Teams - Chinook Primary Care Network
advertisement
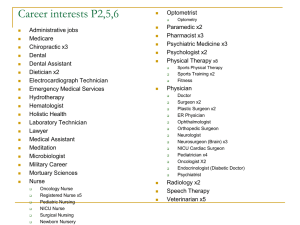
Teams Operational, Clinical, and Teamwork Overview Mike Davies, MD FACP Mark Murray and Associates Burning Questions • How many support staff are needed in our practice? – How many will improve production? – How many will improve outcomes? – How many do other practices have? • If we decide to hire, what professional types of person is best? – RN/LPN/MA/Other? – Social worker, case manager, other? • Other burning questions? Related Questions • What is our current team number and composition? • Are we clear about our mission and goals? • Are we working together as smoothly and efficiently as we could? • Are we providing the right care for our patients? • Is working with this team any fun? • Do we get the job done well? Let’s get to the burning questions.. • What kind? (Who ARE support staff?) • How many? • • • • US Government (excellent data) US Military (excellent data) US Private Practice (survey data – fair data) US HMO (excellent data) Who are Support Staff? • • • • • Medical Clerks RN’s LPN’s Medical Assistants Health Technicians • Pharmacists (including PharmD’s)? • Case Managers? • Social Workers? • Billing • Others? What are Support Staff Duties? • Check in/out patients & Schedule • Example Nursing Duties – VS; Prevention & Chronic Disease screening, information, care – Nursing evaluations; injections; office procedures • Independent Follow-up clinics – BP; DM; Cholesterol; Anticoagulation • Telephone calls Are These Support Staff Duties? • • • • Phlebotomy Billing (and other business office functions) Support for specialty or mental health clinics Other professionals not working directly with providers – i.e. dieticians, social workers • Pharmacy prescription filling duties Team Composition and Number Large Govt. Healthcare US • Adult Primary Care Tending toward Geriatric Practice • 1100 Sites of Care • ~4300 Providers – 2864 MD – 1393 Non-MD Providers (NP, PA) • ~8,200 Support Staff FTEE • Pro-Rated to time spent in clinic managing the panel of assigned patients Bottom Line Average US Govt. Healthcare RN/Provider 0.6 LPN/Provider 0.5 Clerk/Provider 0.6 MA/Provider 0.2 Pharm/Provider 0.15 Support/Provider 2.1 US Military • US Military Primary Care = 2.7-2.8 support staff/provider FTEE – 0.5 RN – 1.8 LPN – 0.5 Clerk FTEE MGMA Safety Net Provider** RN LVN MA Med. Receptioinist Case Manager 1 0.51 0.63 0.53 0.85 1** 0.3 0 1 1 0 Clinical Support 1.67 Staff/FTEE Pro. Medical Record 0.4 Gen. Admin 0.25 2.52/Provider FTEE 0.3 1.6 0.3 0.17 2.6/Provider FTEE MGMA Specialty RN LPN NA Clerk Total Ratio Multi-Specialty 0.4 0.6 0.9 0.4 2.3 Medicine Single Specialty 0.6 0.5 0.9 0.4 2.4 Surgery Single Specialty 0.4 0.6 0.9 0.4 2.3 Cardiology 0.4 0.4 0.6 0.6 2 OB/GYN 0.5 0.9 0.9 0.7 3 0 0 1 0.2 1.2 Psychiatry HMO Team Composition FTEE 6 2.5 11.5 3 0.5 1.0 1.0 0.5 Team Role Physician Nurse Practitioner Medical Assistant/Support Staff RN/Extended Role LVN Exempt Manager Behavior Health Med Specialist Health Educator Physical Therapist 2.8/FTEE Overall Team Composition and Number Summary • Large Govt. US = 2.1 staff/PCP – (RN, LPN, Clerk, Pharmacist) • MGMA = 2.52 – (RN, LVN, MA, Receptionist) • Safety Net = 2.6 – (RN, MA, Receptionist, Case Mgr.) • US Military = 2.7-2.8 – (RN, LPN, Clerk) • US HMO = 2.8 staff/PCP – (RN, LVN, MA) Productivity What Is the Right Number? # On Team Advanced Access Support Staff per Provider 3.18 baseline 2.69 Nov 1998 Jan 2000 Wisconsin F.P. Group Who? RN Team Member Fee for Service Capitated Workload (Burnout) Doc Visit # Less Less Less Less Intensity of Doc Less Visit Net Revenue Less (Unless replaced) Clinical Care Better Less More Better LPN Team Member Fee for Service Capitated Workload (Burnout) Doc Visit # Less Less No Change No Change Intensity of Visit Same or Less Same or Less Net Revenue Same Clinical Care Better Same or Slightly more Better RN/LPN Comparison RN Fee for Service Capitated LVN Fee for Service Capitated Workload (Burnout) Less Less Workload (Burnout) Less Less Doc Visit # Less Less Doc Visit # No Change No Change Intensity of Doc Visit Less Less Intensity of Visit Same or Less Same or Less Net Revenue Less (Unless replaced) More Net Revenue Same Same or Slightly more Clinical Care Better Better Clinical Care Better Better Why Choose RN Based Team? • If you are: – Thinking of moving to Alternative Pay – Have so much work you can’t possibly do it – Want to improve clinical care Now let’s step back…. What is the big picture here? What is a Care Team? An integrated group of professional and clerical staff whose processes and skills enable them to care for the needs of a patient population over time. What is a Care Team? • Cares for a defined population of patients • Measures process and outcomes for feedforward and feedback • Matches the activities to customer demand (uses the data to improve individual and population care) Batalden, Nelson, et al. Continually improving the health and value of health care for a population of patients; the panel management process. Quality Management in Health Care, 1997, 5 (3). 41-51 Total number of patients Provider initiated returns (Internal Demand) Patient Demographics Top 10 Diagnosis Daily walk-ins (External Demand) Pt. Psychosocial and Cultural needs Population Seasonal Variation High Utilizers Daily Phone Calls Self Care Rx refill habits Team (2.5X FTEE) Reception Nurse Provider Capacity Demand Panel Size 2000 66 have Diabetes 360 Patients are Over 65 Team (2.5x FTEE) 113 have Asthma 60 Patients had more than 10 Office Visits Last Year Reception Nurse Provider 248 have Arthritis 130 are Clinically Depressed 228 have Hypertension 160 have Heart Disease 39% of Capacity is Physician Time 39% of Capacity is MA Time 22% of Capacity is RN Time Basic Team Duties • Clinical – WHAT to do – What are the main population needs? – What protocols and guidelines do we need? – What is the work? • Operational – HOW to do it. – Process mapping and redesign – Space/staff use and redesign – Who will do the work? • How “good” is the overall teamwork? – Putting it all together Operational and Clinical Teams Clinical Teams: What to do? Far from agreement on WHAT to do (what prevention and chronic disease guidelines to implement) XX Far from agreement on HOW to do it (how to implement guidelines, how to support provider’s efficiency) Close to Agreement Operational Teams: How to do it? XX Operational Teams This is about efficiency, reliability, and safety Flow Through the Office Check-in to Nurse Dr. in to Dr. out Nurse to Room Check-out to leave Synchronization Point System How Processes Support Flow 1 1 1 1 Process Process Process Process Check-in to Nurse Dr. in to Dr. out Check-out to leave Nurse to Room 1 1 Process Process 1 1 1 Process Process Process Process What are Some Clinic Processes? documentation medication refills lab review messages referrals forms management How Tasks Support Processes Specialist Referral Process Physician orders consult 4 minutes Tasks Make Appointment Clerk calls to make appointment 5 minutes Clerk gives appointment reminder and directions to patient Check-in to Nurse Dr. in to Dr. out Nurse to Room Check-out to leave Task How Tasks Support Processes Specialist Referral Process: Physician orders consult Task: Call to make appointment 4 minutes Clerk calls to make appointment Task: Give directions for specialist 5 minutes Clerk gives appointment reminder and directions to patient Task Provider Roles (continuum)… • MD with non-consistent nurse and clerical staffing • MD with consistent nurse staffing, but inconsistent clerical staff • MD with consistent nurse and clerical staffing • Group of providers with consistent RN, MA, and clerical staff Better! Clerical Staff Roles: (continuum) • Scheduler at front desk or in central area • Schedules and takes messages for many • Scheduler accountable to a group of providers • Scheduler actually co-located with the providers and patients they support Better! Nursing Roles: (Continuum) • Phone calls, rooming, paperwork, triage, scheduling • Nurse offers advice over the phone or through e-mail • Nurse manages populations of patients Better! What are the attributes of a Care Team? • Proactive vs. reactive • Communicative vs. isolated • Accountable to each other, and to the patient • Uses measures for feedback • Delivers high quality chronic, acute, and preventive care Attributes continued……. • Cross-trained versus territorial • Integrated versus separated • Continuous flow versus flow based on urgency • All staff work to highest level of training, experience, and licensure Flow Through the Office Clinical Teams This is about doing the right thing right! Clinical Teams • Refers to the “what” we provide for our patients • Depends on disease burden and evidence • Good clinical teams use every team member to the greatest extent of their license Panel Size 2000 66 have Diabetes 360 Patients are Over 65 113 have Asthma 60 Patients had more than 10 Office Visits Last Year 248 have Arthritis 130 are Clinically Depressed 228 have Hypertension 160 have Heart Disease ICD 9 Diagnosis 401 250 272 465 V70 Essential Hypertension Diabetes Mellitus Disorders of Lipid Metabolism Upper Resp. Infection…. General Medical Exam 780 473 724 462 477 General Symptoms Chronic Sinusitis ….Back Disorders… Acute Pharyngitis Allergic Rhinitis Chronic Dz Clinical Goals Diagnosis HTN DM Hgb A1c DM Foot DM Eye DM Lipids CVD Lipids MDD New Meds CHF Weight CAP - Culture Protocol? Our Outcomes Benchmark Chronic Dz Clinical Goals Diagnosis Protocol? Our Outcomes Benchmark HTN 75%<140/90 DM Hgb A1c DM Eye <12% > 9 85% 80% DM Lipids >80% LDL<120 CVD Lipids <20% LDL>100 MDD New Meds >77% >95% 92% DM Foot CHF Weight CAP - Culture Prevention Clinical Goals Prevention Protocol? Results Flu shot Colon Ca Breast Ca Cervical Ca Pneumo. V. MDD Screen SUD Screen Tob. Counsel Benchmark Prevention Clinical Goals Prevention Protocol? Results Flu shot Colon Ca Breast Ca Cervical Ca Pneumo. V. MDD Screen SUD Screen Tob. Counsel Benchmark >90% >75% >90% >90% >87% >95% >95% >93% Firm A Medical Outcomes: Baseline Through February '03 80% 70% Goal 50% % At 60% 40% 30% All Outcomes p < .01 A1c < 7.5 LDL cholesterol <100 20% BP < 140/90 10% Month Fe b03 03 Ja n- De c02 v02 No Oc t-0 2 02 Se p- g02 Au Ju l-0 2 -02 Ju n Ma y02 r-0 2 Ap Ma r -0 2 Fe b02 02 Ja n- Ba se lin e 0% Clinical Quality Indicators Oct 01 to Sept 05 Primary Care Dx Management 90% 80% 74% 74% 70% 60% 58% 61% 63% 66% 77% 72% 69% 64% 57% 66% 70% 69% 71% 70% 66% 65% 60% 58% 59% 54% 52% 47% 50% 40% 30% 20% 10% 0% % LDL < 100 Oct to Mar FY 02 Ap to Sept FY 02 % HgbA1c < 7.5 Oct to Mar FY 03 Ap to Sept FY 03 Oct to Mar FY 04 % BP< 140/90 Ap to Sept FY 04 Oct to Mar FY 05 Ap to Sept FY 05 Results: Improvement in CRC screening 80% 60% 40% 20% ne Au g No v De c Ja n Fe b M ay Ju ne Au g Oc t No v M ar ch M ay Ju ne Au g Ju ay 0% M % complete 100% 2003-2005 CRC Screening Stage IV CRC from Charleston VAMC Tumor Registry through April 1, 2005 7 6 5 4 Stage IV 3 2 1 0 2003 2004 2005 Teamwork It matters! A lot! Teamwork! Operational Improvement Team Home Team Clinical Airplane Accidents • In an analysis of 35,000 reports of incidents over 7.5 years, almost 50% resulted from a flight crew error, and an additional 35% were attributed to air traffic controller error • Communication was a significant factor in about ½ of the human errors. How Hazardous Is Health Care? (Leape) DANGEROUS (>1/1000) 100,000 REGULATED ULTRA-SAFE (<1/100K) HealthCare Total lives lost per year Driving 10,000 1,000 Scheduled Airlines 100 Mountain Climbing Bungee Jumping 10 Chemical Manufacturing Chartered Flights European Railroads Nuclear Power 1 1 10 100 1,000 10,000 100,000 Number of encounters for each fatality 1,000,000 10,000,000 Errors • JCAHO Data of 2034 Sentinel Events – Majority resulted in death – Communication root cause in 60% • VA Data of 10,000 near misses – Communication root cause in 55% It’s all about communication….. ………in a certain way Communication Example An Actual Radio Conversation between US Naval Ship & Canadian Authorities off the Newfoundland Coast October 1995 • Canadians: – Please divert your course 15 degrees to the south to avoid a collision. • Americans: – Recommend you divert your course 15 degrees to the north to avoid a collision. • Canadians: – Negative, you will have to divert your course 15 degrees south to avoid a collision. • Americans: – This is the Captain of a US Navy ship. I say again, divert your course. • Canadians: – No, I say again, you divert YOUR course. • Americans: – This is the Aircraft Carrier USS Lincoln, the 2nd largest ship in the Atlantic Fleet. We are accompanied by 3 destroyers, 3 cruisers, and numerous support vessels. I DEMAND that you change your course 15 degrees north, I say again, that’s one-five degrees north, or countermeasures will be undertaken to ensure the safety of this ship. • Canadians: – This is a lighthouse. Your call. An Actual Radio Conversation between US Naval Ship & Canadian Authorities off the Newfoundland Coast October 1995 Engagement • • • • • • Challenge Authority Autonomy Stimulation Access to information Growth opportunities • 20% highly engaged • 40% moderately • 20% unengaged • • • • Sr. Mgr 53% engaged Directors 25% Supervisors 18% Non mgt 12 to 14% • Higher in nonprofit sector Cooperation and Teamwork % Favorable % Neutral 100% 90% 80% 56 70% 60% 50% 40% 16 30% 20% 28 10% 0% Q.27 Cooperation and teamwork Results are shown from most to least favorable % Unfavorable Most Important Reasons People Leave • • • • 1. 2. 3. 4. Lack of Respect Not listened to Not involved No opportunity to increase responsibility • 5. Can’t make an impact • 6. Pay Do patients notice good teams? % Rating of Perfect Care by Patients Using These Office Practices Perfect Care (Patient Perspective) Correlated with Teamwork (Clinical Staff Perspective) for Ten Office Practices 90 80 70 60 R=.77; p=.01 50 40 30 20 From John H. Wasson MD - Dartmouth 10 0 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5 Rating of Teamwork In Office Practices (5 is Best) From John Wasson Surgery Service Story Surgery Service O:E Ratio 1.8 1.6 1.4 1.2 1 0.8 0.6 0.4 0.2 0 1 2 3 Best-Middle-Worst of 44 Services Morbidity Mortality Young, et al. Best Practices For Managing Surgery Services: The Role of Coordination. Health Care Management Review 22 (4), p 72 – 81. Well Functioning Teams Have: • • • • • • Leadership and direction Common aim Population of patients identified Shared work and process Shared information Flexibility Team Performance Curve High-performing Team Real Team Performance Work Group Potential Team PseudoTeam Effectiveness Source: “The Wisdom of Teams” Katzenbach/Smith Defining an Ideal Place to Work! Management Trust the people you work for Employee Be proud of what you do Job Enjoy the people you work with Other Employees 13 Month Rolling Average Staff Turnover 2002-2003 40.00% 35.00% 30.00% 25.00% 20.00% 15.00% 10.00% 5.00% 0.00% J-02 F-02 M -02 A-02 M -02 J-02 J-02 A-02 S-02 O-02 N-02 D-02 Voluntary J-03 F-03 M -03 A-03 M -03 J-03 J-03 A-03 S-03 Involuntary O-03 N-03 D-03 Summary • We know typical support staff numbers • We know typical support staff composition • We can probably markedly improve efficiency • We can discover population needs • We know a key difference between good and great teams is teamwork! Next 18 months… • Improve operational teams (LS 3) – Through “office efficiency” change ideas – Flow mapping & Task analysis – Measure lead time and cycle time • Improve clinical teams (LS 4) – Identify and improve chronic disease care – Identify and improve prevention care • Improve teamwork (Throughout) – Improve individual and team functioning Homework • Measure lead time (operational) • Discover top 10 diagnosis (clinical) • Talley chronic disease and prevention protocols (clinical) • “Take the test” page 3-11. Record answers on page 16 (teamwork) • Read championship teams introduction • DO module 1 and 2 in the book