chapter23
advertisement

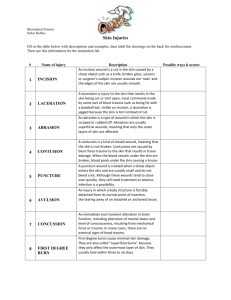
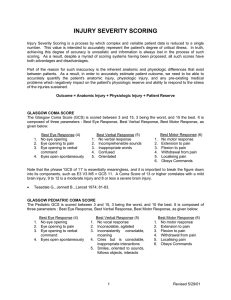
• Acute & chronic pain differ in their neurological processing, impact, treatment • Acute – short duration, subsequent healing • Chronic long duration with underlying cause – can be chronic malignant with cancer or chronic benign with no disease • Nociceptors are activated, cause autonomic (sympathetic) and emotional response and behaviors • Pain stimuli produces physiological & psychic arousal, responses, and either precise localization or chronic pain • Sharp pain – activates lightly myelinated fibers • Tissue damage, inflammation activates unmyelinated fibers • Initial pain, with glutamate as the transmitter, causes primary hyperalgesia, then NO is released that causes secondary hyperalgesia (hurts more) • Pain pathway includes mesencephalon where impulses are sent to the hypothalamus, limbic system, and cortex for endocrine, autonomic, emotional components and can stimulate the analgesia pathway • Narcotics cause analgesia by binding to endorphin receptors of the analgesia pathway, that stimulate fibers to release transmitters that inhibit pain signals • Referred pain and phantom pain are results of pain perception • Referred pain – pain from internal organs that is perceived from the skin or muscles, because of the dermatome of incoming signal • Phantom pain after amputation • Pain from cancer is variable in nature & pathology, from tumor mass with compression, distention, occlusion • Somatic pain – tissue damaging • Neuropathic pain – altered neural processing • Peripheral analgesics inhibit prostaglandin production, by blocking the cyclooxygenase pathway, which raises pain threshold and reduces pain perception • Narcotics act centrally, bind to receptors in spinal cord, brain stem, cerebrum that endorphins bind to and can also produce constipation, nausea, euphoria • Use can lead to tolerance (decreased effect) • Nonmedical techniques can ameliorate pain, includes counterstimulation with accupuncture, electric stimulation, ultrasound • Headaches can be symptomatic of underlying pathology, and headache syndromes can produce significant disability • Pain sensitive structures of the head are the venous sinuses and veins, dura mater at the base of the brain, meningeal arteries, and subarachnoid space • Nerves involved are the trigeminal, vagus, and upper cervical nerves • Eye, ear, sinuses also sensitive • Headache types: • Tension – from muscle tension • Migraine headaches – one side of the head accompanied by nausea and vomiting, arteriolar constriction, decreased cerebral blood flow – classic has prodrome, common doesn’t, complicated includes numbness or TIA like symptoms • Cluster – occur in a cluster of time, similar to migraine pain • Severe traumatic injury results from burns or mechanical injury, producing wounds • Abrasion – removal of epidermis, usually minor • Contusion – bruise, damage to small blood vessels with blood loss into tissue spaces, surface unbroken • Hematoma – focal pooling of blood in tissue • Laceration – tear of skin or organ surface • Bone fractures – incomplete, greenstick from bending, simple with only 2 fragments, comminuted with many fragments, through skin is compound, depressed in skull, pathological because of weakness • Responses help to maintain blood flow & metabolic support with traumatic injury • Craniocerebral trauma is serious because the brain is delicate, secondary brain injury from local infarcts, hydrocephalus, hypoxia 2ndary to initial injury • Concussion – period of lost or altered consciousness from brain injury, usually caused by torsion of cerebrum around the brain stem, reversible interruption of function, severe concussions result in coma • Coup-contrecoup injury causes edema, hemorrahge, laceration • Hematoma effects are determined by vessels involved & location relative to meninges • Epidural hematoma – arterial blood outside of dura that causes pressure • Subdural – from bridging vein, slow development, also expands • Closed head injury – no breach of vasculature • spinal cord trauma is linked to vertebral trauma • Most vulnerable are cervical vertebrae and upper lumbar • Spinal shock usually is 1st response – loss of conscious movement, sensation, reflexes from initial trauma • Thoracic cage trauma can disrupt respiratory movements, lacerate lungs or heart • Flail chest with rib fractures • Pneumothorax with opening into pleural spaces – open-sucking, vs tension • Heart & great vessels can have contusions, dysrhythmia, bleeding with trauma, tamponade • Abdominal trauma can cause contusion, laceration, rupture of viscera, penetration cause hemorrhage and infection • Spleen is especially vulnerable, can cause bleeding • Evisceration – abdominal organs escape from the abdomen • Peritonitis caused by spilling of secretions and contents, infection • Athletes have trauma of limbs • Ligament tears are sprains • Avulsion – ligament pulls bone off • Subluxation – dislocation of joint • Rupture of muscles from excessive load • Thermal injuries results from heat delivery faster than the skin can dissipate it, classified on depth of damage • Burns cause fluid loss, infection because of the loss of the barrier • 1st degree – epidermis • 2nd degree – epidermis & part of dermis • 3rd degree (full thickness) – through dermis to subcutaneous tissue • Smoke inhalation – systemic hypoxia & acidosis, toxic components that enter blood, damage alveolar surfaces – exudate forms, surfactant is inactivated