimuli into the horn. • Phenomenon of ‘wind-up’ involving the NMDA receptor, making neurons more sensitive - ie sensitising them. • Expansion in receptive field size. 2007 Dr Michael W Platt Imperial College Ascending tracts • 2nd order neurons ascend in spinothalamic, spinoreticular and spinomesencephalic tracts. • Terminate in structures throughout the brain stem, thalamus, and cortex. • Thalamus has 2 main groups of relays: – sensory discriminative aspects – affective-motivational aspects 2007 Dr Michael W Platt Imperial College Descending modulation • descending inhibitory modulation from: – – – – – hypothalamus PAG locus coeruleus nucleus raphe magnus etc • Involves opioids, 5-HT, n-adr, GABA 2007 Dr Michael W Platt Imperial College Visceral Pain • There are specific nociceptors originating in viscera. • They respond to: – – – – 2007 tension (contraction) chemical nociception sensitisation of nociceptors effects of ischaemia Dr Michael W Platt Imperial College Concept of referred pain • Visceral nociceptors rarely activated • Much more common to activate somatic nociceptors • Spinal cord and brain interpret visceral signals as emanating from somatic source • Convergence of visceral and somatic afferents may account for this 2007 Dr Michael W Platt Imperial College Diagnosis of Pain in Endometriosis • Acute, cyclical pain – due to pressure, chemical irritation, nerve compression • Chronic, non-cyclical pain – due to neuropathic pain, sources outside the pelvis (back, groin, etc.) • Other visceral pain – especially bladder pain. 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College 2007 Dr Michael W Platt Imperial College Measurement of Pain • Visual Analogue Score – make as objective as possible – Straight line 10 cm long – No other markings • Personality inventories – Help to score chronic pain in terms of personality type and stress markers. 2007 Dr Michael W Platt Imperial College Treatment of Pain in Endometriosis • Acute Pain: – – – – – 2007 NSAIDS Hormonal Oral Contraceptive Systemic analgesia, opioids Other techniques (TENS, Acupuncture) Dr Michael W Platt Imperial College Pain Ladder • Minor pain: paracetamol, aspirin • Moderate pain: – combination with minor opioids • Co-proxamol (propoxifine), Co-dydramol (codeine) – Minor opioids alone - eg Pethidine, Tramadol • Severe pain: – Opioids: 2007 Morphine etc. Dr Michael W Platt Imperial College Endometriosis and Inflammatory Pain: Use of NSAIDS • Cyclo-oxygenase pathway blocked – 2 forms: • COX1 & COX2 • COX1 always present • COX2 only induced by inflammation • Also have central role, where both COX1 & COX2 are found as neuro-transmitters 2007 Dr Michael W Platt Imperial College NSAIDS • COX 2 antagonists preferable where there is high-risk of peptic ulceration / bleeding • Still not 100% guarantee. 2007 Dr Michael W Platt Imperial College Treatment of Pain in Endometriosis • Chronic / Intractable Pain: – Multiple modality pain clinic - holistic approach – Drugs – Nerve blocks – TENS, Acupuncture – Physio, occupational Ther., Psychology 2007 Dr Michael W Platt Imperial College Neuropathic Pain in Endometriosis • Not responsive to opioids • Two main classes of drugs used: – Tricyclic antidepressants (esp Amitriptyline) – Anti-epileptics: • • • • 2007 Carbamazepine Sodium valproate Clonazepam Gabapentin (Pregaballin) Dr Michael W Platt Imperial College Gracilis Adductor longus Adductor brevis Adductor magnus Obturator externus Obturator internus 2007 Dr Michael W Platt Imperial College Other complicating factors • Psychosocial & spiritual processes strongly influence the impact and expression of pain. • (Saunders 1985, Portenoy 1992; Breitbart 1994) 2007 Dr Michael W Platt Imperial College Some factors: • Pain interrelated with: – depression (r = 0.33 with pain) – lack of family support (r = -0.15 with pain) – desire for death (r = 0.47 with depression) 2007 Dr Michael W Platt Imperial College Some correlates with severe pain: • • • • • • • • 2007 Patient anxiety: r = 0.30 Communication problems: r = 0.29 Constipation: r = 0.24 Poor co-ordination: r = 0.21 Family anxiety: r = 0.19 Nausea: r = 0.19 Vomiting: r = 0.13 Other symptoms: r = 0.11 Dr Michael W Platt Imperial College Factors that diminish quality of life: Pain Other symptoms Psychological distress Spiritual/existential distress Family distress Social distress Financial needs Health care concerns (eg poor communication) Perception & appraisal of pain Expression of suffering A MODEL OF SUFFERING Summary • The pain system is a very complex one. • Endometrial Pain may be difficult to treat due to a variety of causes, and these should be addressed in the management of the patient: • Adequate pain assessment, including those factors which are inter-related is essential. 2007 Dr Michael W Platt Imperial College