Mensah
advertisement

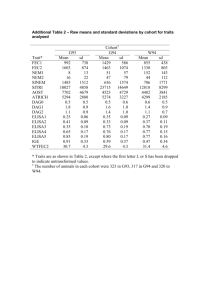
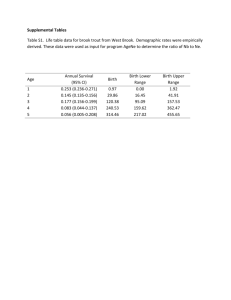
Latent Class Analysis of the Breadth, Severity and Stability of Child Health Inequalities Mensah FK, Nicholson JM, Headley L, Carlin JB, Berthelsen D, Wake M Acknowledgments NHMRC Capacity Building Grant, MCRI, RCH and University of Melbourne Professors Melissa Wake, John Carlin Professor Jan Nicholson, Parenting Research Centre, Melbourne Liz Headley, Victorian Public Health Training Scheme and Monash University Professor Donna Berthelsen, Queensland University of Technology Gender Equality Network, Economic and Social Research Council UK Dr Wendy Sigle-Rushton, London School of Economics Professors John Hobcraft and Kathleen Kiernan, Department of Social Policy and Social Work and Institute of Effective Education, University of York Multiple Outcomes of Health Inequality Models have often focused on single outcomes – fail to consider breadth of impact and address “multifinality” Alternative strategies – summary indices – multiple outcome models Example to follow: Impact of socioeconomic position on children’s risks for multiple problems in physical, socio-emotional and cognitive functioning The Longitudinal Study of Australian Children (LSAC) Two national cohorts of ~5,000 children each Infants (0-1 yrs) & Kindergarten children (4-5 yrs) in 2004 Followed up every two years Conducted by Australian Govt. Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA), Australian Institute of Family Studies (AIFS), and the Australian Bureau of Statistics (ABS) with advice from a national research consortium www.aifs.gov.au/growingup/ Physical, Psychosocial and Cognitive Difficulties at 4-5 (Birth cohort) 75 64.3 50 % 32.6 33.1 25 9.2 0 Most advantaged qu. 2 qu. 3 at least one problem in 2 or more domains qu. 4 Least advantaged at least one problem in all 3 domains Latent Class Analysis (LCA) • • • • • Groups children to reflect key differences Accounts for inter-correlations between measures Similar to cluster analysis, but is model based (probabilistic) Gives model fit statistics to determine number of categories Uses specialist software such as Mplus E.g. Multiple problem behaviours in adolescence Fergusson et al. 1994, Journal of Child Psychology & Psychiatry 35 (6) 1123-1140 Subtypes and severity of peer victimisation Nylund et al. 2007, Child Development 78 (6) 1706-1722 Study design Age 4-5 Age 6-7 Age 8-9 K cohort (wave 1) (N=3,711) K cohort (wave 2) (N=2,563) K cohort (wave 3) (N=3,080) B cohort (wave 3) (N=3,608) (replication sample) Indicators and Measures Global health measure Excellent / Very good / Good / Fair or Poor Special health care needs No / Yes (condition lasting for at least 12 months requiring medicines, medical care, health or educational services ) Asthma diagnosis No / Yes Sleep difficulties 0,1,2+ (getting to sleep, sleeping alone, waking during the night) Injuries 0,1,2+ in the last year Body mass index Underweight / Normal / Overweight / Obese Peds Quality of Life Physical, Social, Emotional and School Scores Strengths and Difficulties Pro-social, Conduct, Emotional, Hyperactivity and Peers Scores Peabody Picture vocabulary test Direct Assessment of Language Development Who am I? (Age 4-5) Direct Assessment of School Readiness Teacher rating scales (Age 6-7, 8-9) Language and Literacy, Mathematical Thinking Model fit parameters (K cohort age 4-5) 278,000 Akaike information criteria (AIC) Bayesian information criteria (BIC) Adjusted BIC 276,000 274,000 272,000 270,000 268,000 266,000 1 2 3 4 Number of classes 5 6 P value 0.000 0.014 0.048 0.188 0.327 Classes 0.75 0.25 0.59 0.33 0.07 0.55 0.20 0.19 0.07 0.45 0.22 0.20 0.09 0.05 0.38 0.22 0.15 0.12 0.09 0.04 Profiles from 3 class model (K cohort age 4-5) Mean score for Peds Quality of Life: Healthiest (59.5%) Moderate (33.4%) Severe (7.2%) Physical 87.1 79.8 63.0 Social 90.3 77.4 52.1 Emotional 78.5 64.4 56.8 School 93.3 83.8 58.2 Pro-social 8.3 7.0 6.8 Conduct difficulties 1.7 3.7 3.6 Emotional difficulties 1.1 2.3 3.7 Hyperactivity 2.7 4.6 5.0 Difficulties With Peers 1.1 2.2 3.2 Language PPVT 65.0 63.6 59.7 School readiness Who am I 65.2 63.4 61.1 Strengths and difficulties Profiles from 3 class model (K cohort age 4-5) Percent of children with Healthiest (59.5%) Moderate (33.4%) Severe (7.2%) Fair or poor health 1.0 3.1 9.3 Special health care need 7.2 17.2 38.6 Asthma diagnosis 16.9 26.5 34.0 2 or more sleep problems 7.1 21.3 23.3 2 or more injuries 2.8 6.3 6.9 Underweight 4.9 5.0 7.0 Overweight/obese 19.3 20.4 21.1 Replication and consistency of 3 class structure B cohort K cohort Age 4-5 (%) Age 4-5 (%) Age 6-7 (%) Age 8-9 (%) (N=3,608) (N=3,711) (N=2,563) (N=3,080) Healthiest 54.7 59.2 60.3 54.9 Moderate 38.4 33.4 30.5 36.5 Severe 6.9 7.4 9.2 8.6 Common sample across 3 waves of the K cohort N=1,685 Age 4-5 (%) Age 6-7 (%) Age 8-9 (%) Healthiest 64.7 64.2 60.0 Moderate 30.1 29.0 33.5 Severe 5.2 6.7 6.6 Classification (K cohort age 4-5) ESTIMATED CLASS PROPORTIONS AND COUNTS 1 (Healthiest) 0.592 2196 2 (Moderate) 0.334 1241 3 (Severe) 0.074 274 CLASSIFICATION QUALITY (Entropy) 0.809 CLASSIFICATION OF INDIVIDUALS BASED ON THEIR MOST LIKELY LATENT CLASS MEMBERSHIP 1 (Healthiest) 0.595 2208 2 (Moderate) 0.334 1238 3 (Severe) 0.072 265 A further technique for classification after LCA Technique of random draws on the basis of probabilities http://www.statmodel.com/download/meantest2.pdf Takes into account both bias and uncertainty Similar principles to multiple imputation Implemented in Mplus as a default Can also be implemented in Stata Feeds into descriptive analysis and regression models Health Inequalities - K cohort age 4-5 Most healthy (%) Moderate (%) Severe (%) Moderate 69.5 27.7 2.8 Severe 69.2 27.7 3.1 3rd Quintile 69.3 24.4 6.3 4th Quintile 56.6 36.2 7.2 Least advantaged 47.5 37.9 14.6 Most advantaged 61.2 33.0 5.9 2nd Quintile 63.0 31.3 5.6 3rd Quintile 56.7 36.6 6.7 4th Quintile 54.0 39.2 6.9 Least advantaged 39.4 43.4 17.2 Girls Most advantaged 2nd Quintile Boys 0 0.2 0.4 0.6 Proportion of children 0.8 Stability through childhood (K cohort) Age 4-5 Age 6-7 Age 6-7 Healthiest (%) Severe (%) Age 8-9 Healthiest (%) Moderate (%) Moderate (%) Severe (%) Healthiest 78.8 18.5 2.8 73.0 25.5 1.5 Moderate 41.2 50.1 8.7 39.6 48.6 11.8 Severe 16.5 38.9 44.6 15.7 45.3 39.0 Healthiest 77.7 22.0 0.3 Moderate 31.1 55.7 13.3 Severe 15.5 47.3 37.2 Conclusions, continuation and discussion Clear and reproducible groups reflecting degree of difficulties Powerful social grading Strong continuity from early to mid-childhood Potential to examine predictors, prognosis and associated costs For discussion: Criteria for evaluating validity Utility of this type of indicator beyond academic research