The Digestive System - mustafaaltinisik.org.uk
advertisement

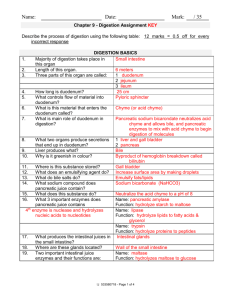
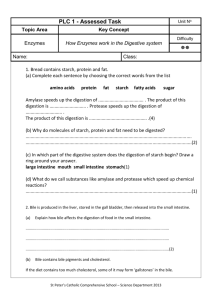
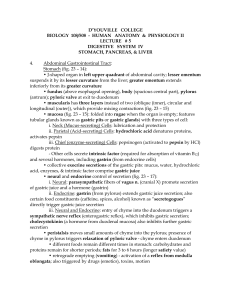
The Digestive System • Mechanism for nourishing the body • Most nutrients in food require either degradation or release prior to absorption • Digestion occurs in GI Tract • Digestion – Mechanical • chewing and peristalsis – Chemical • enzymes, HCl Overview of GI Tract • Upper GI Tract – Mouth and pharnyx provide entryway – Lead to Esophagus • Esophagus wall consists of same layers found in remainder of GI tract – epithelium (mucosa), submucosa, muscularis mucosa, circular and longitudinal muscles – Secretory glands found throughout GI except colon • Exocrine glands and Endocrine glands Upper GI Tract Continued • Sphincters – circular muscles located throughout digestive tract • Lower Esophageal Sphincter – allows passage of food into stomach • Pyloric Sphincter – Controls release of chyme from stomach to duodenum • Stomach – J shaped organ – volume ranges from 50 to 1500 mL (2 -52 oz) Lower GI tract and Accessory Organs • Small Intestine – duodenum, jejunum and ileum – main site for nutrient digestion and absorption – duodenum receives secretions from liver, gallbladder and pancreas • Liver – hepatocytes make bile from cholesterol – right and left hepatic bile ducts join to form common hepatic duct Lower GI tract and Accessory Organs • Gallbladder – capacity to hold 40-50 mL of bile – functions to concentrate and store bile • Pancreas – 2 types of active tissue • Acini or ducted exocrine tissue – produces digestive enzymes • secreted into small ducts within pancreas which leads to common hepatic bile duct • empties into duodenum • Ductless endocrine tissue – secretes hormones, glucagon and insulin Structure of SI • Epithelial surface (mucosa) structured to maximize surface area – Large folds of mucosa (folds of Kerckring) – Villi • projections lined with 100s of absorptive cells • contain blood capillaries and central lacteal – Microvilla • • • • extensions of plasma membrane of absorptive cells possess surface coat of glycocalyx forms brush border most digestive enzymes produced by SI found here. Structure of SI • Crypts of Lieberkuhn – pits located between villi – epithelial cells in these crypt migrate upward and out of crypts toward tips of villi – turnover every 3-5 days – Cells include • paneth cells secrete proteins with unknown function • globlet cells secrete mucus • Enterochromaffin cells with endocrine functions Structure of SI • Lymphoid Tissues – mucosa and submucosa – Peyer’s Patches • T-lymphocytes and B-lymphocytes • provide defense against bacteria and foreign bodies • Ileocecal valve – allows unabsorbed materials to leave ileum and enter cecum Colon • Cecum • Ascending, transverse and descending sections • Sigmoid sections • Haustra or pouches – created by contraction of 1 or 3 muscular strips (tenaie coli) along with contraction of circular muscles • Absorbs water and lytes Regulation Of Digestive Process • Regulatory Peptides (GI hormones and neuropeptides) – Gastrin (hormone) • produced mainly by gastric cells • released upon entry of food into stomach – stimulates HCl release – gastric and intestinal motility – pepsinogen release – Cholecystokinin (CCK, hormone) • produced by SI cells • released upon entry of chyme into stomach – amino acids, fat • targets pancreas and gallbladder Regulatory Peptides • Secretin – produced by cells of SI – secreted in response to chyme (acid) into duodenum – targets pancreas – may inhibit GI motility • Gastric Inhibitory Polypeptide (GIP) – produced by SI cells – Inhibits gastric secretions and motility – Simulates intestinal and insulin secretions Regulatory Peptides • Somatostatin – Produced by pancreatic and SI cells – Paracrine • released by endocrine cells but diffuse through extracellular space to target tissue – Enters gastric juice – Inhibits gastrin secretion, as well as GIP and secretin – Inhibits gastric acid release, gastric motility, pancreatic exocrine secretions and gall bladder secretions Neural Regulation • Enteric Nervous System – – – – located in wall of GI tract begins in esophagus and ends at anus controls peristaltic activity affected by parasympathetic and sympathetic nervous systems • Acetylcholine increase GI motility • Norepinephrine and epinephrine inhibit GI activity – Also influences GI secretions Neurocrines (Regulatory Peptides) • Neurocrines – Peptides originating from nerves of gut • Vasoactive Intestinal Peptide (VIP) – stimulates intestinal secretions – relaxes GI sphincters – inhibits gastric acid secretion – stimulates bicarbonate release • Gastrin Releasing Peptide (GRP) – Stimulates release of HCl, gastrin and CCK • Neurotensin (Bombesin) – Mediates gastric emptying, gastric acid secretion and SI motility Process of Digestion • Oral Cavity and Salivary Glands – mastication of food – mixed with salivary gland secretions • parotid glands – water, lytes and enzymes • submandibular and sublingual glands – water, lytes, enzymes and mucus – Enzymes • alpha amylase and lingual lipase Process of Digestion • Esophagus – Entry of food results in peristalsis • acetylcholine – LES • LES pressure decreases upon swallowing • Neural and hormonal regulation • functions to prevent gastric reflux Process of Digestion • Stomach – Body extends from LES to angular notch • includes fundus • serves as reservoir as well as producer of gastric juice – Antrum (Pyloric Portion) • extends from angular notch to duodenum • grinds and mixes food with digestive juice (chyme) • provides strong peristalsis Stomach • Gastric Juices – produced by 3 different gastric glands • Cardiac glands (fundus) – mucus cells (HCO3 and mucus) and endocrine cells – no parietal (oxyntic cells) • Parietal glands (body) – mucus cells, oxyntic cells (secrete HCl and IF), chief cells secrete pepsinogen upon stimulation by acetylcholine • Pyloric glands (antrum) – both mucus and oxyntic cells – endocrine G cells that produce gastrin – Acetylcholine stimulates chief, oxyntic and other gastric cells Gastric Juices • HCl – activates inactive zymogen pepsinogen to active pepsin – denatures proteins – serves as bactericide • Mucus – lubricates and protects gastric lining • Intrinsic Factor (IF) – necessary for vitamin B12 absorption HCl • Release from oxyntic cells stimulated by – acetylcholine, gastrin, CCK, histamine – Histamine • secreted from mast cells • paracrine that binds to H2 receptors on parietal cells to stimulate HCl release • mechanism used in drug therapy to lower acid – drugs prevent histamine from binding to H2 receptors – decreases acid release Gastric Emptying • GI hormones and neuropeptides affect a pacemaker – determines frequency and rate of contractions – 1-5 mL chyme allowed to enter duodenum every 30 seconds – Fat appears to slow gastric emptying • Inhibitors – Secretin, GIP, Somatostatin, CCK Small Intestine • Chyme has low pH – SI protected by pancreatic secretions and secretions from Brunner’s glands – Secretin and CCK • Digestive juices – Glands within crypts of Lieberkuhn – Pancreas • Responsible for enzymes that digest 50% CHO, 50% protein, 90% lipids Digestive Juice • Pancreatic Proteases – trypsinogen, chymotrypsinogen, procarboxypeptidases, proelastase, collagenase – secreted in vesicles – must be activated • trypinsogen converted to trypsin by enteropeptidase (enterokinase) and by free trypsin – hydrolyze peptide bonds either internally or from ends – mono, di and some tri can be absorbed • Brush border aminopeptidases to hydrolyze further Digestive Juice • CHO – Pancreatic alpha amylase • hydrolyzes alpha 1-4 bonds – Alpha dextrinase to hydrolyze 1-6 branches – Brush border enzymes (maltase, sucrase, lactase) • Lipids – Pancreatic lipase hydrolyzes TG to yield MG, FFA and glycerol Bile Synthesis • Made in liver cells from cholesterol – cholesterol oxidized • chenodeoxycholic acid and cholic acid – conjugated to glycine or taurine • glycocholic acid and taurocholic acid – conjugation of bile acids with amino acids improves its ability to form micelles – cholesterol and PLs secreted into bile • bile acid dependent frx – Water, Lytes and bilirubin secreted in bile Bile Storage • Gallbladder – Concentrates bile by removing 90% of water – Stores bile – Stimulated to release bile by CCK • CCK secreted in response to amino acids and lipids – Bile is secreted into duodenum Function of Bile • Digestion – Bile acids are amphipathic – Decrease surface tension of fat – Permits emulsification of fat • Increases exposure of area of lipids – Allow digestive enzymes (lipase) to get close to fat • Absorption – Micelle Formation Micelles • Bile acid monomers from simple micelles – Hydrophobic centers, hydrophilic periphery • Fatty acids and MAGs enter micelles – Mixed Micelles • Micelles travel to brush border – MAGs and fatty acids diffuse through unstirred water layer and into enterocytes – Bile acids released for reuse Enterohepatic Circulation • > 90% of bile acids secreted in duodenum are reabsorbed into ileum • Enters portal vein for transport via blood back to liver • Reabsorbed bile acids are secreted in bile along with newly made bile acids • New bile mixed with recirculated bile is sent via cystic duct for storage in gallbladder • Pool of bile (2-4 g) may recycle 1-2 times/meal Secondary Bile Acids • Bile acids not reabsorbed in ileum may be deconjugated by bacteria in colon – deconjugated bile acids form secondary bile acids • cholic acid is converted to deoxycholic acid which may be reabsorbed • chenodeoxycholic acid is converted to lithocholic acid which is excreted in feces – ~ 0.5 g of bile salts are lost in feces daily Decreasing Blood Cholesterol • Only route of cholesterol excretion is in feces • By increasing excretion of bile in feces, one can lower blood cholesterol levels – necessitates use of body cholesterol for synthesis of new bile acids – drugs (powdered resins) bind bile and enhance excretion from body – soluble fiber behaves like resins Role of Intestinal Brush Border in Digestion • CHO Digestion – Isomaltase • 1-6 bonds in oligosaccharides and dextrins – Sucrase • alpha 1-4 bonds in sucrose and maltose – Glucoamylase, glucosidase, maltase • alpha 1-4 bonds in oligosaccharides, maltotriose and maltose – Maltase, Lactase and Sucrase Role of Intestinal Brush Border in Digestion • Protein Digestion – Aminopeptidases hydrolyze N terminal amino acids from oligopeptides, tripeptides and dipeptides – Tripeptidases – Dipeptidases Absorption • Begins in duodenum • Continues throughout jejunum and ileum • May be accomplished by – simple diffusion – facilitated diffusion – active transport – pinocytosis or endocytosis – paracellular absorption • Mechanism depends on – nutrient solubility; electrical gradient; size Colon • Greater absorption of sodium, chloride and water • Secretion of bicarbonate into colon – neutralize acids produced by colonic anaerobic bacteria via action on CHO – also synthesize vitamin K, biotin and folate • Acids produced in colon include short chain fatty acids – acetate, butyrate, propionate – may be absorbed by colonocyte • Progressive dehydration of unabsorbed materials – 1 L of chyme reduced to < 200 mL of defecated