pain during inflation of balloon
advertisement

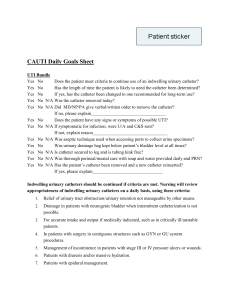
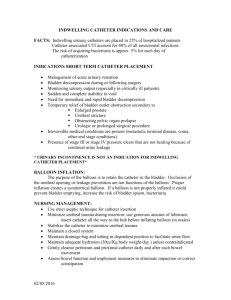
Reducing Iatrogenic Urethral Injury and Urinary Tract Infections Colleen Kasa RN BScN CMSN© CNE Urology May 2015 UTI’S ► 600,000 patients developed hospital acquired UTI per year ► 80% of these are urinary catheter associated (CAUTI) ► Common pathogens: E. Coli, Klebsiella, Proteus, enterococcus, Psuedomonas, Candida. ► Every day that catheter remains, risk of CAUTI increases by 5%; 100% in 30 days ► PROMPTLY REMOVE UNNECESSARY URINARY CATHETERS Indications for a urinary catheter ► Urinary tract obstruction ► Gross hematuria with clots ► Neurogenic bladder dysfunction or urinary retention ► Urologic or other surgery or studies ► Stage 3 or 4 sacral area decubitus ulcer with incontinence ► Accurate outputs in critically ill patients ► Hospice or palliative (if patient requests) Migrating Bacteria ► Immunocompromised patients ► Patients on antibiotics – fungus/yeast ► Introduction of the bacteria with the insertion, especially if mucosal disrupted ► Migrate up the catheter in the periurethral sheath ► Migrate up the internal lumen of the catheter if break in the closed drainage system – reduce UTI’s to 25% Catheters are NOT for: ► Incontinence ► Immobility ► Obtaining specimens ► Monitoring of outputs ► Patient request/convenience Strongly Recommended-CDC 1. 2. 3. 4. 5. 6. 7. 8. 9. Educate personnel in correct techniques of catheter insertion and care Catheterize only when necessary Emphasize handwashing Insert catheter using aseptic technique and sterile equipment Secure catheter properly Maintain closed sterile drainage Obtain Urine samples asepticlly Maintain unobstructed urine flow Empty drainage system at least every 8 hours, using aseptic technique, pt. specific container Moderately Recommended 1. 2. 3. 4. 5. Periodically re-educate personnel in catheter care Use smallest suitable bore catheter and balloon possible Avoid irrigation unless needed to prevent obstruction Refrain from daily meatal care Do not change catheters at regular intervals Weakly Recommended 1. 2. 3. 4. Consider alternative techniques of urinary drainage Replace the collection system when sterile closed system has been violated Spatially separating infected and uninfected patients with indwelling catheters Avoid routine bacteriologic monitoring Other Complications 1. 2. 3. Non bacterial urethral inflammation Urethral strictures Mechanical Trauma (catheter not stabilized, confused patients, etc) Any traumatic/difficult catheterization predisposes the male urethra to future difficulties…scarring, false passages, fistulas. Catheters ► Clean Intermittent Catheters ► Foley Catheters Size 14-16 French ► Materials: latex, silicone, lubricious ► Balloon Sizes: 5cc to 30cc ► 3-Way catheters: balloons 30cc – often 45-50cc in balloon – may actually be tethered into the prostatic fossa (applies pressure to the operative site) ► Used for continuous bladder irrigation (TURP`s) Notice the functional diameter of the holes Female Catheterization Male Anatomy Benign Prostatic Hypertrophy Pressure Points in the Male Urethra Support the troops! Urethral Tear Inspect carefully for meatal damage Paraphimosis with constriction Edema and Discoloration Manual reduction of Paraphimosis Catheter in Male Bladder Difficult Catheterizations (Male) ► Resistance - not the nurses fault ► (strictures, false passages, scarring, BPH) ► Pain During Insertion ► (explanations, pointing toes, Xylocaine gel) ► (consider specially shaped catheters-coude) ► PAIN DURING INFLATION OF BALLOON Problem with Female Catheterizations ► Difficulty Visualizing Urethra ► (good lighting, know anatomy, review history for bladder repair, female circumcision, have patient bear down as if to void..urethra opens) ► How many of you have put the catheter into the vagina? (leave it there so you know where not to go!) ► Difficulty with insertion- abuse ► (use smaller catheter, explanations, consider Xylocaine gel for lubrication of catheter) Xylocaine Gel Physician’s Order (some programs may have standing order) ► Xylocaine must be sterile ► Insert into the urethra for 5 - 15 minutes. 1. Opens the posterior urethra (hold penis at 90 degrees to straighten the path)(TUG) 2. Lubricates the path for the catheter 3. Desensitizes the urethra during and after the procedure 4. Psychological benefit – you are acknowledging that this is unpleasant and you are doing your best to alleviate discomfort ► Xylocaine Syringe Checklist for Proper Placement of Catheter ► 1. ► 2. ► 3. ► 4. ► 5. ► ► 6. ► Insert Catheter to the hub Wait for Urine return (? flush) Catheter does not recoil when released Balloon fills without resistance Patient does not have pain during inflation Balloon can be brought to the wall of the bladder Moving Along Question 1 ► 1. How often does a catheter need to be changed? Answer 1 ► Catheters should not be routinely changed. ► Always follow manufacturers’ recommendations ► Change catheter if encrusted, plugged or not functioning well ► In general short term catheters are intended for 510 days (latex foley) ► Long term catheters can remain as long as functioning well (silicone, silastic) ► NB: catheters should be last resort for urine drainage. Question 2 ► Should you ever irrigate a catheter? Answer 2 ► Generally catheters should not be irrigated, as bacteria and/or debris can be forced back into he bladder and potentially cause infection. ► However, when a catheter is initially inserted, the catheter may need to be irrigated to flush out any lubrication that may be obstructing the drainage eye. ► Three way catheters are intended to be irrigated to flush out clots and keep the catheter patent. Question 3 ► Doesn’t a bigger catheter do a better job? Answer 3 ► No, the smallest catheter that allows free flow of the urine is best. The periurethral mucosa is less compressed and is able to do a better job of lubricating the urethra and deterring bacterial migration up the outside of the catheter Question 4 ► Isn’t a bigger balloon better to hold the catheter in place? Answer 4 A bigger balloon actually causes stress at the bladder sphincter (1cc of H2O weighs 1 gm) May cause spasms, significant injury if catheter is removed with the balloon intact ► A larger balloon holds the drainage higher in the urine at the base of the bladderleaves residual of urine at the base Large Balloon Problems Question 5 ► How forceful should a nurse be to get a catheter inserted? Answer 5 Steady even pressure should be all that is required to insert a urinary catheter ► Knowledge about the anatomy is essential so the nurse is aware of the locality of spincters, which might spasm during insertion and require a hesitation ► Explanations, xylocaine gel, breathing techniques all assist the patient to relax the ► Sphincters ► If catheter is not inserting easily…STOP and get help! Consider coude catheter, experienced nurse or urologist. ► Question 6 ► What kind of catheter is best for the patient? Answer 6 ► Often best solution is no catheter ► Consider the purpose for the catheter (ie. Draining large clots will require a much larger catheter) ► Generally the smallest catheter to drain the bladder is the best ► Consider latex allergies…most catheters are made of a latex combination ► Latex is generally used for short term (5-10 days) and silicone for long term (>10 days) Question 7 ► Why should a catheter be tethered? Answer 7 Both make and female catheters should be tethered to maintain the integrity of the urethral mucosa (reduces pistoning effect) and reduces the pressure on the urinary tract spincters and stress points Question 8 ► What if no urine comes out of the catheter? Answer 8 ► Possible considerations: ► patient may have just voided ► Catheter isn’t in the bladder ► Catheter is plugged – drainage eye, catheter may be bent, catheter may be above the bladder…need gravity to flow ► Patient may be hypovolemic….may need bolus to have urine Question 9 ► What causes a catheter to bypass? Answer 9 ► Bypassing is caused by detrusor instability ► Common Causes: ► Obstruction: clots, encrustation, kinking ► constipation ► infection ► large balloon…5gms vs. 30gms Question 10 ► Why cc.? can’t you just fill a 10cc balloon with 5 Answer 10 ►A balloon should always be spherical and symmetrical in the bladder. This prevents potential erosion of the bladder mucosa and sphincter. It also keeps the drainage eye lower in the urine, allowing for better drainage. We’re Finished! References 1) Amukele Samuel A, Lee Gene W., et al 20-Year Experience with Iatrogenic Penile Injury The Journal of Urology Copyright © 2003 by American Urological Association Vol. 170, 1691-1694 October 2003 2) APIC Centers for Disease Control and Prevention Infectious Diseases Society of America Society for Healthcare Epidemiology of America et al Getting Started Kit: Prevent Catheter-Associated Urinary Tract Infections How-to Guide pages 1-32 3) Canes, David MD Male Urethral Catheterization The New England Journal of Medicine Volume 344:1178-1179 September 14, 2006 Number 11 4) Chung c, Chu M, et al. Comparison of lignocaine and water-based lubricating gels for female urethral catheterization, Emergency Medicine Australas.2007 Aug;19(4):315-9 5) Conterno LO, Mayhew A, Pereira CR The Cochrane Collaboration Intervention aimed at improving professional adherence to guidelines for prevention of device-related infections (Protocol) Copyright © 2009 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. 6) Cummings James M. MD, Boullier John MD, Urethral Trauma emedicine.medscape.com, Updated Jul 13, 2006 7) Dandan Imad S, MD, Farhat Walid, MD Trauma, Lower Genitourinary emedicine.medscape.com Updated April 16, 2009 8) DohertyW. Instillagel: an anesthetic antiseptic gel for use in catheterization. Br J Nurs. 1999 Ja28-Feb 10;8(2):109-12. Review. 9) Gray Mikel L Securing the Indwelling Catheter AJN December 2008 Vol 108, No 12 pages 4451 References (continued) 10) Greene Linda, Marx James, et al Guide to the Elimination of Catheter-Associated Urinary Tract Infections (CAUTIs) Developing and Applying Facility-Based prevention Interventions in Acute and Long-Term Care Settings Association for Professionals in Infection Control and epidemiology pages 1-41 11) Kashefi Carol, Messer Karen, et al Incidence and Prevention of Iatrogenic Urethral Injuries The Journal of Urology Copyright © 2008 by American Urological Association Vol. 179, 2254-2258, June 2008 12) Kelly Janis ADHD Medications Narrow But Do Not Close the Academic Achievement Gap www.medscape.com 13) Leone Marc, Perrin Anne-Sohpie et al A randomized trial of catheter change and short course of antibiotics for asymptomatic bacteriuria in catheterized ICU patients Intensive Care Med (2007) 33:726-729 14) Lo, Evelyn MD; Nicolle, Lindsay MD; et al Strategies to Prevent Catheter-associated Urinary Tract Infections in Acute Care Hospitals S41 Infection Control and Hospital Epidemiology October 2008, Vol. 29, Supplement 1 15) Moore Katherine, Rayome R. Problem solving and Troaubleshooting: The Indwelling Catheter. JWOCN. 1995. Volume 22 (5) 16) Moore Katherine N, Hunter Kathleen F, et al Do Catheter Washouts Extend Patency Time in Long-term Indwelling Urethral Catheters? JWOCN January/February 2009 Copyright © 2009 by the Wound, Ostomy and Continence Nurses Society pages 82-90 References (continued) 17) Nazarko, Linda Effective evidence based catheter management British Journal of Community Nursing Vol 13, No 3 110-114 18) Newman, Diane K The Indwelling Urinary Catheter Principles for Best Practice Journal of Wound, Ostomy and Continence Nursing November/December 2007 volume 34 Number 6 pages 655-661 19) Parker Diana, Callan Laurie et al Catheter-Associated Urinary Tract Infections JWOCN March/April 2009 Copyright © 2009 by the Wound, Ostomy and Continence Nurses Society pages 156-159 20) Parker Diana, Callan Laurie et al Nursing Interventions to Reduce the Risk of CatheterAssociated Urinary Tract Infection Part 1: Catheter Selection JWOCN January/February 2009 Copyright © 2009 by the Wound, Ostomy and Continence Nurses Society pages 23-34 21) Parker Diana, Callan Laurie et al Nursing Interventions to Reduce the Risk of CatheterAssociated Urinary Tract Infection Part 2: Staff Education, Monitoring, and Care Techniques JWOCN March/April 2009 Copyright © 2009 by the Wound, Ostomy and Continence Nurses Society pages 137-154 22) Potter, Patricia A., Perry Anne Griffin, et al Canadian Fundamentals of Nursing Fourth Edition pages 1096-1113 23) Reilly Laura, Sullivan Patty et al Reducing Foley Catheter Device Days in an Intensive Care Unit AACN Advanced Critical Care Volume 17, Number 3, pp. 272-283 © 2006, AACN References (continued) 24) Roberts James A., MD Kaack M. Bernice, PH.D., Fussell E.N., MS Adherence to Urethral Catheters by Bacteria Causing Nosocomial Infections Urology Volume 41 Number 4 April 1993 pages 338-342 25) Robinson John Clinical skills: how to remove and change a suprapubic catheter British Journal of Nursing 2005 Vol 14, No 1 pages 30-35 26) Siderias J, Guadio F, Singer AJ. Comparison of topical anesthetics and lubricants prior to urethral catheterization in males. Acad Emerg Med. 2004 June;11(6):703-6. 27) Senese Victor, Hendricks Mary Beth, et al Clinical Practice Guidelines. Care of the Patient With an Indwelling Catheter Published: 04/11/2006 http://www.medscape.com/viewarticle/525695_print 28) Smith JoAnn Mercer Indwelling Catheter Management: From Habit-Based to Evidence-Based Practice OstomyWound Management 2003;49(12)34-45 29) Tanabe P, Steinman R, Anderson J, Johnson D, et al. Factors Affecting Pain Scores during Female Urethral Catheterization. Acad Emerg Med. June 2004. Vol11(6) 30) Tanagho Emil A, MD, McAninch Jack W., MD,FACS Smith’s General Urology Seventeenth Edition McGraw Hill Medical, page 293-296 31) Trautner Barbara W Darouiche Rabih O Role of biofilm in catheter-associated urinary tract infection AIIC state of the science report Vol. 32 No 3 pages 177-183 32) Tzortis V, Stavros G, Melekos M. Intraurethral Lubricants: Acritical Literature Review and Recommendations. Journal of Endourology. Vol23; 33) Wein Alan J. Campbell-Walsh Urology Ninth Edition Volume 3 pages 1923-1924 34) Wong, Edward S. M.D. in consultation with Thomas M. Hooton, M.D. Guideline for Prevention of Catheter-associated Urinary Tract Infections CDC Department of Health and Human Services Centers for Disease Control and Prevention Published: February 1981