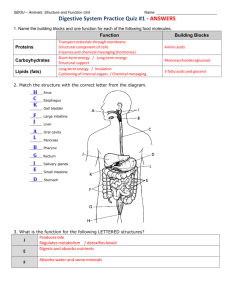
Digestive System
advertisement

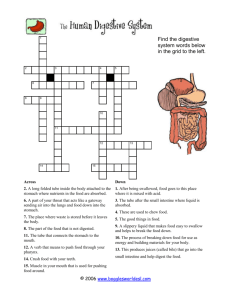
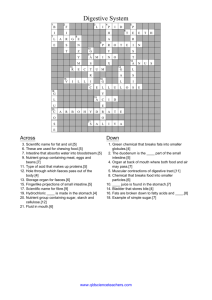
Chapter 24 Digestive System 24-1 I. Introduction: A. Anatomy of the Digestive System • 1. Digestive tract: also called alimentary tract • 2. GI tract: technically refers to stomach and intestines • 3. Accessory organs • 4. Regions – Mouth or oral cavity with salivary glands and tonsils – Pharynx (throat – Esophagus – Stomach – Small intestine (duodenum, ileum, jejunum) – Large intestine including cecum, colon, rectum – anal canal with mucous glands – Anus 24-2 B. Functions of the Digestive System 1. Ingestion: 2. Mastication:. 3. Propulsion – Deglutition: swallowing – Peristalsis: – Mass movements – chyme 24-3 4. Mixing: Segmental contractions • http://www.youtube.com/watch?v=GdNtRomPvs&NR=1 24-4 Functions, cont. 5. Secretion: lubricate, liquefy, digest – – – – Mucus: Water: Bile: Enzymes: 6. Digestion: Mechanical and chemical 7. Absorption: 8. Elimination: 24-5 C. Histology of the Digestive Tract •1. Mucosa •2. Submucosa 24-6 • 3. Muscularis: • 1. circular and longitudinal • 2. smooth except for upper esophagus • 4. Serosa or adventitia: • 1. visceral peritoneum in abdominal cavity • 2. tunica adventitia outside of the abdominal cavity 24-7 D. Nervous regulation of the Digestive System – 1. • • • Local: enteric nervous system Types of neurons: sensory, motor, interneurons Coordinates peristalsis and regulates local reflexes As stomach empties into small intestine, local reflex regulates rate of emptying – 2. General: coordination with the CNS. May initiate reflexes because of sight, smell, or taste of food. Parasympathetic primarily. Sympathetic input inhibits muscle contraction, secretion, and decrease of blood flow to the digestive tract. 24-8 E. Peritoneum – 1. Visceral: – 2. Parietal: – 3. Retroperitoneal: e.g., kidneys, pancreas, duodenum – 4. Mesenteries: – 5. Greater omentum: connects greater curvature of the stomach to the transverse colon. – 6. Lesser omentum: connects lesser curvature of the stomach and the proximal part of the duodenum to the liver and diaphragm – G. Hand in balloon explanation 24-9 Greater omentum 24-10 II. Terms of Oral Cavity – – – – – – – – – – – – – – A. Vestibule: B. Oral cavity proper: C. Frenulum: 1. labial 2. lingual D. Teeth 1. incisors 2. canines 3. premolars 4. molars E. Gingiva F. Hard palate G. Soft palate H. Uvula 24-11 I. Tongue • 1. Muscular – Intrinsic muscles: change shape – Extrinsic muscles: protrude or retract tongue, move side to side • 2. Lingual frenulum • 3. Terminal sulcus: groove divides tongue into anterior 2/3; posterior 1/3 • a. Anterior part: papillae, some of which have taste buds • b. Posterior part: no papillae and a few scattered taste buds. • c. Lymphoid tissue embedded in posterior surface: lingual tonsil • 4. Moves food in mouth, participates in speech and swallowing 24-12 J. Muscles of Mastication • 1. masseter • 2. temporalis • 3. medial and lateral pterygoidsproduce lateral excursion when acting together. • 4. http://www.you tube.com/watch ?v=pV2TRZE7 pJM 24-13 K. Salivary Glands-three pairs – 1. Parotid: largest. – a.Serous. – b. Parotid duct enters the oral cavity adjacent to the 2nd upper molar – 2. Sublingual: smallest. – a.Mixed, but primarily mucous. – b.Each has 10-12 ducts that enter the floor of the oral cavity. – 3. Submandibular: mixed, – a.Posterior half of inferior border of mandible. – b.Duct enters oral cavity on either side of lingual frenulum 24-14 I. Functions of Saliva – 1. Prevents bacterial infection – 2. Lubrication – 3. Contains salivary amylase that breaks down starch into disaccharides – 4. Helps to form bolus for deglutition – 5. Parasympathetic input causes salivary production – 6. Sympathetic stimulation leads to thick mucoid saliva 24-15 III. Pharynx A. Common chamber of respiratory and digestive system B. Regions C. Structures ensuring that food gets to the right place 1. hard palate 2. soft palate and uvula 3. epiglottis 24-16 IV. Esophagus A. 10” long B. Tunical mucosa- Stratified squamous epithelium C. Passes through diaphragm at esophageal hiatusHiatal hernia D. sphinters E. GERD F. Peristalsis of bolus G. http://www.youtube.com/watc h?v=Q-n_Q0qKXzg H. Tunica muscularis-upper third voluntary with lower two thirds visceral I. Swallowing (Deglutition)-three phases – 1. Voluntary: bolus of food moved by tongue from oral cavity to pharynx. – 2. Pharyngeal: reflex. – a. Controlled by swallowing center in medulla oblongata. – b. Soft palate elevates, upper esophageal sphincter relaxes, – c. elevated pharynx opens the esophagus, – d. food pushed into esophagus by pharyngeal constrictors’ successive contraction from superior to inferior. – e. Epiglottis is tipped posteriorly due to pressure of the bolus, – f. larynx elevated to prevent food from passing into larynx. – 3. Esophageal: reflex. Stretching of esophagus causes enteric NS to initiate peristalsis of muscles in the esophagus. 24-18 V. Stomach A. Parts 1. Openings – Gastroesophageal (cardiac): to esophagus – Pyloric: to duodenum 2. Parts – – – – Cardiac Fundus Body Pyloric: antrum and canal – Greater and lesser curvatures: attachment sites for omenta – Sphincters – Pyloric 24-19 B. Histology of the Stomach 1. Layers – a. Serosa or visceral peritoneum – b. Muscularis: three layers • Outer longitudinal • Middle circular • Inner oblique – c. Submucosa – d. Mucosa – e. Rugae: folds in mucosa and submucosa when empty. 24-20 2. Modifications of the tunica mucosa • • a. Gastric pits: openings for gastric glands. Lined with simple columnar epithelium b. Cells of gastric pits – Mucous neck: mucus – Parietal: hydrochloric acid and intrinsic factor (aids in vitamin B12 absorption – Chief: pepsinogen – Endocrine: regulatory hormones • histamine that stimulates acid secretion • Somatostatin that inhibits gastrin and insulin secretion 24-21 3. Secretions of the Stomach • a. Chyme: ingested food plus stomach secretions • b. Mucus: surface and neck mucous cells – Viscous and alkaline – Protects from acidic chyme and enzyme pepsin – Irritation of stomach mucosa causes greater mucus • c. Intrinsic factor: parietal cells. Binds with vitamin B12 and helps it to be absorbed. B12 necessary for DNA synthesis • d. HCl: parietal cells – Kills bacteria – Stops carbohydrate digestion by inactivating salivary amylase – Denatures proteins – Helps convert pepsinogen to pepsin • e. Pepsinogen: packaged in zymogen granules released by exocytosis. Pepsin catalyzes breaking of covalent bonds in proteins 24-22 4. Hydrochloric Acid Production produces alkaline tide in veins draining stomach 24-23 5. Regulation of stomach activity a. Cephalic Phase • • The taste or smell or even thoughts of food stimulate the medulla oblongata. • Parasympathetic action potentials are carried by the vagus nerves to the stomach • Postganglionic neurons stimulate secretion by parietal and chief cells (HCl and pepsin) and stimulate the secretion of the hormone gastrin and histamine. . • Gastrin is carried through the circulation back to the stomach where it and histamine stimulate further secretion of HCl and pepsin 24-24 b. Gastric Phase 24-25 c. Intestinal Phase -Chyme in the duodenum with a pH less than 2 or containing lipids inhibits gastric secretions by three mechanisms -Sensory input to the medulla from the duodenum inhibits the motor input from the medulla to the stomach. Stops secretion of pepsin and HCl. -Local reflexes inhibit gastric secretion-enterogastric reflex -Secretin, and cholecystokinin produced by the duodenum decrease gastric secretions in the stomach. 24-26 6. Movements of the Stomach-reflux mixing • a. Initially both esophageal and pyloric sphincters are closed. • b. A lot like kneading dough • c. Mixture is turned back at the pyloric sphincter and folds over itself • d. Liquefied mixture is called chyme • e. At some point pyloric sphincter opens a little and a bit of acidic chyme squirts through • f. The acidic additions to the small intestine lead to the enterogastric reflex 24-27 7. Rate of stomach emptying • a. Goldilocks and the three bears • b. Regulated by CCK (lipid rich meals) and secretin • c. Carbohydrate meals fastest through-1 hour • d. Fatty meals slowest (5-6 hours) • e. Greater the stretching the more reflux 24-28 VI. Small Intestine • Site of greatest amount of digestion and absorption of nutrients and water • Divisions – Duodenum- first 25 cm beyond the pyloric sphincter. – Jejunum- 2.5 m – Ileum- 3.5 m. Peyer’s patches or lymph nodules 24-29 A. Modifications to Increase Surface Area – 1. Plicae circulares (circular folds) – 2. Villi that contain capillaries and lacteals. Folds of the mucosa – 3. Microvilli: folds of cell membranes of absorptive cells – 4. total surface area about that of a tennis court 24-30 B. Mucosa and Submucosa • 1. Cells and glands of the mucosa – Absorptive cells: cells with microvilli, produce digestive enzymes and absorb digested food – Goblet cells: produce protective mucus – Endocrine cells: produce regulatory hormones – Granular cells (paneth cells): may help protect from bacteria • 2. Intestinal glands (crypts of Lieberkühn): tubular glands in mucosa at bases of villi • 3. Duodenal glands (Brunner’s glands): tubular mucous glands of the submucosa. 24-31 C. Jejunum and Ileum • 1. Gradual decrease in diameter, thickness of intestinal wall, number of circular fold, and number of villi the farther away from the stomach • 2. Peyer’s patches: lymphatic nodules numerous in mucosa and submucosa • 3. Ileocecal junction: where ilium meets large intestine. Ileocecal sphincter and ileocecal valve 24-32 D. Secretions of the Small Intestine • 1. Fluid primarily composed of water, electrolytes and mucus. • 2. Mucus – Protects against digestive enzymes and stomach acids • 3. Digestive enzymes: bound to the membranes of the absorptive cells – Disaccharidases: Break down disaccharides to monosaccharides – Peptidases: Hydrolyze peptide bonds – Nucleases: Break down nucleic acids • 4. Brunner’s glands – Stimulated by vagus nerve, secretin, chemical or tactile irritation of duodenal mucosa 24-33 E. Movement in the Small Intestine • 1. Segmental contractions mix • 2. Peristalsis propels • 3. Ileocecal sphincter remains slightly contracted until peristaltic waves reach it; it relaxes, allowing chyme to move into cecum • 4. Cecal distention causes local reflex and ileocecal valve constricts – Prevents more chyme from entering cecum – Increases digestion and absorption in small intestine by slowing progress of chyme – Prevents backflow 24-34 VII. Liver, Gallbladder, Pancreas and Ducts 24-35 VIII. Histology of the Liver • A. Connective tissue septa branch from the visceral peritoneum into the interior – Divides liver into lobules – Nerves, vessels and ducts follow the septa • B. Lobules: portal triad at each corner – Three vessels: hepatic portal vein, hepatic artery, hepatic duct – Central vein in center of lobule • C. Central veins unite to form hepatic veins that exit liver and empty into inferior vena cava 24-36 • D. Hepatic cords: radiate out from central vein. Composed of hepatocytes • E. Hepatic sinusoids: between cords, lined with endothelial cells and hepatic phagocytic (Kupffer) cells • F. Bile canaliculus: between cells within cords • G. Hepatocyte functions – Bile production – Storage – Interconversion of nutrients – Detoxification – Phagocytosis – Synthesis of blood components 24-37 H. Functions of the Liver • 1. Bile production: 6001000 mL/day. Bile salts (bilirubin), cholesterol, fats, fat-soluble hormones, lecithin – Neutralizes and dilutes stomach acid – Bile salts emulsify fats. Most are reabsorbed in the ileum. – Secretin (from the duodenum) stimulates bile secretions, increasing water and bicarbonate ion content of the bile • 2. Storage – Glycogen, fat, vitamins, copper and iron. Hepatic portal blood comes to liver from small intestine. 24-38 • 3. Nutrient interconversion – Amino acids to energy producing compounds – Hydroxylation of vitamin D. Vitamin D then travels to kidney where it is hydroxylated again into its active form-promotes bone growth and absorption of calcium • 4. Detoxification – Hepatocytes remove ammonia and convert to urea • 5. Phagocytosis – Kupffer cells phagocytize worn-out and dying red and white blood cells, some bacteria • 6. Synthesis – Albumins, fibrinogen, globulins, heparin, clotting factors 24-39 IX. Gallbladder • A. Sac lined with mucosa folded into rugae, inner muscularis, outer serosa • B. Bile arrives constantly from liver is stored and concentrated • C. Stimulated by cholecystokinin (from the intestine) and vagal stimulation • D. Bile exits through cystic duct then into common bile duct • E. Gallstones: precipitated cholesterol – Can block cystic duct – Can occur because of drastic dieting 24-40 Control of Bile Secretion and Release 24-41 X. Pancreas • A. Pancreas both endocrine and exocrine • B. Endocrine: pancreatic islets or Islets of Langerhans. • C. Exocrine: groups acini (grape-like cluster) form lobules separated by septa. • D. Aqueous. Bicarbonate lowers pH inhibiting pepsin and providing proper pH for enzymes • E. Enzymatic portion: – Trypsinogen – Chymotrypsinogen – Procarboxypeptidase – Pancreatic amylase – Pancreatic lipases – Deoxyribonucleases and ribonucleases 24-42 Histology of pancreas 24-43 F. Pancreatic Secretions • 1. Interaction of duodenal and pancreatic enzymes – Enterokinase from the duodenal mucosa and attached to the brush border activates trypsinogen to trypsin. – Trypsin activates chymotrypsinogen to chymotrypsin. – Trypsin activates procarboxypeptidase to carboxypeptidase. • 2. Trypsin, chymotrypsin, and carboxypeptidase digest proteins: proteolytic. • 3. Pancreatic amylase continues digestion of starch. • 4. Pancreatic lipase digests lipids. • 5. Deoxyribonucleases and ribonucleases digest DNA and ribonucleic acid, respectively. 24-44 G. Control of Pancreatic Secretion 24-45 XI. Large Intestine • A. Extends from ileocecal junction to anus • B. Consists of cecum, colon, rectum, anal canal • C. Movements sluggish (18-24 hours); chyme converted to feces. • D. Absorption of water and salts, secretion of mucus, extensive action of microorganisms. • E. 1500 mL chyme enter the cecum, 90% of volume reabsorbed yielding 80-150 mL of feces 24-46 E. Anatomy of the Large Intestine • • 1. Cecum – Blind sac, vermiform appendix attached. 2. Colon – Ascending, transverse, descending, sigmoid – Circular muscle layer complete; longitudinal incomplete (three teniae coli). Contractions of teniae form pouches called haustra. – Mucosa has numerous straight tubular glands called crypts. Goblet cells predominate, but there are also absorptive and granular cells as in the small intestine 24-47 • 3. Rectum – Straight muscular tube, thick muscular tunic • 4. Anal canalsuperior epithelium is simple columnar; inferior epithelium is stratified squamous – Internal anal sphincter (smooth muscle) – External anal sphincter (skeletal muscle) – Hemorrhoids: Vein enlargement or inflammation 24-48 F. Secretions of the Large Intestine • 1. Mucus provides protection – Parasympathetic stimulation increases rate of goblet cell secretion • 2. Bacterial actions produce gases (flatus) from particular kinds of carbohydrates found in legumes and in artificial sugars like sorbitol • 3. Bacteria produce vitamin K which is then absorbed • 4. Feces consists of water, undigested food (cellulose), microorganisms, sloughed-off epithelial cells • 5. Lactose intolerance 24-49 G. Movement in the Large Intestine • 1. Mass movements – Common after meals – Integrated by the enteric plexus • 2. Local reflexes instigated by the presence of food in the stomach and duodenum – Gastrocolic: initiated by stomach – Duodenocolic: initiated by duodenum • 3. Defecation – Defecation reflex: distension of the rectal wall by feces – Parasympathetic stimulation – Usually accompanied by voluntary movements to expel feces. Abdominal cavity pressure caused by inspiration and by contraction of muscles of abdominal wall. 24-50 Movement in the Large Intestine 24-51 XII. Digestion and absorption A. Carbohydrates 1. 2. 3. 4. 5. Monosaccharide vs. disaccharide vs. polysaccharide Carbohydrate digestion begins in the mouthsalivary amylase Nothing occurs in the stomach as salivary amylase is denatured Pancreatic amylase takes the carbo to the disaccharide level Epithelium of the small intestine produces disaccharidases 24-52 B. Protein digestion • 1. amino acid vs. protein • 2. initial breakdown begins in stomach with pepsin • 3. continues in intestine with trypsin, chymotrypsin, and carboxypeptidase • 4. dipeptides are broken down by peptidases from epithelial cells of the mucosa 24-53 C. Lipid digestion • 1. categories of lipids • a. phospholipids • b. Triglycerides • c. Cholesterol • 2. diverse group but all are hydrophobic • 3. digestion commences in the small intestine with pancreatic lipase and bile salts 24-54 4. Transport of Lipids Across Intestinal Epithelium 24-55 5. Transport of Lipids in blood stream • All lipids carried in the blood are done so in combination with protein to make them soluble in plasma. • Cholesterol: 15% ingested; 85% manufactured in liver and intestinal mucosa • Lipids are lower density than water; proteins are higher density than water • Chylomicrons: 99% lipid and 1% protein (extremely low density); enter lymph • VLDL: 92% lipid, 8% protein – Form in which lipids leave the liver – Triglycerides removed from VLDL and stored in adipose cells. VLDL has been converted to LDL. • LDL: 75% lipid, 25% protein – Transports cholesterol to cells – Cells have LDL receptors – # of LDL receptors become less once cell’s lipid/cholesterol needs are met. • HDL: 55% lipid, 45% protein – Transports excess cholesterol from cells to liver 24-56 Water and Ions • Water: can move in either direction across wall of small intestine depending on osmotic gradients • Ions: sodium, potassium, calcium, magnesium, phosphate are actively transported 24-57