Pacers, ablation, cardioversion, telemetry, Intro to ACLS
advertisement

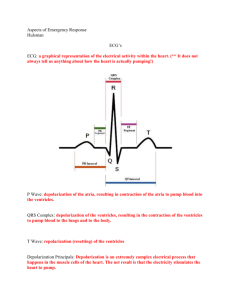
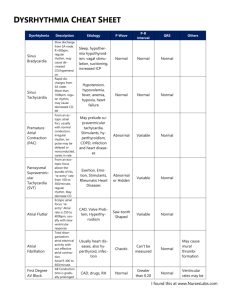
Pacers, ablation, cardioversion, telemetry, Intro to ACLS By: Diana Blum MCC NURS 2140 • A dysrhythmia is a disturbance of the rhythm of the heart caused by a problem in the conduction system. • Categorized by site of origin: atrial , AV nodal, ventricular • Blocks are interruptions in impulse conduction: 1st, 2nd type 1&2, 3rd or complete heart block 2 Each small box measures 0.04 1 big box (5 small boxes) is equal to a HR of 300 2 big boxes is hr of 150 3 big boxes is hr of 100 4 big boxes is hr of 75 5 big boxes is hr of 60 6 big boxes is hr of 50 7 big boxes is hr of 43 8 big boxes is hr of 38 3 Large box estimate of heart rate works with regular rhythms • P-wave = atrial electrical activity • QRS= ventricular electrical activity • T wave= resting phase of ventricle 5 6 P wave Measures: 0.12-0.20 8 QRS WAVE Measures: 0.06-0.10 9 QT Wave Measures approx 0.400.48 secs 10 Heart rates • NSR: heart rate is 60-100bpm • ST: heart rate 101-180 bpm • SB: heart rate <60 bpm 11 Calculating Heart Rate • Quick Estimate: The 6-second Method • - count the # of QRS complexes in a 6 sec. • length of strip & multiply by 10 • (the second mark is = to 5 large boxes) • This can be used is rhythm is reg or unreg. • Count small boxes between two R waves. Divide into1500 Gives BPM Atrial arrythmias • • • • • • • Normal sinus rhythm Sinus tachycardia Sinus bradycardia Premature atrial contraction (PAC) Supraventricular tachycardia Atrial flutter Atrial fibrillation 14 Ventricular arrythmias • • • • • • • • • Junctional rhythm AV blocks Premature junctional rhythm Premature ventricular contraction (PVC) Ventricular Tachycardia (V-tach) Ventricular Fibrillation (V-Fib) Torsade de Pointes (TdP) Pulseless electrical activity (PEA) Asystole 15 ARTIFACT NSR 17 Sinus rhythm • • • • PR interval- 0.12-0.20sec QRS-0.06-0.10sec QT segment 0.36-0.44 sec Heart rate 60-100 18 • Hr= 60-100 bpm • On strip it looks regular but does not map out • PR interval= 0.12-0.20 19 HR 40-60 bpm <60 bpm is accelerated Rhythm is regular Pwaves not always present 20 Junctional Rhythm 21 SB 22 Sinus Bradycardia • All criteria same except rate < 60bpm • S/S: dizziness, syncope, angina, hypotension, sweating, nausea, dyspnea • Sometimes no S/S • Treat underlying cause • IV atropine, pacemaker 23 Sinus Bradycardia: Your pt is pale, c/o dizziness & fatigue. Pulse 56, BP 86/60 • ACLS protocol: • 1. airway • 2. oxygen • 3. ECG, BP, oximetry • 4. IV access • If s/s of poor perfusion: altered mental status, CP, • hypotension, signs of shock • a. prepare for transcutaneous placing • b. atropine 0.5 mg IV while waiting for pacer • - may repeat for total 3 mg IV • c. epinephrine or dopamine drip while waiting pacer or • if pacing ineffective 24 ST 25 Sinus Tachycardia • All criteria same as with NSR except rate >100 • Causes: fever, dehydration, hypovolemia, increased sympathetic nervous system stimulation, stress, exercise, AMI • S/S: Palpations #1, angina and < CO from < V filling time • Treatment: correct cause, eliminate caffeine, nicotine, alcohol. Beta blockers may be ordered 26 Sinus Tachycardia • • • • • Heart rate greater than 100 but less 180 Caused by external influences (fever, blood loss, exercise) Adenosine used B-blockers may cause condition to worsen ( if MI limits vent function the heart will compensate by increasing rate then CO will fall) • Remember to identify and treat cause !!! 27 Supraventricular Tachycardia 28 Supraventricular Tachycardia • • • • • • • • Impulse originates in AV junction or atria Rhythm regular A-fib most common cause Ventricular rate 150-250 QRS normal configuration Symptoms: palpitations, lightheadedness, Loss of Conscious, CP, SOB 29 How to treat SVT • B-blockers ( to decrease conduction thru AV • node: • Calcium channel blockers ( to decrease condux • thru AV node) • Radio frequency ablation 30 31 SVT converted with Adenosine given rapid IV Push stimulates vagal response. S/E: flushing,bronchospasm,AVblock 32 AV Blocks • • • • • First degree block Second degree block Type I (Wenchebach) Second degree block Type II (Mobitz II) Third degree block Bundle branch block 33 Rate is usually WNL Rhythm is regular Pwaves are normal in size and shape The PR interval is prolonged (>0.20 sec) but constant 34 1st degree block • AV node delays the impulse from the SA node for abnormal length of time • Causes: • CAD, MI, drugs that act on AV node (digitalis) • Characteristics: • PR interval >0.20 seconds • Not serious but may progress to 2nd degree 35 1st degree block nursing intervention: • Document the dysrhythmia • Monitor for progression to slower heart rate or worsening block • If progression noted, monitor pt, notify physician 36 Pwaves are normal in size and shape; Some pwaves are not followed by QRS PR interval: lengthens with each cycle until it appears without QRS Complex then the cycle starts over QRS is usually narrow 37 2nd degree AV block:Type I: • AV node delays progression of SA node impulse for longer than normal • Some of the SA impulses never reach ventricles • P waves regular • Progressive lengthening of PR interval until one P wave is not conducted • CAUSE: ischemia or injury to AV node 38 2nd degree Type I AV block: • RISK: often a temporary block after MI • May progress to complete(3rd degree) • block • TREATMENT; freq. none needed • slow vent rate: ATROPINE will increase AV conduction • To increase rate of SA node:EPINEPHRINE 39 2ND degree nursing interventions: Type I • Document • Monitor pt/vitals • If ventricular rate slows enough to produce • symptoms, document , notify physician 40 http://www.youtube.com/watch?v=GVxJJ2 DBPiQ&feature=related Ventricular rate is usually slow Rhythm is irregular Pwaves are normal in size and shape (more pwaves than QRS) PR interval is within normal limits QRS is usually wide 42 2nd degree Type II (Mobitz Type II) • • • • • Atrial rate 60 to 100 More P waves than QRS complexes Ventricular response 2:1 or 3:1 No change in PR intervals of conducted P waves CAUSES: disease of AV node, AV junctional tissue, or His-Purkinje system, inferior MI 43 2nd degree Type II: • RISK: unpredictable & may suddenly advance to complete hrt block • Especially common after inferior infarction • A DANGEROUS WARNING DYSRHYTHMIA • TREATMENT: if vent rate slow, atropine or epinephrine • may need temporary pacer 44 2nd degree Type II Nursing Interventions: • Determine width of QRS • WATCH for widening QRS complex • *width QRS indicates location in the conduction system of the block • - the wider the complex, the lower in the bundle branch system the block will be. • IF QRS WIDENS, NOTIFY PHYSICIAN IMMED. • Prepare for insertion of pacer • Assess vitals 45 Ventricular rate is regular but there is no correlation between pwaves and QRS Pwaves are normal in size and shape No true PR interval 46 3rd degree block: complete heart block: “AV dissociation” • • • • • More atrial waves than ventricular No conduction of atrial impulses Atrial/ventricles beat independently RISKS: bradycardia which produces a decrease in CO leading to hypotension & myocardial ischemia TREATMENT; pacer NURSING INTERVENTION; monitor , hemodynamics , prepare for pacer • 47 Atrial Fibrillation Erratic wavy base Pr is not measurable QRS 0.10 sec or less usually http://www.youtube.com/watch?v=VKxQgjj2yVU&fe ature=related 48 A fib continued • • • • • Atrial rate > 400 bpm with a varying Ventricular rate Overall rhythm irregular No P waves, unable to measure PR interval QRS=normal: Twave undeterminable Causes: Rheumatic fever, mitral valve stenosis, cad. HTN, MI, hyperthyroidism, COPD, CHF see pp. 604 49 A fib continued • Concern with A fib is the development of atrial thrombus and loss of atrial kick from ineffective atrial function. • Treatment: Ca channel blockers and antiarrhythmics to convert, beta blockers to < HR, anticoagulants to prevent embolization. • Synchronized cardioversion 50 Atrial Fibrillation • • • • • • • - - 5 to 6 times more likely to have stroke - - atrial rate: 300 to 600 times/minute --prolonged A-Fib may stretch & weaken heart muscle - - symptoms: lightheaded, very tired, SOB, diaphoretic, chest pain, 51 Afib causes : • Chocolate large amounts: contains theobromine, a mild cardiac stimulant. • - sleep apnea • - athletes more prone (enlarged heart) • - tall athletes (esp basketball players) • - aging heart • - men more than women • - sleeping on left side or stomach • etc. 52 A-fib treatment: • ASA not as effective as Coumadin in preventing strokes. • ASA less likely to cause abnorm bleeding • **since hemorrhagic stroke increases with age & is also increased by taking Coumadin, some Drs. may switch older pts from Coumadin to ASA. 53 A Fib electrical cardioversion: • High risk of forming clots & causing stroke • Anticoagulants taken before treatment and 34 weeks post treatment • If life-threatening, may need Heparin IV before cardioversion • Best time: recent A fib 54 Atrial rate of 250-450 bpm ventricular rate varies Atrial rhythm is regular ventricular rate is irregular No identifiable p waves P wave is not measurable Qrs: 0.10 or less usually 55 Atrial fib/flutter 56 57 Pacer spike should fall before the P wave unless a dual Chamber pacemaker; if it does not there could be a problem 58 PAC 59 PAC: premature atrial contraction • Premature depolarization of atrial origin • P wave may be buried in T wave • A pause follows and SA node will start new cycle of sinus beats • Indicates atrial irritability • No risk if occasional • If 6 or more per minute, indicates atrial tachycardia • Treat: digitalis, calcium channel blockers, beta blockers 60 Extra beat Types uniform=go the same direction multifocal= go in different direction R on T=when the pvc fall on the preceding twave couplet= 2 pvcs together bigeminy= pvc every other beat trigeminy=pvc every third beat 61 PVCs (unifocal) 62 PVCs (multifocal) 63 PVC: ventricular origin • Complex is wide followed by compenatory pause • An irritable focus in ventricle initiates a contraction before normally expected beat. • Acute MI most common cause • QRS is wide and bizarre • Risks: increasing myocardial irritability, leading to increased freq. of PVCs • Can occur as bigeminy (every other beat) • or short runs 64 Ventricular tachycardia Monomorphic: beats are same size and shape Polymorphic: different size and shape 65 V-tach • Advanced irritability of ventricles due to ASHD, CHF, acute MI electrolye imbal. Hypoxia, acidosis,occas drugs • RISKS: low to no Cardiac output • Nursing Interventions: monitor, if pt unconscious,immed. defib 66 This is a polymorphic VT Usually electrical imbalance in nature r/t NA+ or K+ 67 68 Torsade de pointes • Will see prolonged QT interval when in sinus rhythm • Will see prominent U wave • If lasts >10 seconds pt will progress to unconsciousness, life threatening with ineffective cardiac output • TREATMENT: IV magnesium 69 Ventricular Fibrillation Rate can not be determined because of no identifiable waves Rapid chaotic rhythm with no pattern No p waves No PR interval No QRS 70 Vtach/Vfib • • • • • • • Both can be life threatening VT= V HR 100-250 bpm Causes: AMI, CAD, hypokalemia, dig toxic S/S: palpitations, dizzy, angina, <LOC Treatment: assess for pulse, if none, defib VF=Rate undeterminable Cause: same Treatment: CPR 71 V-fib • • • • • • • • • May occur after MI Extensive ventricular irritability Very little cardiac output Death within 4 to 8 minutes TREATMENT: immediate defibrillation immed defib at 200 J if unsuccessful, repeat at 300 J If unsuccessful, repeat at 360 J CPR 72 Asystole 73 Asystole and PEA • CPR Oxygen • Epinephrine 1 mg IV/IO (repeat 3-5 minutes) • May give Vasopressin 40U IV/IO to replace • 1st or 2nd dose of epinephrine • Consider Atropine 1 mg IV/IO Repeat every 3 to 5 min (up to 3 doses) 74 75 What arrthymias are considered PEA? • See an organized or semi-organized rhythm BUT NO PULSE: • This includes: • - idioventricular rhythms • - ventricular escape beats • - postdefibrillation idioventricular • 76 http://www.campaignfornursing.com/events/WINNERS/pennsylvania/ 77 ST elevation 12 lead ekg • The electrocardiogram (EKG) is a device that receives electric impulses from the body and changes them into a monitor tracing that can be analyzed to find problems with electrical conduction in the heart. The EKG simply picks up electrical impulses; it does not read mechanical activity. When a patient has ischemia, injury or necrosis to the heart muscle, the electrical impulses change in the area involved. Nurses can analyze the electrical changes and determine if they indicate mechanical dysfunction. • The EKG is simply a volt meter that picks up electrical signals. Therefore, anything that interferes with electrical conduction can cause changes in the EKG. These variables can be divided into three main categories: – 1) physiological variables not specific to the heart (ie. pulmonary embolism, increased intracranial pressure) – 2) electrical interference (ie. poorly placed lead) – 3) ischemia, injury, or infarction 5 Steps to 12 Lead Interpretation 1. Assess regularity and speed 2. Look for signs of infarction 3. Present in >1 lead, but not all? 4. Assess associated conditions 5. Correlate with clinical condition Normal EKG MI Polymorphic VT VFIB 88 89 90 91 • http://nursebob.com/ • http://www.usfca.edu/fac_staff/ritter/ekg.htm • http://ems-safety.com/12-lead-ekg.htm Rhythms for Cardioversion • A-fib • A-flutter • Supraventricular tachycardia 93 Electrical cardioversion • It is the treatment of choice if the patient has a hemodynamically unstable tachydysrhythmia • It is used for the treatment of unstable ventricular tychardia with a pulse • With cardioversion the potential exists to prevent this life-threatening dysrhythmias. • Cardioversion may either be a planned or emergent procedure. • Properly done cardioversion will correct the patient’s dysrhythemia with minimal discomfort and maximum safety. Chemical cardioversion • • • Indication A. Considered to be an effective alternative to electrical cardioversion for Rapid conversion of atrial fibrillation and atrial flutter. B. Ibutilide is moderately effective in causing prompt conversion to sinus rhythm with greater efficacy in patients who have atrial flutter. 2. Action. A. Ibutilide prolongs action potential duration by activating a slow inward current, largely carried by sodium ions. B. Blocks the rapidly activating component of the delayed rectifier potassium current. C. No significant effect on heart rate, PR interval, or QRS interval D. Potential prolongation by Ibutilide leads to an increase in atrial and ventricular refractoriness in vivo. E. No clinically significant effect of Ibutilide to lower blood pressure or worsen congestive heart failure. F. Route of elimination: hepatic. 3. Administration. A. Ibutilide is available in 10 mL vials containing 0.1 mg/mL (1 mg total). B. For intravenous administration, the recommended dose of Ibutilide is 1mg over a 10 minute period in patients weighing > 60 kg C. Patients weighing < 60 kg, the recommended dose is 0.01 mg/kg initially, with a second dose of the same strength 10 minutes later if necessary. D. Ten minutes after the end of the initial infusion, a second 10 minute infusion of equal strength can be given if the arrhythmia has not terminated. • • • Cautions. A. Prolong ventricular repolarization B. Carries a risk of excessive QT prolongation C. Acquired long-QT syndrome D. Associated polymorphic ventricular tachycardia (torsade de pointes) E. Careful patient selection and clinical monitoring during drug administration. 5. Contraindications. A. QTc interval exceeding 440ms B. Bradycardia C. Electrolyte disturbances D. Other QT-prolonging drugs 6. Adverse Effects. A. Ventricular tachycardia B. Premature ventricular complexes C. Hypotension D. Bundle branch block E. Atrioventricular • Post cardioversion care: • 1. generally the care for a patient tells cardioversion is the same as for the fibrillation. • 2. If it is a elective procedure, digoxin is usually withheld for 48 hours prior to cardioversion to prevent dysrhythmias after the procedure. • 3. Airway patency should be maintained and the patient state of consciousness should be evaluated. Indications for pacemaker • Temporary: • -symptomatic bradycardia (not controlled by meds) • - ant MI • - drug overdose (dig, beta blocker) • Permanent: • - 2nd degree Mobitz Type II • - 3rd degree Block • - symptomatic bradycardia, arrhythmias • - suppress tachyarrythmias 98 Modes of Pacing • Synchronous (demand )Mode • - sensitivity is set to patient beats • - pacer will fir when pt rate goes below • that what is set • Asynchronous pacing: • - for asystole, or profound bradycardia • - does not sense any pt beats • - fires at set rate no matter what pt rate is 99 Position of the letter Designation 1st letter Chamber being paced (A=atrium, V=ventricle, 0=none) 2nd letter Chamber being sensed (A=atrium, V=ventricle, 0=none) 3rd letter Pacing Mode (O=none, I=inhibited, T=triggered, D=dual) 4th letter Rate Response (R=rate response is on) Chambers that can be paced: Atrium Ventricle Dual (both atrium and ventricle) ICD (Implantable Cardioverter Defibrillator) 101 Dual Paced • Atrial Pace, Ventricular Pace (AP/VP) AV AP VP V-A AV AP VP V-A Implant Cardioverter Defibrillator ICD 103 ICD • - prevents sudden cardiac death due to • V-tach or V-fib. • Pt can feel the shock • -defib felt like “kick in the chest” • that lasts 1 second • - cardiovert feels like “thump in chest • - pt doesn’t feel pacing 104 Problems with pacers • Failure to fire • Failure to capture • Undersensing (low battery, poor lead • position) • Oversensing (turn down output, magnetic • interference) 105 Operative failures with pacers: • Pneumothorax • Pericarditis • Infection • Hematoma • Lead dislodgement (seen on X-ray) • Venous thrombosis (rare but would see • unilateral edema to arm on same side • as pacer) 106 Pt Education: • • • • • • • • • • • • • 1. carry ID card (Xray code seen in standard chest Xray) 2. not allowed to drive for 1 month 3. no metal detectors or no longer than nec. 4. MRI interrupts pacing-can’t get one for some time if new 5. No power generators (welding) 6. microwave questionable 7. radiotherapy (may damage circuits) The pacer may need to be surgically moved if in path of radiation field. 8. TENS (transcutaneous electrical stimulation) interferes may need reprogramming 9. Cell phone use in opposite ear of pacer and store away from side of pacer 107 EP with Ablation An electrophysiology study is simply a study of the electrical function of your heart. • • A (IV) catheter may be placed and be used to continuously administer fluids. The purpose of this IV is to provide the nurses and doctors with a quick means of administering medications, should your heart rhythm abnormality occur. An EP team doctor will explain why the procedure is necessary and what risks are involved for you. – – • The degree of risk varies with each person and is related to your specific condition. After discussing this information, a consent form needs to be signed prior to Prior to the EP study, your skin will be washed with a special soap and the hair shaved from potential catheter insertion sites. The most common site used is the groin, or the area at the crease of the leg about midway between the center of your body and your hip. Occasionally the forearm, neck or collarbone areas are used. The purpose of this washing is to provide a clean insertion site and reduce the chance of infection • • • • NPO after midnight the night before the test. If your test is not scheduled until later in the day, may have a clear liquid breakfast, after which you must not eat or drink. You may take your morning pills with a sip of water. All your medicines will be reviewed, and some may be withdrawn prior to the test. You will not receive anything to put you to sleep before this test. It is important for you to describe sensations you have during the test to the staff in the EP laboratory. If you have dentures and they are tight-fitting, you may wear them during the study. You may also wear your glasses and watch if you wish. An initial EP study takes an average of two and a half hours; however, they may range from one to six hours. • • Long, thin, flexible wires, referred to as pacing wires, or intra-cardiac catheters, are advanced through the IV catheter and up into the heart chambers under the guidance of an x-ray camera (see diagram). These pacing wires are used to both record the electrical patterns from inside the heart and to "pace" the heart. Pacing the heart is delivery of very small amounts of electricity to the heart muscle through the tip of the catheter. This causes a heart beat, and allows the electrophysiologist to compare your heart's response to paced beats to already known normal responses. Approximately half of the patients undergoing this procedure are aware of each heart beat, and therefore, feel their heart speed up, slow down, or "skip a beat". Many other people are completely unaware of the pacing procedure. If an arrhythmia is provoked by the pacing, you may feel some of the same symptoms that caused you to seek medical attention. Please tell the EP staff what you feel. Let them know if you have shortness of breath, dizziness, light-headedness, or chest discomfort. A member of the team will be by your side and talking with you at all times. • • • • • After the test, the catheters will be removed. Firm pressure will be applied over the puncture site for approximately 15 minutes. This is necessary to prevent any bleeding from the insertion site. You will then be taken to your hospital room, or the EP recovery area. Flat bed rest is necessary for two to eight hours after the study. During this time, it is important to keep the leg or arm used in the procedure straight to prevent bleeding from the insertion site. After the specified amount of rest, you will be able to resume your previous activity level. Your nurse will be in the room frequently during the first hour after the study to take your blood pressure, heart rate, and check your insertion site for signs of bleeding. The pulses and temperature of your feet will also be checked. You will be instructed to apply pressure firmly to the insertion site if you cough or sneeze and while using the bedpan or urinal. If you should notice any bleeding at the site, notify your nurse immediately. If your back becomes uncomfortable, do not hesitate to ask the nurses for pain medications. You will be able to resume your previous diet and your nurse or family members can help you eat while you are reclining in bed. Bundle Branch Blocks: Diagnosed with 12 lead EKG: most common cause: acute MI • Right bundle branch block: • - impulse travels through left ventricle first, then activates right ventricle (gives am “M” shaped complex • Left bundle branch block: • --impulse first depolarizes right side of heart then the left ventricle (gives deep, wide “V” shaped complex 113 Bundle Branch Blocks: • Risks: can deteriorate to 3rd degree block • then treat with atropine or pacemaker • Pt can be asymptomatic until progresses 114 115 Hyperkalcemia 116 Intro to ACLS Primary Survey • Airway: Open airway, look, listen, and feel for breathing • Breathing: If not breathing slowly give 2 rescue breaths. If breaths go in continue to next step. • Circulation: Check the carotid artery (Adult) for a pulse. If no pulse begin CPR. • Defibrillation: Search for and Shock VFib/Pulseless V-Tach Adult ACLS Secondary Survey ABCDs (abbreviated) • Airway: Intubate if not breathing. Assess bilateral breath sounds for proper tube . placement. • Breathing: Provide positive pressure ventilations with 100% O2. • Circulation: If no pulse continue CPR, obtain IV access, give proper medications. • Differential Diagnosis: Attempt to identify treatable causes for the problem. AED • An AED is a device used in cardiac arrest, or sudden cardiac death, when the heart’s electrical activity is disorganized and there is no effective pumping of blood. The AED is capable of recognizing the heart's electrical activity, and determining if an electric shock is required. If the shock is needed, a voice prompt in the AED is activated, telling the rescuer to push a button to deliver the shock • http://acls.net/quiz/mi_stroke_1.htm stress • Common responses can include: – Feeling a sense of loss, sadness, frustration, helplessness, or emotional numbness – Experiencing troubling memories from that day – Having nightmares or difficulty falling or staying asleep – Having no desire for food or a loss of appetite – Having difficulty concentrating – Feeling nervous or on edge Teaching to cope • • • • • • Reach out and talk. Express yourself. Watch and listen. Stay active. Stay in touch with family. Take care of yourself. ANY QUESTIONS???