Sympathetic nervous system
advertisement

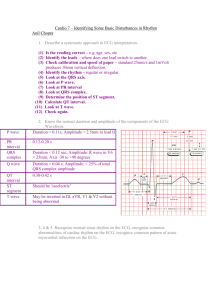
DYSRHYTMIAS & Hemodynamic Monitoring Cardiac Rhythm Monitoring 12 lead ECG Telemetry Halter monitor Bedside monitor Lead placement 12 lead 12 lead ECG Diagnostic Structural changes Ischemia Infarction Enlarged cardiac chambers Electrolyte imbalances Drug toxicity Assessment of dysrhythmias Lead placement 5 lead 5 lead monitoring Telemetry monitoring ICU Holter monitors Provides more views in different leads Lead placement 3 lead Three Lead Less lead views Simple monitoring Quick Patch Considerations Properly prepare skin Clip excessive hair on the chest wall with scissors Gently rub the skin with dry gauze If skin is oily, wipe with alcohol first Heart Anatomy & Conduction System Conduction System Properties of Cardiac Cells Automaticity Excitability Ability to initiate an impulse spontaneously and continuously Ability to be electrically stimulated Conductivity Ability to transmit an impulse along membrane in an orderly manner Contractility Ability to respond mechanically to an impulse Nervous System Control of the Heart Autonomic nervous system controls: Rate of impulse formation Speed of conduction Strength of contraction Nervous System Control of the Heart Parasympathetic nerve nervous system Vagus Decreases rate Slows impulse conduction Decreases force of contraction Nervous System Control of the Heart Sympathetic nervous system Increases rate Increases force of contraction Intrinsic Rates of the Conduction System SA 60-100 AV node node 40-60 Bundle of His, Purkinje fibers 20-40 Ventricles <20 P Wave Atrial depolarization Firing of SA node Should be upright Normal duration 0.06-0.12 sec Source of variation Disturbance in atria PR Interval Impulse through atria to AV node, bundle of His Measured from beginning of P wave to beginning of QRS complex Normal duration 0.12-0.20 sec Source of variation Short – impulse from AV junction Longer – AV block QRS Interval Ventricular Depolarization Atrial repolarization Measured from the beginning to end of QRS complex Normal is not always a traditional wave form Normal duration Hidden in wave < 0.12 sec Source of variation Disturbance in bundle branches or in ventricles QRS variations not everyone has “normal” QRS ST Segment Time between ventricular depolarization and repolarization Should be flat (isoelectric) Look for elevation or depression Normal duration ST elevation – myocardial injury ST depression – reciprocal changes and ischemia 0.12 sec Source of variation Ischemia Injury infarction T Wave Ventricular repolarization Should be upright Follows QRS complex Larger than a P wave Inversion indicates ischemia to myocardium Normal duration 0.16 sec Sources of variation Electrolyte imbalances Ischemia Infarction QT Interval Beginning of QRS complex to end of T wave Represents time taken for entire ventricular depolarization and repolarization Normal duration 0.34-0.43 sec Sources of variation Drugs Electrolyte imbalances Changes in heart rate – inverse relationship U Wave Sometimes seen after T wave ?? May be normal May indicate hypokalemia Rhythm interpretation A Systematic Approach Rules for Systematic Interpretation If the rhythm doesn’t look right check your patient! Treat the patient not the monitor Is the rhythm regular or irregular – R to R, then P to P What is the heart rate Can you identify P waves Can you identify QRS complexes & T waves What is the ratio of P waves to QRS complexes What is the PR interval Anything else you notice that shouldn’t be there Calculating Heart Rate Regular Small blocks into 1500 Large blocks into 300 Irregular = 6-second strip Divide by 300 between waves Atrial Rhythms Rhythms that originate in the atria Normal Sinus Rhythm Follows normal conduction pattern Rate 60-100 P wave Normal , one per QRS PR interval Normal, consistent (0.12-0.20) QRS complex Normal (<0.12) Sinus Bradycardia ECG characteristics Rhythm Rate Normal, one per QRS PR interval <60 P wave Regular, slow 0.12-0.20, consistent QRS complex Normal, <0.12 Sinus Bradycardia Clinical Associations Normal in fit, athletic individuals Normal in sleep Increased vagal tone –e.g. vomiting Drugs Beta blockers Calcium channel blockers Hypothyroidism MI Increased intracranial pressure Hypoglycemia Sinus Bradycardia Clinical significance Dependent on patient tolerance Symptomatic Pale Cool skin Hypotension Weakness Angina Dizziness Syncope Confusion or disorientation SOB Sinus Bradycardia Treatment Atropine Pacemaker Treat underlying cause Sinus Tachycardia ECG characteristics Rhythm Rate Normal, one for every QRS PR interval 100-200 P wave Regular, fast 0.12-0.20, consistent QRS complex Normal, <0.12 Sinus Tachycardia Clinical Associations Exercise Anxiety, pain, fear Hypotension Hyperthyroidism Hypovolemia Anemia Hypoxia Hypoglycemia MI Heart failure Sinus Tachycardia Clinical Associations (cont’d) Drugs Epinephrine Norepinephrine Atropine Caffeine Theophylline Nifedipine Hydralazine Sudafed Sinus Tachycardia Clinical significance Dependent on tolerance Symptoms Dizziness Dyspnea Hypotension Angina Treatment Treat underlying cause Vagal maneuvers Beta blockers Sinus Arrhythmia ECG characteristics Rhythm Irregular, but with a pattern Speeds up with respiration Rate P wave normal PR interval 60-100 normal QRS complex normal Sinus Arrhythmia Clinical Associations Clinical significance Treatment Atrial Fibrillation ECG characteristics Rhythm irregular Rate Atrial 350-600, irregular Ventricular - < & > 100 – irregular P wave Irregular, chaotic PR interval Not measurable QRS complex normal Atrial Fibrillation Clinical Associations CAD Rheumatic heart disease cardiomyopathy Hypertensive heart disease Heart failure Pericarditis Thyrotoxicosis Alcohol intoxication Caffeine Electrolyte disturbances Stress Cardiac surgery Atrial Fibrillation Clinical significance Most common, clinically significant dysrhythmia Decreased cardiac output Thrombus formation Stroke Accounts for as many as 20% of all strokes Treatment Calcium channel blockers Beta blockers Digoxin Amiodarone Cardioversion Anticoagulation therapy Atrial Flutter ECG characteristics Rhythm Rate Flutter waves – sawtoothed More than QRS complexes – may be in a ratio PR interval Atrial – 200-350 and regular Ventricular - < & > 100 – regular or irregular P wave May be regular or irregular Not measurable QRS complex Normal Atrial Flutter Clinical Associations CAD HTN Mitral valve disorders PE’s Chronic lung disease Cor pulmonale Cardiomyopathy Hyperthyroidism Digoxin Quinidine Epinephrine Atrial Flutter Clinical significance Decrease cardiac output Heart failure Increased risk of stroke Treatment Slow ventricular response by increasing AV block Calcium channel blockers Beta blockers Cardioversion Amiodarone Rhythmol Ablation Supraventricular Tachycardia ECG characteristics Rhythm Rate Regular 150-220 P wave Difficult to determine – may be hidden Abnormal PR interval Normal or shortened QRS complex Normal Supraventricular Tachycardia Clinical Associations Overexertion Emotional stress Deep inspiration Caffeine Tobacco Rheumatic heart disease Digitalis toxicity CAD Cor pulmonale Supraventricular Tachycardia Clinical significance Prolonged episodes may precipitate decreased cardiac output Symptoms Hypotension Dyspnea Angina Treatment Vagal stimulation Valsalva maneuver Drugs Adenosine Beta blockers Calcium channel blockers Cardioversion Asystole There is no electrical activity in the heart during asystole, therefore there will only be a flat line on the rhythm strip Asystole Clinical Associations Clinical significance Advanced cardiac disease Severe cardiac conduction system disturbance End stage heart failure Prolonged arrest, may not be resuscitated Treatment CPR with ACLS Epinephrine Atropine Intubation Transcutaneous temporary pacemaker Premature Beats Premature Atrial Contractions (PAC’s) Beats occur early in the cycle and there is no compensatory pause ECG characteristics Rhythm irregular Rate Dependent on underlying rhythm P wave Abnormal shape PR interval Normal Will be different than underlying rhythm QRS complex Normal Premature Atrial Contractions (PAC’s) Clinical Associations Can occur normally Emotional stress Physical fatigue Alcohol Caffeine Tobacco CHF Ischemia COPD Hypoxia Hyperthyroidism CAD Premature Atrial Contractions (PAC’s) Clinical significance In healthy hearts, not significant Symptoms Heart “skipped” beat Palpitations May be early indication of more serious dysrhythmias Treatment Reduce stimulants Beta blockers Premature Ventricular Contractions (PVC’s) Beat early in cycle with compensatory pause ECG characteristics Rhythm Rate No P wave with premature beat PR interval Dependent on underlying rhythm P wave irregular none QRS complex Wide bizarre, >0.12 Premature Ventricular Contractions (PVC’s) Bigeminy Trigeminy All PVC’s from same source Look alike Multifocal Every third beat is a PVC Unifocal Every other beat is a PVC Different sources of beat Beats look different Couplet Two in a row Runs will turn into V-tach Premature Ventricular Contractions (PVC’s) Clinical Associations Caffeine Alcohol Nicotine Aminophylline Epinephrine Digoxin Electrolyte imbalances Hypoxia Fever Exercise Emotional stress MI Mitral valve prolapse Heart failure CAD Premature Ventricular Contractions (PVC’s) Clinical significance Usually benign May precipitate Decreased cardiac output Angina Heart failure Assess apical-radial pulse rate Treatment Treat underlying cause Beta blockers Procainamide Amiodarone Lidocaine Premature Junctional Contractions (PJC’s) Beat occurs early in cycle and no compensatory pause ECG characteristics Rhythm Rate May or may not be present – if present will be inverted PR interval Dependent on underlying rhythm P wave Irregular Different from underlying rhythm if there at all QRS complex normal Premature Junctional Contractions (PJC’s) Clinical significance &Treatment Similar to PAC’s Junctional Rhythms Originate below atria and above ventricles Junctional Rhythm ECG characteristics Rhythm regular Rate 40-60 P wave Inverted, may be hidden in QRS complex PR interval Shortened or missing QRS complex normal Accelerated Junctional Rhythm & Junctional Tachycardia ECG characteristics Rhythm regular Rate 60-180 P wave Inverted, may be hidden in QRS complex PR interval Shortened or missing QRS complex normal Junctional Dysrhythmias Clinical Associations CAD Heart failure Cardiomyopathy Electrolyte imbalances Inferior MI Rheumatic heart disease Digoxin Amphetamines Caffeine Nicotine Junctional Dysrhythmias Clinical significance Occur when the SA node has not been effective If increases to junctional tachycardia patient may become hemodynamically unstable Treatment Dependent on tolerance Atropine Beta blockers Calcium channel blockers Amiodarone Ventricular Rhythms Originate in the ventricles Idioventricular Rhythm ECG characteristics Rhythm Rate none PR interval 20-40 P wave Regular absent QRS complex Wide, bizarre >0.20 Ventricular Tachycardia ECG characteristics Rhythm Rate none PR interval Ventricular rate 150-250 P wave Regular R to R none QRS complex Wide, bizarre, > 0.12 Ventricular Tachycardia Run of three or more PVC’s Clinical Associations MI CAD Significant electrolyte imbalances Cardiomyopathy Mitral valve prolapse Long QT syndrome Drug toxicity CNS disorders Ventricular Tachycardia Clinical significance Stable – patient has a pulse Unstable – no pulse Decreased cardiac output Hypotension Pulmonary edema Decreased cerebral blood flow Cardio-pulmonary arrest Ventricular Tachycardia Treatment Treat quickly Identify and treat underlying causes Procainamide Sotalol Amiodarone Lidocaine Beta blockers Magnesium Dilantin Cardioversion CPR & ACLS Ventricular Fibrillation ECG characteristics Rhythm Rate No P waves PR interval No rate P wave No rhythm present none QRS complex none Ventricular Fibrillation Clinical associations Acute MI Myocardial ischemia Heart failure Cardiomyopathy Cardiac catheterization Cardiac pacing Accidental electric shock Hyperkalemia Hypoxemia Acidosis Drug toxicity Ventricular Fibrillation Clinical significance Symptoms Unresponsive Pulseless Apneic state If not treated rapidly, patient will die Treatment Immediate CPR & ACLS Immediate defibrillation Ventricular Standstill ECG characteristics Rhythm Rate normal PR interval Atria 60-80 P wave Regular p waves none QRS complex none Heart Blocks First Degree AV Block ECG characteristics Rhythm Rate Normal PR interval Normal P wave Regular >0.20 QRS complex normal First Degree AV Block Clinical Association MI CAD Rheumatic fever Hyperthyroidism Vagal stimulation Digoxin Beta blockers Calcium channel blockers First Degree AV Block Clinical significance Usually not serious Can be a precursor for higher degrees of AV block Patients are asymptomatic Treatment No treatment unless caused by medications Monitor patient for increase in block Second Degree AV Block – Type I Also called Mobitz I or Wenckebach ECG characteristics Rhythm Rate More p waves than QRS complexes PR interval Atrial – normal and regular Ventricular – slightly higher than atrial rate P wave Irregular Progressing lengths until drops QRS QRS complex Normal and then one dropped Second Degree AV Block – Type I Clinical Association Clinical significance Digoxin Beta blockers CAD Myocardial ischemia or infarction Generally transient and well tolerate May be warning sign for a more serious AV disturbance Treatment Symptomatic Atropine Temporary pacemaker Asymptomatic Closely monitored Transcutaneous pacer on standby Second Degree AV Block – Type II Also called Mobitz II ECG characteristics Rhythm Rate More p waves than QRS complexes, stated in a ratio PR interval Atrial – normal and regular Ventricular – slower, regular or irregular P wave Irregular Regular if consistent conduction ratio Normal or prolonged QRS complex Preceded by two or more P waves Second Degree AV Block – Type II Clinical Association Clinical significance Rheumatic heart disease CAD Anterior MI Drug toxicity Often progresses to third degree AV block Poor prognosis Decreased cardiac output Hypotension Myocardial ischemia Treatment Permanent pacemaker Third Degree AV Block ECG characteristics Rhythm Rate Normal, more P waves than QRS complexes PR interval Atrial 60-100 Ventricular 20-60, dependent on focus P wave R-R regular P-P regular No relationship between P waves and QRS complexes QRS complex Dependent on focus Third Degree AV Block Clinical Association Severe heart disease CAD MI Myocarditis Cardiomyopathy Amyloidosis Scleroderma Digoxin Beta blockers Calcium channel blockers Third Degree AV Block Clinical significance Reduced cardiac output Ischemia Heart failure Shock Syncope possible periods of asystole Treatment Pacemaker Atropine Epinephrine Dopamine Calcium chloride Bundle Branch Blocks ECG characteristics QRS complex Wide, bizarre Bundle Branch Blocks Clinical significance Treatment • http://www.skillstat.com/Flash/ECG_Sim_ 2004.html • http://www.nobelprize.org/educational/ medicine/ecg/index.html • http://www.iphoneappsplus.com/medic al/instant-ecg--an-electrocardiogramrhythms-interpretation-guide/index.htm Defibrillation & Cardioversion Including pacemakers and implanted cardioverter defibrillator Lifepak Can be used as defibrillator, monitor, or transcutaneous pacer Defibrillation The use of a carefully controlled electric shock, administered either through a device on the exterior of the chest wall or directly to the exposed heart muscle, to restart or normalize heart rhythms. Most effective method of terminating V-Fib and pulseless V-Tach Deliver energy using a monophasic or biphasic waveform Monophasic defibrillators deliver energy in one direction. Biphasic defibrillators deliver energy in two directions. Deliver successful shocks at lower energies Fewer post shock ECG abnormalities Defibrillation Output is measured in joules or watts per second. Recommended energy for initial shocks in defibrillation Biphasic defibrillators: First and successive shocks: 150 to 200 joules Monophasic defibrillators: Initial shock at 360 joules Defibrillation Indications Pulseless v-tach V-fib Always done as emergent Contraindications Multifocal atrial tachycardia Digitalis toxicity Cardioversion Restoration of normal heart rhythm: the use of an electric shock to convert a dangerously rapid, fluttering, and ineffective heartbeat to its normal rhythm Synchronized circuit delivers a counter shock on the R wave of the QRS Synchronizer switch must be turned ON Cardioversion Indications A-fib If unstable or new witnessed onset – may do without anticoagulation but preferred method is with anticoagulation three weeks prior TEE to rule out blood clots A-flutter (if unstable) Anticoagulation therapy Stable V-tach (with pulse) If patient does not respond to medications Contraindications Digitalis toxicity associated tachycardia Defibrillation & Cardioversion Nursing Considerations IV access Airway management equipment Sedative drugs Monitor Be aware of possible implanted devices Firm pressure when discharging Decrease chance for arcing and burns Clear of patient and bed Defibrillation & Cardioversion Complications Hypoxia or hypoventilation from sedation Burns Mostly superficial some deep tissue Dysrhythmias Premature beats V-fib Hypotension Pulmonary edema Thromboembolization Myocardial necrosis r/t high energy discharge ICD’s & Pacemakers Implantable CardioverterDefibrillators (ICD’s) A, The implantable cardioverter-defibrillator (ICD) pulse generator from Medtronic, Inc. B, The ICD is placed in a subcutaneous pocket over the pectoralis muscle. A single-lead system is placed transvenously from the pulse generator to the endocardium. The single lead detects dysrhythmias and delivers an electric shock to the heart muscle. Indications for ICD Spontaneous sustained v-tach Syncope with inducible v-tach/v-fib during EP study At high risk for future life-threatening dysrhythmias (cardiomyopathy) Have survived cardiac arrest ICD’s Consists of a lead system placed via subclavian vein to the endocardium Battery-powered pulse generator is implanted subcutaneously ICD sensing system monitors the HR and rhythm and identifies VT or VF. Approximately 25 seconds after detecting VT or VF, ICD delivers <25 joules. If first shock is unsuccessful, ICD recycles and delivers successive shocks ICD’S ICDs are equipped with anti-tachycardia and anti-bradycardia pacemakers. Initiate overdrive pacing of supraventricular and ventricular tachycardias Provide backup pacing for brady dysrhythmias that may occur after defibrillation discharges Education is extremely important Participation in an ICD support group should be encouraged Pacemakers A, A dual-chamber rateresponsive pacemaker from Medtronic, Inc., is designed to treat patients with chronic heart problems in which the heart beats too slowly to adequately support the body's circulation needs. B, Pacing leads in both the atrium and ventricle enable a dual-chamber pacemaker to sense and pace in both heart chambers. Pacemakers Used to pace the heart when the normal conduction pathway is damaged or diseased Pacing circuit consists of a power source, one or more conducting (pacing) leads, and the myocardium Pacemaker types Permanent Single chamber Dual chamber Temporary Transcutaneous Transvenous epicardial Indications for permanent pacemakers Indications for a temporary pacemaker Pacemakers Anti-bradycardia pacing Anti-tachycardia pacing: Delivery of a stimulus to the ventricle to terminate tachydysrhythmias Overdrive pacing: Pacing the atrium at rates of 200 to 500 impulses per minute to terminate atrial tachycardias Permanent pacemaker: Implanted totally within the body Cardiac resynchronization therapy (CRT): Pacing technique that resynchronizes the cardiac cycle by pacing both ventricles Temporary pacemakers Temporary pacemaker: Power source outside the body Transvenous Leads threaded through veins to right atrium or ventricle Epicardial Placed during cardiac surgery – leads are passed through the chest wall and can be attached to an external power source Transcutaneous Placed one lead on top of chest and one lead posterior ICD’s & Pacemakers Complications Infection Hematoma formation at sites of insertion Pneumothorax Failure to sense or capture Perforation of atrial or ventricular septum by the pacing lead Corrosion of leads Battery depletion ECG Changes Associated with ACS ECG changes in ACS Ischemia ST segment depression and/or T wave inversion ST segment depression is significant if it is at least 1 mm (one small box) below the isoelectric line. ECG changes in ACS Changes occur in response to the electrical disturbance in myocardial cells due to inadequate supply of oxygen. Once treated (adequate blood flow is restored), ECG changes resolve and ECG returns to baseline ECG changes in ACS Injury ST segment elevation is significant if >1 mm above the isoelectric line. If treatment is prompt and effective, may avoid infarction If serum cardiac markers are present, an ST-segmentelevation myocardial infarction (STEMI) has occurred. ECG changes in ACS Infarction Physiologic Q wave is the first negative deflection following the P wave. Small and narrow (<0.04 second in duration) Pathologic Q wave is deep and >0.03 second in duration ECG changes in ACS Infarction Pathologic Q wave indicates that at least half the thickness of the heart wall is involved. Referred to as a Q wave MI Pathologic Q wave may be present indefinitely. T wave inversion related to infarction occurs within hours and may persist for months