Template to create a scientific poster
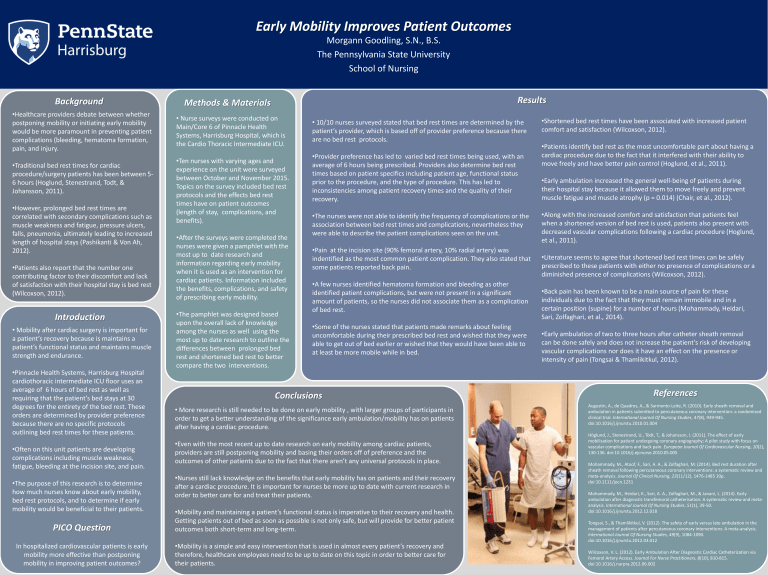
Early Mobility Improves Patient Outcomes
Morgann Goodling, S.N., B.S.
The Pennsylvania State University
School of Nursing
Background
• Healthcare providers debate between whether postponing mobility or initiating early mobility would be more paramount in preventing patient complications (bleeding, hematoma formation, pain, and injury.
• Traditional bed rest times for cardiac procedure/surgery patients has been between 5-
6 hours (Hoglund, Stenestrand, Todt, &
Johansson, 2011).
• However, prolonged bed rest times are correlated with secondary complications such as muscle weakness and fatigue, pressure ulcers, falls, pneumonia, ultimately leading to increased length of hospital stays (Pashikanti & Von Ah,
2012).
• Patients also report that the number one contributing factor to their discomfort and lack of satisfaction with their hospital stay is bed rest
(Wilcoxson, 2012).
Introduction
• Mobility after cardiac surgery is important for a patient’s recovery because is maintains a patient’s functional status and maintains muscle strength and endurance.
• Pinnacle Health Systems, Harrisburg Hospital cardiothoracic intermediate ICU floor uses an average of 6 hours of bed rest as well as requiring that the patient’s bed stays at 30 degrees for the entirety of the bed rest. These orders are determined by provider preference because there are no specific protocols outlining bed rest times for these patients.
• Often on this unit patients are developing complications including muscle weakness, fatigue, bleeding at the incision site, and pain.
• The purpose of this research is to determine how much nurses know about early mobility, bed rest protocols, and to determine if early mobility would be beneficial to their patients.
PICO Question
In hospitalized cardiovascular patients is early mobility more effective than postponing mobility in improving patient outcomes?
Methods & Materials
• Nurse surveys were conducted on
Main/Core 6 of Pinnacle Health
Systems, Harrisburg Hospital, which is the Cardio Thoracic Intermediate ICU.
• Ten nurses with varying ages and experience on the unit were surveyed between October and November 2015.
Topics on the survey included bed rest protocols and the effects bed rest times have on patient outcomes
(length of stay, complications, and benefits).
• After the surveys were completed the nurses were given a pamphlet with the most up to date research and information regarding early mobility when it is used as an intervention for cardiac patients. Information included the benefits, complications, and safety of prescribing early mobility.
• The pamphlet was designed based upon the overall lack of knowledge among the nurses as well using the most up to date research to outline the differences between prolonged bed rest and shortened bed rest to better compare the two interventions.
Conclusions
• More research is still needed to be done on early mobility , with larger groups of participants in order to get a better understanding of the significance early ambulation/mobility has on patients after having a cardiac procedure.
• Even with the most recent up to date research on early mobility among cardiac patients, providers are still postponing mobility and basing their orders off of preference and the outcomes of other patients due to the fact that there aren’t any universal protocols in place.
• Nurses still lack knowledge on the benefits that early mobility has on patients and their recovery after a cardiac procedure. It is important for nurses be more up to date with current research in order to better care for and treat their patients.
• Mobility and maintaining a patient’s functional status is imperative to their recovery and health.
Getting patients out of bed as soon as possible is not only safe, but will provide for better patient outcomes both short-term and long-term.
• Mobility is a simple and easy intervention that is used in almost every patient’s recovery and therefore, healthcare employees need to be up to date on this topic in order to better care for their patients.
Results
• 10/10 nurses surveyed stated that bed rest times are determined by the patient’s provider, which is based off of provider preference because there are no bed rest protocols.
• Provider preference has led to varied bed rest times being used, with an average of 6 hours being prescribed. Providers also determine bed rest times based on patient specifics including patient age, functional status prior to the procedure, and the type of procedure. This has led to inconsistencies among patient recovery times and the quality of their recovery.
• The nurses were not able to identify the frequency of complications or the association between bed rest times and complications, nevertheless they were able to describe the patient complications seen on the unit.
• Pain at the incision site (90% femoral artery, 10% radial artery) was indentified as the most common patient complication. They also stated that some patients reported back pain.
• A few nurses identified hematoma formation and bleeding as other identified patient complications, but were not present in a significant amount of patients, so the nurses did not associate them as a complication of bed rest.
• Some of the nurses stated that patients made remarks about feeling uncomfortable during their prescribed bed rest and wished that they were able to get out of bed earlier or wished that they would have been able to at least be more mobile while in bed.
• Shortened bed rest times have been associated with increased patient comfort and satisfaction (Wilcoxson, 2012).
• Patients identify bed rest as the most uncomfortable part about having a cardiac procedure due to the fact that it interfered with their ability to move freely and have better pain control (Hoglund, et al., 2011).
• Early ambulation increased the general well-being of patients during their hospital stay because it allowed them to move freely and prevent muscle fatigue and muscle atrophy (p = 0.014) (Chair, et al., 2012).
• Along with the increased comfort and satisfaction that patients feel when a shortened version of bed rest is used, patients also present with decreased vascular complications following a cardiac procedure (Hoglund, et al., 2011).
• Literature seems to agree that shortened bed rest times can be safely prescribed to these patients with either no presence of complications or a diminished presence of complications (Wilcoxson, 2012).
• Back pain has been known to be a main source of pain for these individuals due to the fact that they must remain immobile and in a certain position (supine) for a number of hours (Mohammady, Heidari,
Sari, Zolfaghari, et al., 2014).
• Early ambulation of two to three hours after catheter sheath removal can be done safely and does not increase the patient’s risk of developing vascular complications nor does it have an effect on the presence or intensity of pain (Tongsai & Thamlikitkul, 2012).
References
Augustin, A., de Quadros, A., & Sarmento-Leite, R. (2010). Early sheath removal and ambulation in patients submitted to percutaneous coronary intervention: a randomised clinical trial. International Journal Of Nursing Studies, 47(8), 939-945. doi:10.1016/j.ijnurstu.2010.01.004
Höglund, J., Stenestrand, U., Tödt, T., & Johansson, I. (2011). The effect of early mobilisation for patient undergoing coronary angiography; A pilot study with focus on vascular complications and back pain. European Journal Of Cardiovascular Nursing, 10(2),
130-136. doi:10.1016/j.ejcnurse.2010.05.005
Mohammady, M., Atoof, F., Sari, A. A., & Zolfaghari, M. (2014). Bed rest duration after sheath removal following percutaneous coronary interventions: a systematic review and meta-analysis. Journal Of Clinical Nursing, 23(11/12), 1476-1485 10p. doi:10.1111/jocn.1231
Mohammady, M., Heidari, K., Sari, A. A., Zolfaghari, M., & Janani, L. (2014). Early ambulation after diagnostic transfemoral catheterisation: A systematic review and metaanalysis. International Journal Of Nursing Studies, 51(1), 39-50. doi:10.1016/j.ijnurstu.2012.12.018
Tongsai, S., & Thamlikitkul, V. (2012). The safety of early versus late ambulation in the management of patients after percutaneous coronary interventions: A meta-analysis.
International Journal Of Nursing Studies, 49(9), 1084-1090. doi:10.1016/j.ijnurstu.2012.03.012
Wilcoxson, V. L. (2012). Early Ambulation After Diagnostic Cardiac Catheterization via
Femoral Artery Access. Journal For Nurse Practitioners, 8(10), 810-815. doi:10.1016/j.nurpra.2012.06.002