Digestive enzymes
advertisement

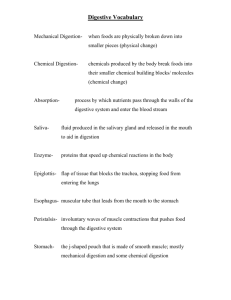
Digestive enzymes mirka.rovenska@lfmotol.cuni.cz Various organs in digestion and absorption Pancreas is the major organ that synthesizes the digestive enzymes Small intestine is a principal site of digestion and absorption …and there are 3 compartments where digestion and absorption occur: Pancreatic enzymes together with bile are poured into the lumen of the descending part of the duodenum Digestion of oligomers of AA and saccharides is accomplished by the enzymes in the luminal plasma membranes of enterocytes; these enzymes – usually glycoproteins Hydrolysis of di- and tripeptides occurs in the cytoplasm of enterocytes Zymogens Digestive enzymes are usually synthesized as larger inactive precursors – zymogens Otherwise they would digest the tissues that synthesize them: acute pancreatitis: premature activation of digestive enzymes produced by pancreas → auto-digestion of pancreas; activated phospholipase A2 converts lecithin to lysolecithin that can damage cell membranes Synthesis of zymogens Proteins destined for secretion are synthesized on polysomes of the RER Their N-terminus contains a signal sequence → release of the protein into ER; then, the signal sequence may be clipped off Transport to the Golgi complex The proteins are stored in vesicles; after stimulus, granules move to the luminal plasma membrane (PM) and fuse with PM …exocytosis Zymogens are activated by proteolysis Proenzymes (zymogens) are activated by proteolytic cleavage in the lumen of the GIT: pepsinogen trypsinogen chymotrypsinogen proelastase procarboxypeptidases prophospholipases Activation of pepsinogen Pepsinogen is secreted from the stomach cells Pepsinogen is activated by the proteolytic removal of 44 AA from its N-terminus – either as an intramolecular reaction or by active pepsin This reaction takes place at pH values below 5 Activation of pancreatic zymogens in the lumen of the small intestine chymotrypsinogen, proelastase, procarboxypeptidases, prophospholipase enteropeptidase (produced in duodenum) trypsinogen trypsin – 6 N-terminal AA autocatalytic activation chymotrypsin, elastase, carboxypeptidases, phospholipase „Strategies“ that prevent premature zymogen activation At pH>2, the peptide (44 AA) clipped of pepsinogen remains bound to pepsin, masking its active site; it is released by a drop of pH below 2 or by further degradation by pepsin Pancreatic secretory trypsin inhibitor (PSTI), a small polypeptide, blocks any trypsin that is erroneously activated within the pancreas Regulation of secretion Through secretagogues that interact with the receptors on the surface of the exocrine cells → signal cascade leading to fusion of granules with PM Organ Secretion Secretagogue Salivary gland NaCl, amylase Stomach HCl, pepsinogen acetylcholine, histamine, gastrin (peptide) Pancreas NaCl, enzymes acetylcholine, cholecystokinin NaHCO3, NaCl secretin acetylcholine Cholecystokinin: peptide secreted by cells of small int. after stimulation by AA and peptides from gastric proteolysis, by FA, and by acid pH Secretin: peptide secreted by cells of small int.; stimulated by luminal pH < 5 DIGESTION OF PROTEINS By peptidases (proteases): endopeptidases – attack internal bonds: • • • • pepsin trypsin chymotrypsin elastase exopeptidases – cleave off 1 AA at a time from the: • • C-terminus – carboxypeptidases N-terminus – aminopeptidases Classes of peptidases Type Active site pH optimum Serine proteases Ser, His, Asp 7-9 Cysteine proteases Cys, His 3-6 Aspartate proteases 2 x Asp 2-5 Metalloproteases Zn2+ (coordinated to AA) 7-9 Peptidases hydrolyze the peptide bond …and differ in substrate specificity: Pepsins Acid in the stomach serves to kill off microorganisms and to denature proteins (denaturation makes proteins more susceptible to proteolysis) Pepsins are acid stable and pH optimum is about 2!!! Major products of pepsin action: larger peptide fragments and some free AA; this mix = peptone Importance lies mainly in generation of peptides and AAs that stimulate cholecystokinin release in the duodenum Pancreatic enzymes trypsin chymotrypsin elastase carboxypeptidases Active at neutral pH depend on neutralization of gastric HCl by pancreatic NaHCO3 The combined action of pancreatic peptidases results in the formation of free AA and small peptides (2-8 AA) Intestinal peptidases Luminal surface of intestinal epithelial cells contains endopeptidases, aminopeptidases, and dipeptidases that cleave oligopeptides released by pancreatic peptidases Products: AA, di- and tripeptides → absorbed by enterocytes Di- and tripeptides are hydrolyzed by intestinal cytoplasmic peptidases AA are absorbed into the portal blood DIGESTION OF SACCHARIDES 1) Polysaccharides (starch, glycogen) are attacked by -amylase, which is present in saliva and pancreatic juice (more important) -amylase attacks the internal -1,4-glucosidic bonds products: maltose, maltotriose, -limit dextrins 2) Hydrolysis of oligosaccharides is carried out by surface enzymes of the intestinal epithelial cells – disaccharidases and oligosaccharidases These enzymes – often exoglycosidases Saccharide absorption End products: monosaccharides, mainly D-glucose, D-galactose, D-fructose These are transported by a carrier-mediated process into enterocytes and then into the blood of the portal venous system Not everything can be digested Many plant polymers, including celluloses, hemicelluloses, inulin, pectin, are resistant to human digestive enzymes A small percentage of this „dietary fibre“ is hydrolyzed and then anaerobically metabolized by the bacteria of the lower intestinal tract This bacterial fermentation produces H2, CH4, CO2, H2S, acetate, propionate, butyrate, lactate Lactase deficiency Experienced as milk intolerance Cause: a) genetic defect b) decline of lactase activity with age c) decline of activity due to an intestinal disease Inability to absorb lactose accumulation and bacterial fermentation of lactose production of gas (distension of gut, flatulence); osmotically active solutes draw water into the intestinal lumen (diarrhea) Lysozyme Hydrolyzes -1,4-glycosidic bonds in the bacterial cell wall polysaccharide peptidoglycan Kills only some types of bacteria DIGESTION OF LIPIDS Lipids – sparingly or not at all soluble in aqueous solutions Two problems have to be overcome: poor accessibility of the substrate to the enzyme aggregation of products of hydrolysis to larger complexes that are hard to absorb Steps in lipid digestion & absorption Lipid digestion is initiated in stomach In the stomach, acid-stable lipase, secreted by stomach (gastric lipase) and by lingual glands (lingual lipase), converts TG mostly into FA and 1,2-diacylglycerols (small amount of monoAG is also produced) The products possess both polar and non-polar groups act as surfactants: stabilize the water-lipid interface dispersion of the lipid phase into smaller droplets (emulsification) better availability of the substrate to the lipases. These lipases have the unique ability to initiate the degradation of maternal milk fat globules Pancreatic lipase Cleaves acylglycerols mainly to FA and 2-monoacylglycerols Requires solubilization of the substrate Also requires colipase (secreted by the pancreas) that anchors and activates the enzyme Absorption of resulting FA and monoAG requires bile salts micelles Digestion of phospholipids By phospholipases, especially by phospholipase A2 (requires bile acids for activity): FA and lysophospholipids are absorbed from the bile acid micelles In the intestinal mucosa, the absorbed lysophospholipids are reacylated with acyl-CoA Hydrolysis of cholesterol esters By pancreatic cholesterol esterase The free cholesterol is transported in the bile acid micelles and absorbed through the brush border Here, it is reacylated with acyl-CoA Bile acid micelles solubilize lipids Primary bile acids are synthesized by the liver and in peroxisomes, they are conjugated with glycine or taurine (H2N-CH2CH2SO3-) A portion of the primary bile acids is subjected to the modifications by intestinal bacteria → secondary bile acids Primary and secondary bile acids are reabsorbed by the ileum into the portal blood, taken up by the liver, and then resecreted into the bile …enterohepatic circulation Bile acid has a hydrophobic surface and a hydrophilic surface The most abundant bile salt in humans – glycocholate: Bile acid micelles Hydrophobic region of the bile salt is oriented from the water molecules x hydrophilic region interacts with water Mixed micelles contain (beside bile acids) phospholipids and cholesterol, or FA and acylglycerols; FA and phospholipids form a bilayer in the interior, bile salts occupy the edge. Released FA and monoacylglycerols are incorporated into bile acids micelles Micelles move lipids from the intestinal lumen to the cell surface where absorption occurs Micelles also serve as transport vehicles for vitamins A, K Fat malabsorption can result from pancreatic failure or lack of bile acids bulk of unabsorbed lipids is excreted with the stool…steatorrhea Fat digestion and absorption Most absorbed lipids are incorporated into chylomicrons Within the intestinal cell (after absorption): FA of medium chain lenght (6-10C) pass into the portal blood without modification long-chain FA (> 12C) are bound to a fatty acid binding protein in the cytoplasm and transported to ER, where they are resynthesized to TG • TG form lipid globules to which phospholipids, cholesterol (esters), and apolipoproteins adsorb – chylomicrons • chylomicrons migrate through the Golgi to the basolateral membrane, they are released, and pass into the lymphatics DIGESTION OF NUCLEIC ACIDS Pancreatic enzymes hydrolyze dietary nucleic acids: ribonucleases deoxyribonucleases endo- as well as exonucleases Polynucleotidases of the small intestine complete the hydrolysis to nucleotides which are then hydrolyzed to nucleosides by phosphatases and nucleotidases Nucleosides are used as such or undergo degradation by nucleosidases / nucleoside phosphorylases to free bases and pentose-1-phosphate Purine nucleosides are: A) catabolized to uric acid B) alternatively, purines are released and used for resynthesis of NA Pyrimidine nucleosides are: A) catabolized to NH4+, CO2, and β-aminoisobutyrate or β-alanine, respectively, that are partially converted to (methyl)malonyl-CoA B) absorbed intact and utilized for the resynthesis of nucleic acids