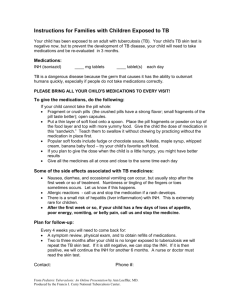
Antitubercular Drugs Nursing Implications
advertisement

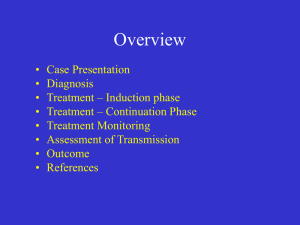
Respiratory System Drugs Antitubercular Drugs Antitubercular Drugs • Tuberculosis (TB) • Caused by Mycobacterium tuberculosis • Antitubercular drugs treat all forms of Mycobacterium Antitubercular Drugs Mycobacterium Infections Common infection sites • • • • • Lung (primary site) Brain Bone Liver Kidney • Aerobic bacillus • Passed from infected: – Humans – Cows (bovine) and birds (avian) • Much less common Antitubercular Drugs Mycobacterium Infections • Tubercle bacilli are conveyed by droplets • Droplets are expelled by coughing or sneezing, then gain entry into the body by inhalation • Tubercle bacilli then spread to other body organs via blood and lymphatic systems • Tubercle bacilli may become dormant, or walled off by calcified or fibrous tissue Antitubercular Drugs Tuberculosis - Pathophysiology • M. tuberculosis – gram-positive, acid-fast bacillus • Spread from person to person via airborne droplets – Coughing, sneezing, speaking – disperse organism and can be inhaled – Not highly infectious – requires close, frequent, and prolonged exposure – Cannot be spread by hands, books, glasses, dishes, or other fomites Antitubercular Drugs Tuberculosis – Clinical Manifestations • Early stages – free of symptoms – Many cases are found incidentally • Systemic manifestations: – Fatigue, malaise, anorexia, weight loss, low-grade fevers, night sweats – Weight loss – occurs late – Characteristic cough – frequent & produces mucoid or mucopurulent sputum – Dull or tight chest pain • Some cases: acute high fever, chills, general flulike symptoms, pleuritic pain, productive cough • HIV Pt with TB: Fever, cough, weight loss – – Pneumocystic carinii pneumonia (PCP) Antitubercular Drugs Tuberculosis – Diagnostic Studies • Tuberculin Skin Testing -- + reaction 2-12 weeks after the initial infection – PPD – Purified protein derivative – used to detect delayed hypersensitivity response • Two-step testing – health care workers • 5mm > induration – Immunosuppressed patients • 10 mm> “at risk” populations & health are workers • 15 mm> Low risk people – Chest X-ray -- used in conjunction with skin testing • Multinodular lymph node involvement with cavitation in the upper lobes of the lungs • Calcification – within several years after infection – Bacteriologic Studies – • Sputum, gastric washings –early morning specimens for acid-fast bacillus -- three consecutive cultures on different days • CSF or pus from an abscess Antitubercular Drugs Tuberculosis – Medical Management • May be treated as outpatient – Depends on debility and severity of symptoms • Mainstay of treatment: drug therapy for active disease: – Five primary drugs: • Isoniazid (INH) * (primary drug used) • Rifampin • Pyrazinamide • Streptomycin • Ethambutol – Combination 4 drug therapy – HIV patients cannot take rifampin – interferes with antiretroviral drug effectiveness Antitubercular Drugs Second-Line Drugs capreomycin cycloserine ethionamide kanamycin para-aminosalicyclic amikacin levofloxacin ofloxacin acid (PAS) Antitubercular Drug Therapy Considerations • Perform drug-susceptibility testing on the first Mycobacterium sp. that is isolated from a patient specimen to prevent the development of MDR-TB(Multidrug-resistant TB) • Even before the results of susceptibility tests are known, begin a regimen with multiple antitubercular drugs • Adjust drug regimen once the results of susceptibility testing are known • Monitor patient compliance closely during therapy • Problems with successful therapy – patient nonadherence to drug therapy – increased incidence of drug-resistant Antitubercular Therapy Effectiveness depends upon: • • • • • Type of infection Adequate dosing Sufficient duration of treatment Drug compliance Selection of an effective drug combination Antitubercular Therapy Problems • Drug-resistant organisms • Drug toxicity • Patient noncompliance • Multidrug-resistant TB (MDR-TB) Antitubercular Drugs Isoniazid (INH) • Drug of choice for TB • Resistant strains of Mycobacterium emerging • Metabolized in the liver through acetylation—watch for “slow acetylators” • Used alone or in combination with other drugs • Used for the prophylaxis or treatment of TB Antitubercular Drugs Adverse Effects • INH – Peripheral neuritis, hepatotoxicity • Ethambutol – Retrobulbar neuritis, blindness • Rifampin – Hepatitis, discoloration of urine, stools Antitubercular Drugs Nursing Implications • Thorough medical history and physical assessment • Perform liver function studies in patients who are to receive isoniazid or rifampin (especially in elderly patients or those who use alcohol daily) • Assess for contraindications to the various drugs, conditions for cautious use, and potential drug interactions Antitubercular Drugs Nursing Implications Monitor for therapeutic effects • Decrease in symptoms of TB, such as cough and fever • C&S and CXR should confirm clinical findings • Observe for lack of clinical response to therapy, indicating possible drug resistance Monitor for adverse effects • Instruct patients on the adverse effects that should be reported to the physician immediately – fatigue, nausea, vomiting, numbness and tingling of the extremities, fever, loss of appetite, depression, jaundice Antitubercular Drugs Patient Education Patient education is critical • Therapy may last for up to 24 months • Take medications exactly as ordered, the same time every day • Emphasize the importance of strict adherence to regimen for improvement of condition or cure • Remind patients that they are contagious during the initial period of their illness—instruct in proper hygiene and prevention of the spread of infected droplets • Emphasize to patients to take care of themselves, including adequate nutrition and rest Antitubercular Drugs Patient Education • Patients should not consume alcohol or take other medications, including OTC -- check with their physician • INH and rifampin cause oral contraceptives to become ineffective; another form of birth control will be needed • Patients who are taking rifampin should be told that their urine, stool, saliva, sputum, sweat, or tears may become reddish orange; even contact lenses may be stained • Pyridoxine (Vitamin B6) may be needed to combat neurologic adverse effects associated with INH therapy • Oral preparations may be given with meals to reduce GI upset, even though recommendations are to take them 1 hour before or 2 hours after meals