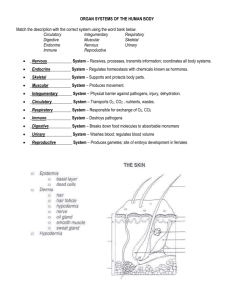
THE SKIN
advertisement

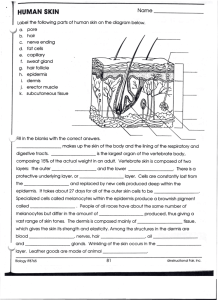
THE INTEGUMENTARY SYSTEM • Complex set of organs that includes the skin and its derivatives (sweat and oil glands, hairs, and nails) – Includes: – Nerves – Blood vessels – Muscles • Major function: protection THE SKIN • Also called the integument, which simply means: covering • Epidermis: – The epidermis is a keratinized stratified squamous epithelium (epi=upon) – Outer most protective shield of the body • Dermis: – Underlying epidermis – Makes up bulk of skin – Composed of: • Fibrous connective tissue • Blood vessels: – Nutrients reach the epidermis by diffusion SKIN THE SKIN • Hypodermis: also called superficial fascia – Subcutaneous tissue: • – – – Deep to the skin Not really part of the skin but it shares some of the skin’s protective functions Superficial to the tough connective tissue wrapping (fascia) of the skeletal muscles Consists mostly of adipose tissue: • Stores fat: – – – – Shock absorber insulation Anchors the skin to the underlying structures (muscles) Thickens as one gains weight: • • • Thighs Breast Beer belly SKIN Epidermis • A keratinized stratified squamous epithelium consisting of four distinct cell types and four or five distinct layers: – Stratum Corneum – Stratum Lucidum (thick skin) – Stratum Granulosum – Stratum Spinosum – Stratum Basale Cells of the Epidermis • Include: – – – – Keratinocytes Melanocytes Merkel cells Langerhan’s cells EPIDERMIS Cells of the Epidermis Keratinocytes • • • Produce keratin – Fibrous protein that helps give the epidermis its protective properties Tightly connected to one another by desmosomes (cell junction composed of thickened plasma membranes joined by filaments) Arise in the deepest part of the epidermis from a layer of cells (stratum basale) that undergo almost continuous mitosis – Cells pushed upward by the production of new cells beneath them – By the time they reach the free surface of the skin, they are dead, scalelike structures that are little more than keratin-filled plasma membranes – Millions rub off everyday giving us a totally new epidermis every 25 to 45 days • Friction rubs them off (hands, etc) – Persistent friction causes a thickening of the epidermis called a callus EPIDERMIS Cells of the Epidermis Melanocytes • • • Spider shaped cells Found in the deepest layer of the epidermis Synthesize the pigment melanin (melan=black) – Made and accumulated in membrane-bound granules (small. grainlike mass) called melanosomes • Moved along actin filaments by motor proteins to the ends of the melanocyte’s processes (spider arms) – From here they are taken up by the keratinocytes – Accumulate on the superficial (sunny side) of the keratinocyte nucleus, forming a pigment shield that protects the nucleus from the damaging effects of ultraviolet (UV) radiation in sunlight EPIDERMIS Cells of the Epidermis Langerhan’s Cells • Star-shaped • Arise from bone marrow and migrate to the epidermis • Also called epidermal dendritic cells • Are macrophages (WBC) that help activate our immune system – Their slender processes extend among the surrounding keratinocytes, forming a more or less continuous network EPIDERMIS Cells of the Epidermis Merkel Cells • Present at the epidermal-dermal junction • Saped like a spiky hemisphere • Intimately associated with a disclike sensory nerve ending: – This combination is called a Merkel disc – Functions as a sensory receptor for touch EPIDERMIS Layers of the Epidermis • Variation in epidermal thickness determines if skin is thick or thin • Thick skin covers: palms, fingertips, and soles of the feet – Five layers: strata (bed sheets) • Deep to superficial: – – – – – Stratum basale Stratum spinosum Stratum granulosum Stratum lucidum Stratum corneum • Thin skin covers the rest of the body – Stratum lucidum is absent and the other layers are thinner EPIDERMIS Layers of the Epidermis Stratum Basale • Deepest epidermal layer • Attached to the underlying dermis along a wavy borderline • Consists (mostly) of a single row of cells representing the youngest keratinocytes • Many mitotic nuclei – Reflects rapid cell division • Alternate name: stratum germinativum EPIDERMIS Layers of the Epidermis Stratum Spinosum • • • Spinosum (prickly) Several cell layers thick Cells contain a weblike system of intermediate filaments, which span their cytosol to attach to desmosomes – • Keratinocytes appear irregular (spiny) in shape, causing them to be called prickle cells – – • These intermediate filaments consist mainly of tension-resisting bundles of prekeratin filaments Spines do not exist in the living cells They arise during tissue preparation when these cells shrink but their numerous desmosomes hold tight Scattered among the keratinocytes are: – – Melanin granules Langerhan’s cells (highest concentration) EPIDERMIS Layers of the Epidermis Stratum Granulosum • • Consist of 3-5 layers in which keratinocyte appearance changes drastically – Cells flatten – Nuclei and organelles begin to disintegrate – They accumulate: • Keratohyaline granules: – Help to form keratin in the upper layers • Lamellated granules: – Contain a waterproofing glycolipid that is spewed into the extracellular space and is a major factor in slowing water loss across the epidermis – Cell membranes thicken • Lipids coat the external membrane Above this layer the epidermal cells are too far from the dermal capillaries, so they die EPIDERMIS Layers of the Epidermis Stratum Lucidum • Thin translucent band • Few rows of clear, flat, dead keratinocytes with indistinct boundaries • Gummy substance of the keratohyaline granules clings to the keratin filaments in the cells, causing them to aggregate in parallel arrays (regular arrangement) • Visible ONLY in THICK SKIN EPIDERMIS Layers of the Epidermis Stratum Corneum • Horny (hard, callous) layer • 23-30 cell layers thick (3/4 of epidermis) • Keratin and the thickened plasma membranes of cells protect the skin against abrasion and penetration • Glycolipid between cells waterproofs this layer • The stratum corneum (horny layer) is the outermost protective layer of the epidermis composed of a thick layer of dead keratinocytes EPIDERMIS SKIN EPIDERMIS Dermis • • Composed of strong, flexible connective tissue Its cells are typical of those found in any connective tissue proper: – – – – – Fibroblasts: cells that form the fibers of connective tissue Macrophages: protective cell capable of phagocytosis Mast cells: immune cell that initiates inflammation White blood cells: protection Its semifluid matrix is heavily embedded with: • Collagen: strong, fibrous (threadlike) insoluble protein • Elastin: extracellular connective tissue protein • Reticular fibers: supporting framework tissue • The dermis binds the entire body together like a body stocking – It is your hide and corresponds exactly to animal hides used to make leather products • • Richly supplied with nerve fibers, blood vessels, and lymphatic vessels Major portions of hair follicles, as well as oil and sweat glands, are derived from epidermal tissue but reside in the dermis Dermis Two Layers • 1.The thin, superficial papillary layer is highly vascularized areolar connective tissue containing a woven mat of collagen and elastin fibers – Its superior surface is thrown into peglike projections called dermal papillae (papill=nipple) that indent the overlaying epidermis • Many contain: – Capillary loops – Meissner’s corpuscles: touch receptors – Pain receptors SKIN Dermis Two Layers • On the palms of the hands and soles of the feet, these papillae lie atop larger mounds called dermal ridges – Which in turn cause the overlying epidermis to form epidermal ridges that increase friction and enhance the gripping ability of the fingers and feet • Epidermal ridge patterns are genetically determined and unique to each of us • Because sweat pores open along their crest, our fingerprints leave identifying films of sweat called fingerprints on almost anything they touch SKIN Dermis Two Layers • Three types of skin markings: – Finger prints – Cleavage lines – Flexure lines Dermis Two Layers • 2.The reticular layer: – Deeper – Account for 80% of the thickness of the dermis – Extracellular matrix contains thick bundles of interlacing fibers that run in various planes • Most run parallel to the skin surface • Less dense regions, between these bundles form cleavage, or tension lines: – Important to a surgeon: » Incision made parallel to these lines, the skin gapes less and heals more readily than when the incision is made across cleavage lines – Collagen fibers give skin strength and resiliency • Binds water, helping keep the skin hydrated – Elastin fibers provide the stretch-recoil properties of skin SKIN Dermis Two Layers • Flexure lines: – Dermal folds that occur at or near joints, where the dermis is tightly secured to deeper structures (notice the deep creases on your palms) • Since the skin cannot slide easily to accommodate joint movement in such regions, the dermis folds and deep skin creases form – Visible on wrists, fingers, soles, and toes HOMEOSTATIC IMBALANCE • Dermal tearing: – Stretching of the skin during pregnancy – Stretch marks • Blister: – Separation of the epidermal and dermal layers by a fluid-filled pocket Skin Color • Determined by three pigments: – Melanin – Hemoglobin – Carotene Melanin • Only pigment made in the skin • Polymer of tyrosine amino acid • Ranges in color from yellow to reddishbrown to black • Synthesis depends on an enzyme in melaocytes called tyrosinase • Passes from melanocytes to the basal keratinocytes Melanin • All humans have the same relative number of melanocytes – Individual and racial differences in skin coloring reflect the relative kind and amount of melanin made and retained – Melanocytes of black and brown skinned people produce many and darker melanosomes than those of fair-skinned individuals, and their keratinocytes retain it longer • Freckles and pigmented moles are local accumulations of melanin Melanin • Melanocytes are stimulated by sunlight – Causes substantial melanin buildup, which helps protect the DNA of viable skin cells from UV radiation by absorbing the light and dissipating the energy as heat HOMEOSTATIC IMBALANCE • Excessive sunlight damages the skin: – Clumping of elastin fibers: results in leathery skin – Depresses the immune system – Alters DNA Carotene • Yellow to orange pigment found in certain plant products such as carrots • Tends to accumulate in the stratum corneum and in the tissue of the hypodermis • Color most obvious in the palms and soles, where the stratum corneum is thickest (example: the skin of the heel) • Most intense when large amounts of carotenerich foods are eaten Hemoglobin • Pinkish hue of fair skin people Skin Color Variations • Redness: erythema – – – – – Embarrassment Fever Hypertension Inflammation Allergy • Pallor: blanching – – – – – Fear Anger Emotional stress Anemia Low blood pressure • Jaundice: yellow cast – Liver disorder (yellow bile pigment accumulates in the blood and deposited in body tissues) • Bile normally secreted in the bile pigments (bilirubin) as part of bile • Bronzing: – Metallic appearance of skin – Addison’s disease – Hyperfunction of adrenal cortex • Black and blue: bruises – Blood escaping from the blood vessels and clotting under the skin APPENDAGES OF THE SKIN • Derivatives of the epidermis: – Sweat Glands – Sebaceous Glands – Nails – Hair – Hair Follicles Sweat (Sudoriferous) Glands • Distributed over the entire skin surface except the nipples and parts of the external genitalia • Two types of sweat glands: – Eccrine – Apocrine Sweat (Sudoriferous) Glands Eccrine Sweat Glands • (b):Eccrine sweat glands, or merocrine sweat glands, produce true sweat, are the most numerous of the sweat glands, and are particularly abundant on the palms of the hands, soles of the feet, and forehead CUTANEOUS GLANDS CUTANEOUS GLANDS Sweat (Sudoriferous) Glands Eccrine Sweat Glands • Also called merocrine sweat glands • Abundant on the palms, soles of feet, and forehead • Simple, coiled, tubular gland Secretory part lies coiled in the dermis: – The duct extends to open in a funnel-shaped pore at the skin surface • Secretion commonly called sweat is a: – Hypotonic filtrate (lower osmotic pressure than a reference) of the blood that passes through the secretary cells of the sweat glands and is released by exocytosis – 99% water, with some salts (mostly sodium chloride) – Vitamin C – Antibodies – Dermicidin: microbe-killing peptide – Traces of metabolic waste ( urea, uric acid, ammonia) – Lactic acid: chemical that attracts mosquitoes – pH between 4-6 Sweat (Sudoriferous) Glands Eccrine Sweat Glands • Sweating is regulated by the sympathetic nervous system – Major role is to prevent overheating of the body • Heat-induced sweating begins on the forehead and then spreads inferiorly over the remainder of the body • Emotionally induced sweating—so-called “cold sweat” brought on by fright, embarrassment, or nervousness— begins on the palms, soles, and axillae (armpits) and then spreads to other body areas Sweat (Sudoriferous) Glands Apocrine Sweat Glands • Largely confined to the axillary and anogenital areas • Larger than eccrine glands • Ducts empty into hair follicles • Secretion contains the same basic components as true sweat, plus fatty substances and proteins – Quite viscous and milky or yellowish color – Odorless: • BUT, when its organic molecules are decomposed by bacteria on the skin, it takes on a musky and generally unpleasant odor (BODY ODOR) Sweat (Sudoriferous) Glands Apocrine Sweat Glands • Little role in thermoregulation • Role not completely understood – BUT, they are activated by sympathetic nerve fibers during pain and stress • Because their activity is increased by sexual foreplay, and they enlarge and recede with the phases of a women’s menstrual cycle, they may be analogous to the sexual scent glands of other animals Sweat (Sudoriferous) Glands Ceruminous Glands • Modified apocrine glands found in the lining of the external ear canal – Secrete a sticky, bitter substance called cerumen, or earwax • Thought to deter insects and block entry of foreign material Sweat (Sudoriferous) Glands Mammary Glands • Variety of modified sweat glands in the breasts that secrete milk Sebaceous (Oil) Glands • Sebaceous glands are simple alveolar glands (c) found all over the body except the palms of the hands and soles of the feet EXOCRINE GLANDS Sebaceous (Oil) Glands • Secrete sebum, an oily secretion: – The central cells of the alveoli accumulate oily lipids until they become so engorged that they burst, so functionally these glands are holocrine glands • The entire secretory cell ruptures, releasing secretions and dead cell fragments • Secreting their product into a hair follicle or to a pore on the surface of the skin – Sebum softens and lubricates the hair and skin, prevents hair from becoming brittle, and slows water loss from the skin when the external humidity is low – Bactericidal action (bacteriumkilling) Holocrine Gland Sebaceous (Oil) Glands (a) • Secretion is stimulated by hormones, especially androgens CUTANEOUS GLANDS Sebaceous (Oil) Gland HOMEOSTATIC IMBALANCE • If a sebaceous gland duct is blocked by accumulated sebum, a whitehead appears on the skin surface – If the material oxidizes and dries, it darkens to form a blackhead • Acne is an active inflammation of the sebaceous glands accompanied by “pimples” (pustules or cysts) on the skin – Usually caused by bacterial infection, particularly by staphylococcus • Seborrhea: cradle cap in infants – Caused by overactive sebaceous glands – Raised lesions that gradually become yellow to brown and begin to slough off oily scales Nails • • • • A nail is a scalelike modification of the epidermis that forms a clear, protective covering on the dorsal surface of the distal part of a finger or toe Nails are made up of hard keratin Each nail has a free edge, a body (visible attached portion), and a proximal root (embedded in the skin) The deeper layers of the epidermis extend beneath the nail as the nail bed – – Corresponds to the superficial keratinized layers The thicker proximal portion of the nail bed, called the nail matrix, is responsible for nail growth NAIL Nails • Nails normally appear pink because of the rich bed of capillaries in the underlying dermis – Region that lies over the thick nail matrix appears as a white crescent called the lunula (little moon) • Proximal and lateral borders of the nail are overlapped by skin folds, called nail folds – Proximal nail fold projects onto the nail body as the cuticle (eponychium=on the nail) – Region beneath the free edge of the nail where dirt and debris tend to accumulate is the hyponychium (below nail), informally called the quick Structure of a Hair • Hairs, or pili, are flexible strands produced by hair follicles that consist largely of dead, keratinized cells – The hard keratin that dominates hairs and nails has two advantages over the soft keratin found in typical epidermal cells: • 1. It is tougher and more durable • 2. Its individual cells do not flake off Structure of a Hair • The main regions of a hair are the shaft, which projects from the skin, and the root, the part embedded in the skin HAIR SHAFT HAIR Structure of a Hair • If the shaft is flat and ribbonlike in cross section, the hair is kinky • If the shaft is oval in cross section, the hair is silky and wavy • If the shaft is perfectly round in cross section, the hair is straight and tends to be coarse Structure of a Hair • A hair has three layers of keratinized cells: – Inner core (central core) is the medulla • Consist of large cells and air spaces • Absent in fine hair – Middle layer is the cortex • Bulky layer surrounding the medulla, consists of several layers of flattened cells – Outer layer is the cuticle HAIR Structure of a Hair Cuticle • • • • Formed from a single layer of cells that overlap one another from below like shingles on a roof This arrangement helps to keep neighboring hairs apart so that the hair does not mat – Hair conditioners smooth out the rough surface of the cuticle and make our hair look shiny The most heavily keratinized part of the hair, the cuticle, provides strength and helps keep the inner layers tightly compacted It is subjected to the most abrasion, the cuticle tends to wear away at the tip of the hair shaft, allowing the keratin fibrils in the cortex and medulla to frizz out, creating “split ends” HAIR SHAFT Structure of a Hair • Hair pigments (melanin of different colors) are made by melanocytes at the base of the hair follicle and transferred to the cortical cells • Various proportions of melanins of different colors (yellow, rust, brown, and black) combine to produce hair color from blond to pitch black – Red hair is colored by the iron-containing pigment called trichosiderin – Gray or white hair results from decreased melanin production (mediated by delayed-action genes) and from the replacement of melanin by air bubbles in the hair shaft (AIRHEAD-JOKE) Structure of a Hair Follicle • Hair follicles fold down from the epidermis into the dermis and occasionally into the hypodermis • The deep end of a hair follicle is expanded, forming a hair bulb, which is surrounded by a knot of sensory nerve endings called a hair follicle receptor, or root hair plexus, wraps around each hair bulb, and bending the hair stimulates these endings – Consequently, our hairs act as sensitive touch receptors HAIR FOLLICLE SKIN Structure of a Hair Follicle • Hair papilla, a nipplelike bit of dermal tissue, protrudes into the hair bulb – Contains a knot of capillaries that supplies nutrients to the growing hair and signals it to grow • The wall of a hair follicle is composed of: – Outer connective tissue root sheath, derived from the dermis, – A thickened basement membrane called a glassy membrane, – An inner epithelial root sheath, derived mainly from an invagination of the epidermis HAIR FOLLICLE SKIN Structure of a Hair Follicle • Hair matrix: actively dividing area of the hair bulb that produces the hair • Associated with each hair follicle is a bundle of smooth muscle cells called an arrector pili muscle – Most hair follicles approach the skin surface at a slight angle – Arrector muscles are attached in such a way that their contraction pulls the hair follicle into an upright position and dimples the skin surface to produce goose bumps SKIN Types and Growth of Hair • Hairs come in various sizes and shapes, but can be classified as: – Vellus: vell=wool, fleece • Pale, fine body hair variety of children and adult females – Terminal: • • • • Darker Coarser, longer hair of eyebrows and scalp Axillary and pubic Face and chest of males • Hair growth and density are influenced by many factors, such as nutrition and hormones Types and Growth of Hair • The rate of hair growth varies from one body region to another and with sex and age – Averages 2.5 mm per week • Life span of hairs varies and appears to be under control of a slew of proteins • Each follicle has a growth cycle where it is active and inactive for a period of time – Inactive, hair matrix cells die and the follicle base and hair bulb shrivel – Follicle then enters a resting stage for a period of time – After the resting phase, the matrix proliferates again and forms a new hair to replace the old one that has fallen out or will be pushed out by the new hair – Only a small percentage of the hair follicles are shed at any one time, we lose an average of 90 scalp hairs daily – Follicles of the eyebrow hairs remain active for only 3-4 months, which explains why your eyebrows are never as long as the hairs on your head HOMEOSTATIC IMBALANCE • In women, small amounts of androgens are normally produced by both the ovaries and the adrenal glands – Excessive hairiness (hirsutism: hirsut=hairy) – Signs of masculinization • Large amounts of androgens can be secreted by ovarian tumors resulting in: • Beard and hairy chest – Tumors can be surgically removed Hair Thinning and Baldness • A follicle has only a limited number of cycles in it – Ideal conditions, hair grows faster from the teen years to the 40s; then its growth slows • The fact that hairs are not replaced as fast as they are shed leads to hair thinning and some degree of baldness (alopecia), in both sexes – Begins at the anterior hairline and progresses posteriorly – Coarse terminal hairs are replaced by vellus hairs, and the hair becomes increasingly wispy • Male pattern baldness, which is a type of true, or frank, balding, is a genetically determined, sex-influenced condition FUNCTIONS OF THE INTEGUMENTARY SYSTEM • Protection – 1.Chemical barriers include skin secretions and melanin: • Although the skin’s surface teems with bacteria, the low pH of skin secretions (acid mantle) retards their multiplication – Many bacteria are killed by bactericidal substances in sebum • Natural antibiotic (human defensin) kills bacteria • Chemical pigment (melanin) prevents UV damage FUNCTIONS OF THE INTEGUMENTARY SYSTEM • 2.Physical or mechanical barriers are provided by the continuity of the skin, and the hardness of the keratinized cells – Waterproofing glycolipids block diffusion of water and water soluble substances between cells (preventing both loss and entry) • Lipid soluble substances DO penetrate: – – – – – Oxygen, carbon dioxide Fat-soluble vitamins (A, D, E, K) Steriods Oleoresins (plants: poison ivy and oak) Organic solvents (acetone, dry cleaning fluids, paint thinner) » Causes kidney shut down and brain damage – Salts of heavy metals (lead, mercury, nickel) » Results in anemia and neurological defects – Drug agents (penetration enhancers) that help ferry other drugs into the body FUNCTIONS OF THE INTEGUMENTARY SYSTEM • 3.Biological barriers include: – Langerhans’ cells of the epidermis • Active elements of the immune system • Respond to antigens – Macrophages of the dermis • Dispose of viruses and bacteria that have managed to penetrate the epidermis – DNA itself • Absorb UV radiation and transfer it to the atomic nuclei, which heat up and vibrate vigorously – Heat dissipates to surrounding water molecules instantaneously, the DNA converts potentially destructive radiation into harmless heat Body Temperature Regulation • The skin plays an important role in body temperature regulation by: – Using the sweat glands of the skin to cool the body: • Evaporation of sweat from the skin surface dissipates body heat and efficiently cools the body, thus preventing overheating – Constriction of dermal capillaries to prevent heat loss: • When the external environment is cold, dermal blood vessels constrict causing the warm blood to bypass the skin temporarily and allows the skin temperature to drop to that of the external environment – Passive heat loss from the body is slowed, thus conserving body heat Cutaneous Sensation • Made possible by the placement of cutaneous sensory receptors, which are part of the nervous system, in the layers of the skin • Cutaneous receptors are classified as exteroceptors because they respond to stimuli arising outside the body: – Example: • Meissner’s corpuscles (in dermal papillae) and Merkel dics allow us to become aware of a caress or the feel of our clothing against our skin • Pacinian receptors (in deepest dermis and hypodermis) alert us to bumps or contacts involving deep pressure • Hair follicle receptors sense wind blowing through our hair and a playful tug on a pigtail • Bare nerve endings that meander throughout the skin sense painful stimuli ( irritating chemical, extreme heat or cold, etc.) Metabolic Functions • When sunlight bombards the skin, modified cholesterol molecules circulating through dermal blood vessels are converted to a vitamin D precursor, and transported via the blood to other body areas to play various roles in calcium metabolism – Example: calcium cannot be absorbed from the digestive tract without vitamin D • Makes chemical conversions that supplement those of the liver: – Examples: keratinocyte enzymes can: • 1. Disarm many cancer-causing chemicals that penetrate the epidermis • 2. Convert some harmless chemicals into carcinogens • 3. Activate some steroid hormones: – Transform cortisone applied to the skin into hydrocortisone, a potent antiinflammatory drug • Make several biologically important proteins, including collagenase, an enzyme that aids the natural turnover of collagen (deters wrinkles) Blood Reservoir • Dermal vascular supply is extensive: – The skin may act as a blood reservoir by holding up to 5% of the body’s blood supply, which may be diverted to other areas of the body should the need arise • When other body organs, such as vigorously working muscles, need a greater blood supply, the nervous system constricts the dermal blood vessels shunting more blood into the general circulation, making it available to the muscles and other body organs Excretion • Limited amounts of nitrogenous containing wastes (ammonia, urea, and uric acid) are eliminated from the body in sweat, although most nitrogenous wastes are excreted in urine • Profuse sweating is an important avenue for water and salt (sodium chloride) loss Skin Cancer • Most tumors that arise in the skin are benign and do not spread (metastasize) to other body areas – Example: • A wart: a neoplasm (abnormal growth of tissue that serves no purpose but grows at the expense of healthy tissue) caused by a virus • Some tumors are malignant, or cancerous, and invade other body areas • A crucial risk factor for the nonmelanoma skin cancers is overexposure to the UV radiation in sunlight, which appears to disable a tumor suppressor gene – However, frequent irritation of the skin by infections, chemicals, or physical trauma seems to be a predisposing factor Skin Cancer • Sunburned skin accelerates its production of Fas, a protein that causes genetically damaged skin cells to commit suicide, thus decreasing the risk of mutations that will cause sun-linked skin cancer – It is the death of these gene-damaged cells that causes the skin to peel after a sunburn – NEW lotions are being produced that will fix damaged DNA before the involved cells can develop into cancer cells • These lotions contain tiny oily vesicles (liposomes) filled with enzymes that initiate repair of the DNA mutations most commonly caused by sunlight Skin Cancer • • • • • • (a):Basal cell carcinoma is the least malignant and the most common skin cancer Stratum basale cells proliferate, invading the dermis and hypodermis Cancer lesions occur most often on sun-exposed areas of the face and appear as shiny, domeshaped nodules that later develop a central ulcer with a pearly, beaded edge Relatively slow growing Metastasis seldom occurs before it is noticed Full cure by surgical excision is the rule in 99% of cases SKIN CANCER Skin Cancer • (b):Squamous cell carcinoma tends to grow rapidly and metastasize if not removed • Arises from the keratinocytes of the stratum spinosum • Lesion appears as a scaly reddened papule (small, rounded elevation) that arises most often on the head (scalp, ears, and lower lip), and hands • If it is caught early and removed surgically or by radiation therapy, chance of complete cure is good SKIN CANCER Skin Cancer • • • (c):Melanoma is the most dangerous of the skin cancers because it is highly metastatic and resistant to chemotherapy Cancer of the melanocytes Begin wherever there is pigment: – – – • Most appear spontaneously About 1/3 develop from preexisting moles Usually appears as a spreading brown to black patch that metastasizes rapidly to surrounding lymph and blood vessels Key to surviving is early detection – – Chance of survival is poor if the lesion is over 4mm thick Therapy is wide surgical excision accompanied by immunotherapy SKIN CANCER Skin Cancer • American Cancer Society suggests you regularly examine your skin for new moles or pigmented spots and apply the ABCDE rule for recognizing melanoma: – A. Asymmetry: • The two sides of the pigmented spot or mole do not match – B. Border irregularity: • The borders of the lesion exhibit indentations – C. Color: • The pigmented spot contains several colors (blacks, browns, tans, and sometimes blues and reds) – D. Diameter: • The spot is larger than 6 mm in diameter (the size of a pencil eraser) – E. Elevation: • Elevation above the skin Burns • A burn is tissue damage inflicted by intense heat, electricity, radiation, or certain chemicals, all of which denature cell proteins and cause cell death to infected areas • The most immediate threat to a burn patient is dehydration and electrolyte imbalance due to fluid loss – Leads to renal shutdown and circulatory shock (inadequate blood circulation due to reduced blood volume) – To save the patient, the lost fluids must be replaced immediately Burns • The volume of fluid lost can be estimated by computing the percentage of body surface burned (extent of the burns) using the rule of nines (ONLY APPROXIMATE) – This method divides the body into 11 areas, each accounting for 9% of total body area, plus an additional area surrounding the genitals accounting for 1% of body surface BURNS Burns • Burn patients also need thousands of extra food calories daily to replace lost proteins and allow tissue repair: – No one can eat this much, so burn patients are given supplementary nutrients through gastric tubes and intravenous (IV) lines • After the first 24 hours has passed, the threat to a burn patient becomes infection to the wound site: – Burned skin is sterile for the first 24 hours – Thereafter, bacteria, fungi, and other pathogens easily invade areas where the skin barrier is destroyed, and they multiply rapidly in the nutrient-rich environment of dead tissues – Adding to this problem is the fact that the immune system becomes deficient one to two days after severe burn injury Burns • Burns are classified according to their severity – First-degree burns involve damage only to the epidermis • Tend to heal in two to three days without special attention • Sunburn is usually a first-degree burn – Second-degree burns injure the epidermis and the upper region of the dermis • Blisters appear • Skin regeneration occurs with little or no scarring within three to four weeks if care is taken to prevent infection – Third-degree burns involve the entire thickness of the skin • Burned area appears gray-white, cherry red, or blackened, and initially there is little or no edema (excessive tissue fluid-swelling) • Since the nerve endings in the area have been destroyed, the burned area is not painful • Skin grafting is usually necessary • Excessive scar tissue usually forms Burns • Burns are considered critical if any of the following conditions exists: – 1. Over 25% of the body has second-degree burns – 2. Over 10% of the body has third degree burns – 3. There are third-degree burns of the face, hands, or feet • Facial burns introduce the possibility of burned respiratory passageways, which can swell and cause suffocation • Burns at joints are also troublesome because scar tissue formation can severely limit joint mobility BURNS ROSACEA WINESTAIN TATTO DEVELOPMENTAL ASPECTS OF THE INTEGUMENTARY SYSTEM • The epidermis develops from the embryonic ectoderm, and the dermis and the hypodermis develop from the mesoderm • By the end of the fourth month of development the skin is fairly well formed • During infancy and childhood, the skin thickens and more subcutaneous fat is deposited • During adolescence, the skin and hair become oilier as sebaceous glands are activated • The skin reaches its optimal appearance when we reach our 20s and 30s; after that time the skin starts to show the effects of cumulative environmental exposures • As old age approaches, the rate of epidermal cell replacement slows and the skin thins, becoming more prone to bruising and other types of injuries