Shock - Yale medStation
advertisement

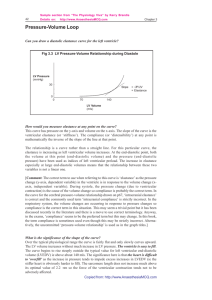
Shock Stephanie N. Sudikoff, MD Pediatric Critical Care Yale School of Medicine Learning Objectives • Understand the pathophysiology of shock • Understand the principles of treatment of shock • Examine septic shock as one example “The reason you get up in the morning is to deliver oxygen to the cells.” Mark Mercurio, MD Demand Supply Oxygen Consumption vs. Delivery • Oxygen consumption (DEMAND) – VO2 = CO x (CaO2-CvO2) • Oxygen delivery (SUPPLY) – DO2 = CO x CaO2 DO2 CO Preload CaO2 SV HR Myocardial contractility Afterload Hb content and affinity What are PRELOAD and AFTERLOAD? Preload • PreloadLV = (EDPLV)(EDrLV)/2tLV where, LV = left ventricle ED = end diastole • Represents all the factors that contribute to passive ventricular wall stress at the end of diastole Venous return and CO Factors affecting venous return 1. Decrease in intravascular volume 2. Increase in venous capacitance 3. Increase in right atrial pressure 4. Increase in venous resistance Afterload • AfterloadLV = (SPLV)(SrLV)/2tLV where, LV = left ventricle S = systole • Represents all the factors that contribute to total myocardial wall stress during systolic ejection Myocardial contractility Myocardial contractility Positive Negative Inotropic Agents Inotropic Agents 1. Adrenergic agonists 2. Cardiac glycosides 3. High extracellular [Ca++] 1. Ca++-channel blockers 2. Low extracellular [Ca++] Heart rate • HR CO • At high HR, diastolic filling is impaired • Atrial contraction accounts for up to 30% of Stroke Volume SHOCK Demand Supply Shock Classification of Shock Decreased preload (hypovolemic) Hemorrhage Dehydration Cardiac tamponade Pneumothorax Decreased myocardial contractility (cardiogenic) Myocarditis Cardiopulmonary bypass Congestive heart failure Myocardial infarction Drug intoxication Sepsis Heart rate abnormalities (cardiogenic) Dysrhythmias Increased afterload (obstructive) Massive pulmonary embolus Critical aortic and pulmonic stenosis Decreased afterload (distributive) Anaphylaxis Neurogenic shock Sepsis Abnormalities in Hb affinity (dissociative) Methemoglobinemia Carbon monoxide poisoning Systemic response to low perfusion Systemic response to low perfusion • Increase CO – Increase preload • Aldosterone • Na reabsorption • Interstitial fluid reabsorption • ADH secretion • Venoconstriction Systemic response to low perfusion • Increase CO – Increase contractility • Sympathetics – Increase afterload • Vasoconstriction – Increase HR • Sympathetics Systemic response to low perfusion • Increase CO – Increase contractility • Sympathetics – Increase HR • Sympathetics • Increase SVR – Vasoconstriction – Increase blood volume Local response to low perfusion • Increase O2ER – Opening of previously closed capillaries – Increased surface area for diffusion – Shortened diffusion distance – Increased transit time Physical Signs of low CO Organ System ↓ Cardiac Output ↓↓ Cardiac Output (Compensated) ↓↓ Cardiac Output (Uncompensated) CNS — Restless, apathetic Agitated-confused, stuporous Respiration — ↑ Ventilation ↑↑ Ventilation Metabolism — Compensated Uncomensated metabolic acidemia metabolic acidemia Gut — ↓ Motility Ileus Kidney ↑ Specific gravity, ↓ volume Oliguria Oliguria-anuria Skin Delayed capillary refill Cool extremities Mottled, cyanotic, cold extremities CVS ↑ Heart rate ↑↑ Heart rate, ↓ peripheral pulses ↑↑ Heart rate, ↓ blood pressure, central pulses only Objective monitors • Systemic perfusion – base deficit – lactate Objective monitors • Systemic perfusion – ABG – lactate • CO – PA catheter – Arterio-venous oxygen difference • Preload – CVP – Echo • Myocardial contractility – Echo • Afterload – PA catheter – Invasive or noninvasive BP • HR – EKG • CaO2 – Hb – ABG TREATMENT OF SHOCK Goals of therapy ↓ Demand ↑ Supply O2 consumption O2 delivery • Treat underlying cause Reduction of demands for CO • Treat hyperthermia aggressively Reduction of demands for CO • Treat hyperthermia • Reduce work of breathing – As much as 20% of CO goes to respiratory muscles PPV and CO Advantages • Decreases work of breathing • Improves acidosis • Decreases PVR • Decreases LV afterload • Improves oxygenation Reduction of demands for CO • Treat hyperthermia • Reduce work of breathing • Sedation • Seizure control • Paralysis DO2 CO Preload CaO2 SV HR Myocardial contractility Afterload Hb content and affinity Increase supply: Restoration of perfusion • Preload – Fluid resuscitation – Colloids vs. crystalloids Increase supply: Restoration of perfusion • Preload – Fluid resuscitation – Colloids vs. crystalloids • Myocardial contractility – Inotropic support – ECMO – Other mechanical support Increase supply: Restoration of perfusion • Preload – Fluid resuscitation – Colloids vs. crystalloids • Myocardial contractility – Inotropic support – ECMO – Other mechanical support • Afterload – Vasopressors – Vasodilators Increase supply: Restoration of perfusion • Preload • HR – Fluid resuscitation – Anti-arrhythmics – Colloids vs. crystalloids – Pacer • Myocardial contractility – Inotropic support – ECMO – Other mechanical support • Afterload – Vasopressors – Vasodilators Increase supply: Restoration of perfusion • Preload • HR – Fluid resuscitation – Anti-arrhythmics – Colloids vs. crystalloids – Pacer • Myocardial contractility – Inotropic support – ECMO – Other mechanical support • Afterload – Vasopressors – Vasodilators – Beta-blockers? • CaO2 – Blood transfusion – Oxygen support SEPTIC SHOCK Types of septic shock • Cold shock – ↓ CO, ↑ SVR (60% pediatric) – Narrow pulse pressure, thready pulses, delayed capillary refill Phases of septic shock • Warm shock (“early”) – ↑ CO, ↓ SVR – ↓ CO, ↓ SVR – Wide pulse pressure, bounding pulses, brisk capillary refill • Cold shock (“late”) – ↓ CO, ↑ SVR – Narrow pulse pressure, weak pulses, delayed capillary refill Early recognition! Early recognition! Increase preload • Aggressive fluid resuscitation Increase preload • Aggressive fluid resuscitation • Usually requires 40-60 mL/kg but can be as much as 200 mL/kg • 20 mL/kg IV push titrated to clinical monitors Monitor improvement in CO • Cardiac output – – – – – Heart rate Urine output Capillary refill Level of consciousness Blood pressure NOT reliable endpoint Increase preload • Aggressive fluid resuscitation with crystalloids or colloids • Usually requires 40-60 mL/kg but can be as much as 200 mL/kg • 20 mL/kg IV push titrated to clinical monitors • Maintain hemoglobin within normal for age (≥10 g/dL) Antibiotic therapy • IV antibiotics within 1 hr of recognition of severe sepsis • Cultures before antibiotics • Cover appropriate pathogens • Penetrate presumed source of infection Improve myocardial contractility and titrate afterload Cold Shock, Adequate BP: Decrease afterload Adequacy of resuscitation • • • • • • • • • Capillary refill < 2 sec Adequate pulses Warm limbs Normal mental status Urine output > 1 mL/kg/hr Adequate blood pressure Improved base deficit Decreased lactate ScvO2 > 70% Early shock reversal improves outcome † † † † Carcillo JA et al. Pediatrics 2009;124:500-508 SUMMARY Demand Supply Shock Goals of therapy ↓ Demand ↑ Supply O2 consumption O2 delivery • Treat underlying cause DO2 CO Preload CaO2 SV HR Myocardial contractility Afterload Hb content and affinity Special thanks to Vince Faustino, MD for use of his slides