General Principles of Pathophysiology
advertisement

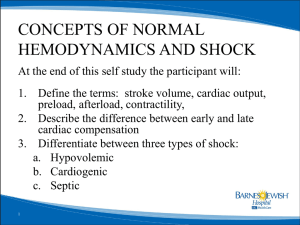
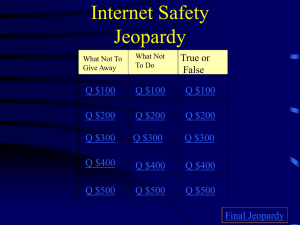
General Principles of Pathophysiology Energy Metabolism Perfusion Shock Topics Define shock in terms of cellular function Review the requirements for adequate cellular perfusion (Fick principle) Review the mechanisms for starling’s law Preload vs. afterload Muscle contraction Topics Continued Discuss the mechanisms for oxygen transport oxyhemoglobin dissociation curve Define the stages of shock Describe different causes of shock Define multiple organ dysfunction syndrome Shock Defined Inadequate tissue perfusion Anaerobic metabolism Final Common Pathway! Aerobic Metabolism 6 CO2 6 O2 METABOLISM GLUCOSE 6 H2O 36 ATP HEAT (417 kcal) Anaerobic Metabolism 2 LACTIC ACID GLUCOSE METABOLISM 2 ATP HEAT (32 kcal) Anaerobic? So What? Inadequate Cellular Oxygenation Inadequate Energy Production Metabolic Failure Anaerobic Metabolism Lactic Acid Production Cell Death! Metabolic Acidosis Homeostasis is maintenance of balance Requires proper functioning systems Cardiovascular Respiratory Renal Physiology of Perfusion Dependant on 3 components of circulatory system Pump Fluid Container Factors Affecting The Pump Preload Contractile force Frank-starling mechanism Afterload Muscle Anatomy Contraction: Sliding Filaments image from: http://www.accessexcellence.com/AB/GG/muscle_Contract.html What Is Blood Pressure? BP = Cardiac Output X Systemic Vascular Resistance CO = Stroke Volume X Heart Rate What Affects Blood Pressure? ANS balance Contractility Preload Starling’s law Afterload Autonomic Nervous System Review… Quiz Time! Yeah! Jeopardy Controls vegetative functions,exits the CNS at high in the neck and low in the back. What is the parasympathetic nervous system? Jeopardy The chief neurotransmitter of the sympathetic nervous system. What is Norepinephrine? Jeopardy The ‘cutesy’ name for the parasympathetic nervous system. What is ‘Feed or Breed’? Jeopardy Two types of parasympathetic receptors. What is nicotinic (NMJ) and muscarinic (organs)? Jeopardy Two types classes of sympathetic receptors. What is alpha and beta? Jeopardy The ‘cutesy name’ for the sympathetic nervous system. What is ‘fight or flight’? Jeopardy Stimulation of this receptor causes an increase in peripheral vasoconstriction. What is alpha 1? Jeopardy Stimulation of this receptor causes an increase in myocardial contractility. What is beta 1? Jeopardy Stimulation of this receptor causes an increase in bronchodilation. What is beta 2? Jeopardy Stimulation of this receptor causes a decrease in the sympathetic activation. What is alpha 2? Jeopardy Two types of parasympathetic receptors. What is nicotinic (NMJ) and muscarinic (organs). Changes in Afterload and Preload Peripheral vasoconstriction… peripheral vascular resistance… afterload… blood pressure. Changes in Afterload and Preload Peripheral vasodilation… peripheral vascular resistance… afterload… blood pressure. Changes in Afterload and Preload fluid volume… preload… contractility (Starling’s Law)… blood pressure. cardiac output. Changes in Afterload and Preload fluid volume… preload… contractility (Starling’s Law)… blood pressure. cardiac output. Fluid Must have adequate amounts of hemoglobin Must have adequate intravascular volume Maintenance of Fluid Volume Renin-Angiotensin-Aldosterone system. Works through kidneys to regulate balance of Na+ and water. Renin-Angiotensin-Aldosterone Plasma volume Detected by &/Or Kidney (juxtaglomerular apparatus) [Na+] Via ACE (Angiotensin Converting Enzyme) Releases Renin Converts Angiotensin II… Angiotensin I… Angiotensinogen Renin-Angiotensin-Aldosterone vasoconstriction PVR Angiotensin II… thirst ADH (anti-diuretic hormone) Adrenal cortex Fluid volume Releases Aldosterone BP! Na+ reabsorption Hemostasis The stoppage of bleeding. Three methods Vascular constriction Platelet plug formation Coagulation Coagulation Formation of blood clots Prothrombin activator Prothrombin thrombin Fibrinogen fibrin Clot retraction Fibrinolysis Plasminogen Tissue plasminogen activator (tPA) Plasmin Disseminated Intravascular Coagulation “A systemic thrombohemorrhagic disorder … with evidence of: 1) Procoagulant activation 2) Fibrinolytic activation 3) Inhibitor consumption 4) End-organ failure” Bick, R.L. Seminars in Thrombosis and Hemostasis 1996 Pathophysiology of DIC Uncontrolled acceleration of clotting cascade Small vessel occlusion Organ necrosis Depletion of clotting factors Activation of fibrinolysis Ultimately severe systematic hemorrhage Container Vasculature is continuous, closed and pressurized system Microcirculation responds to local tissue needs Blood flow dependent on PVR Fick Principle Effective movement and utilization of O2 dependent on: Adequate fio2 Appropriate O2 diffusion into bloodstream Adequate number of RBCs Proper tissue perfusion Efficient hemoglobin ‘loading’ Fick Principle Perfusion = Arterial O2 Content Venous O2 Content Affected by: Hemoglobin levels circulation of RBCs distance between alveoli and capillaries pH and temperature Onloading Oxygen in Lungs oxyhemeglobin pH 7.45 Remember: CO2 [H+] pH 7.4 • pH shifts curve to left • ‘onloading’ in lungs deoxyhemeglobin Pressure Offloading Oxygen in Tissues pH 7.4 Remember: CO2 [H+] oxyhemeglobin pH 7.35 •pH shifts curve to right • ‘offloading’ to tissues deoxyhemeglobin Pressure Causes of Inadequate Perfusion Inadequate pump Inadequate preload Poor contractility Excessive afterload Inadequate heart rate Inadequate fluid volume Hypovolemia Inadequate container Excessive dilation Inadequate systematic vascular resistance Responses to Shock Normal compensation includes: Progressive vasoconstriction Increased blood flow to major organs Increased cardiac output Increased respiratory rate and volume Decreased urine output Cellular Response to Shock O2 use Anaerobic metabolism ATP synthesis Na+ Pump Function Tissue perfusion Stimulation of clotting cascade & inflammatory response Intracellular Na+ & water Impaired cellular metabolism Impaired glucose usage Cellular edema Vascular volume Stages of Shock Compensated Uncompensated Irreversible Compensated Shock Defense mechanisms are successful in maintaining perfusion Presentation Tachycardia Decreased skin perfusion Altered mental status Uncompenstated Shock Defense mechanisms begin to fail Presentation Hypotension Prolonged Cap refill Marked increase in heart rate Rapid, thready pulse Agitation, restlessness, confusion Irreversible Shock Complete failure of compensatory mechanisms Death even in presence of resuscitation Types of Shock Hypovolemic Cardiogenic Neurogenic Anaphylactic Septic Hypovolemic Shock “Fluid failure” Decreased intravascular volume Causes? “Third spacing” Cardiogenic Shock R.A.S. Activation Volume/ Preload Impaired myocardial function Catecholamine Release CO Myocardial O2 demand Dyspnea SVR O2 supply Peripheral & pulmonary edema Neurogenic Shock Sympathetic Tone Or Parasympathetic Tone Tissue perfusion Cardiac Output Vascular Tone Massive Vasodilation SVR & Preload Anaphylactic Shock “Container failure” Massive & systemic allergic reaction Large release of histamine Increases membrane permeability & vasodilation Septic Shock “Container failure” Systemic infection Multiple Organ Dysfunction System Progressive dysfunction of two or more organ systems Caused by uncontrolled inflammatory response to injury or illness Typically sepsis References New York Presbyterian hospital hypertension center: Http://pc101186.Med.Cornell.edu/htchome/htbk/Htbkindex.ht m Biographics Gallery: http://www.accessexcellence.com/AB/GG/#AnchorBuilding-11481 RAS (Renin-Angiotensin-Aldosterone System): http://www.science.mcmaster.ca/Biology/4S03/RAS.HTM A graduate student’s hypertension page: http://www.teachingbiomed.man.ac.uk/student_projects/2000/mnpm6ven/default.h tm