Accessing Diabetes Education Through Tele-Health
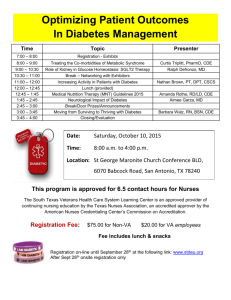
advertisement

Accessing Diabetes Education Through Telehealth M. Dianne Brown, MS, RDN, LD, CDE OU Physicians Diabetes Life Clinic at the Harold Hamm Diabetes Center Cynthia Scheideman-Miller, MHSA Heartland Telehealth Resource Center Oklahoma Telemedicine Conference 2014 October 16, 2014 Objectives: 1. Discus the benefits of a diabetes telehealth program for patients and how it can be partnered with provider education to improve diabetes management 2. List processes involved when selecting a diabetes telehealth program for your patients 3. Outline key components of a diabetes telehealth program including patient and provider site requirements. Why Diabetes Tele-education? 2011 2013 Prevalence* of Self-Reported Obesity Among U.S. Adults, by State, BRFSS State Prevalence Confidence Interval Oklahoma 32.5 (31.2, 33.9) 26 million Americans have diabetes Diabetes by the Numbers 79 million Americans have pre-diabetes 7th leading cause of death in the U.S. The research shows: People with Diabetes Providers • Don’t follow through on referral • Are emotional / shocked at diagnosis • End up relying on family / friends • Believe they know enough / can handle it on their own • Know importance of DE, but don’t necessarily prescribe – or don’t prescribe definitively enough • Sometimes forget to follow up with patients to encourage attendance Diabetes Education Patient Benefits Studies have shown people who receive diabetes education Use primary care / prevention services Take medications as prescribed Control glucose, blood pressure, LDL cholesterol Have lower health costs Diabetes Education Process Year 1 Patient Diagnosed with Diabetes PCP refers patient for DE Patient assessed by CDE *DSMT Class (10 hours) **MNT 3 hours (by RD) Year 2 2 hour Refresher Classes *DSMT - 2 hours & **MNT -2 hours (by RD) *Diabetes Self-Management Training (DSMT) **Medical Nutrition Therapy (MNT) Prevalence of Diabetes (2011 Overall) N/A 2.25% or Less 2.26% - 3.35% 3.36% - 5.04% 5.05% - 6.74% 6.75% - 8.44% 8.45% - 10.14% 10.15% - 11.84% 11.85% - 14.00% 14.01% or Greater Where most Certified Diabetes Educators (CDEs) Live in Oklahoma Recognized or Accredited Diabetes Education Programs in Oklahoma 34- Recognized by the American Diabetes Association (ADA) 17- Accredited by American Association of Diabetes Educators (AADE) Telehealth benefit # 1 Provides access- multiple sites may be used patients other health care providers Telehealth benefit #2 Saves money patient & CDE saves “gas” money remote site “borrows” CDE informed patients reduce hospital admission Telehealth benefit #3 Saves time patients & CDE do not lose time with travel and information is delivered in “real time” CDE can see more patients, reducing service wait time for patients Telehealth benefit #4 Helps to address cultural diversity which contributes to challenges of education, patient compliance, and cooperation with treatment regimens Increased ability for participation with diabetes care team Telehealth Concern #1 Budget Considerations technology set up on remote and originating sites Telehealth Concern #2 Time needed for set up Training Staff Patient teaching tools and resources at remote Telehealth Concern # 3 Services are only reimbursable by Medicare if the services were provided to a Medicare or Medicaid beneficiary at an acceptable originating site. Selecting a Diabetes Tele-education Program Define what you want vs need ADA program for Medicare reimbursement Champions Technology – fits in your needs and budget A program that is right for your organization and population served Sales pitches can be misleading Selecting a program Is this a program you want as a partner in patient care or contract with for total delivery? Do they follow the same State laws, Hospital by-laws as on-site programs are required to supply? What are their references? Are the providers (distant site) in Oklahoma? Double Check the Contract What if expectations aren’t met? Who is responsible for what? What staff will be needed at the originating site before, during, after the classes? Who gets the data? Who tracks patient satisfaction? Is there training for staff at the patient site? No-Show policy Telehealth Consent Form – who is responsible to get this signed prior to services? Developing a Diabetes Tele-Education Program Early Development Champion Support Administration Providers Originating Site Distant site Delivery Model Multiple sites or single site Contract vs direct billing Individual sessions conducted remotely or on-site Early Development, con. Program Components Understand current process flow and staffing: Multiple sites or single Optimal number and arrangement Mandatory documentation – define the who, where, how Resources Consider health literacy & culture What resources go with the patient or stay Budget Budget Start up costs Staff time Equipment Broadband Marketing Contract development Liaisons Staff prep for sessions Consultants Technology Software Reliable Image quality ASC X12 encryption standard Compatible with other software Linkage of older to newer technology Split screen capable Transmission requirements Technology Distant (Provider) End Computer High-definition camera Monitors – single will work, dual is better Speaker/microphone Projector Software – some have split screen capabilities Desktop – Self-contained High quality image Split screen capabilities Frees up computer for EHR Technology Originating (Patient) Site Patient Cart High-quality image Can be wheeled to patient bedside Multi-purpose Issue: mobility vs larger monitor Wall-mounted Monitors High quality image Split screen capabilities The closer to “real” size, the better Reimbursement: Medicare Medicaid • ADA approved program • Service must be real time using interactive audio/video • Eligible originating (patient) site – rural HPSA – online tool to determine eligibility • Codes: • 99201 GT modifier • HCPCS codes G0108 & G0109 • ADA approved program • Service must be real time using interactive audio/video • Eligible originating (patient) site • Codes: 99201, 9780297803 GT modifier • Must be delivered using appropriate equipment and meet HIPAA, privacy & security requirements Reimbursement (con.): Medicare Medicaid • Eligible originating site • Office of physician/practitioner • Hospital • CAH • RHC • FQHC • Eligible originating site • Office of physician/practitioner • Hospital • CAH • RHC • FQHC • School • I/T/U • Eligible provider • Registered Dietitian • Advanced Registered Nurse Practitioners • Nutrition professional • Clinical Social Worker • Eligible Provider • Registered Dietitian • Advance Registered Nurse Practitioners Food Models Handouts such as: My Carbohydrate Guide Organize the classroom -Pens, highlighters, sharpies -Ketone chart and strips -Glucose wands -Food models -Sample of fast acting glucose -Etc. Diabetes Education Tele-health Patient Take Home Resources • Have topics organized by title and number the file (or computer files) • Have reference list to find resource topics quickly. Final Development Staff training User training Cheat Sheet Troubleshooting Guide Help Desk Contingency Plan Helpdesk visit 3rd level vendor support Patient recruitment Marketing material tele-health brochure internal web page Clinician invitation Patient Mailing Telehealth Patient Consent Form Diabetes Tele-education Pilot Instructors Dietitian at one rural location, nurse specialist at the other Diabetes tele-education delivered at a lower cost LOS shorter for those who attended class – reduced hospital costs Pre- and Post-tests comparable to on-site classes High patient and provider satisfaction Rapport between class attendees unforeseen plus Telemedicine Patient Satisfaction Survey Question How comfortable did you feel? (0, very comfortable; 5 very comfortable) Score_________ 4.2 ± 1.2 (19) How convenient was the encounter? (0, not at all convenient ; 5 very convenient) 4.4± 1.0 (19) Was the lack of physical contact acceptable? (0, not acceptable; 5 very acceptable) 4.3 ± 1.3 (19) Concerns about privacy? (0, no concerns; 5 very concerned) 1.1± 1.7 (19) Overall satisfaction? (0, not at all satisfied; 5 very satisfied) 4.3± 1.3 (19) Would you do it again? (yes/no) Diabetes Care, Vol. 26, No 4, April 2003 16/3 Quality Checks: Metrics Utilization Satisfaction Sustainability Outcomes By location patient financial health By service provider support care plan By provider staff champions no-show Rynn Geier, MBA, RD, LD, CDE presented at AADE annual meeting Aug 6-9 2014 Summary: Establish goals for a telemedicine program Gain champion support Develop a budget Choose a vendor Take time for clinical training and well-planned program deployment Develop strategies for program “buy –in” Build into your program Measure your outcomes: metrics Don’t Forget Diabetes Education for Providers Providers have the same information as their patients Increases provider’s confidence that they have the latest diabetes information Reinforcement – patient’s hear the same message Providers have a contact/mentor “Prior to the study it was almost impossible for this type of patient to get the consultation and specialized care that is not accessible in a small rural community.” Rural Home Health Administrator Who knows what future telehealth will look like?