Assessment of Oxygenation
advertisement

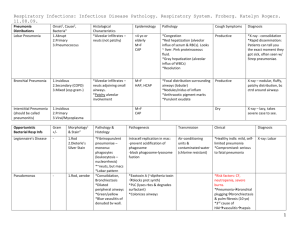
Assessment of Oxygenation Subjective Data Past History – Upper resp infections – Lower resp problems (asthma, TB, pneumonia, COPD) – Related illness that affect resp system – AIDS, CHF – Immunizations, TB skin tests, CXRs – Allergies – Medications Subjective Data Family History – Focus on resp illnesses Personal and social history – Occupational history Factory, chemical plants, coal mines, farming, heavy traffic are all high risk for respiratory system – Smoking history How long? How much? (pk yrs = # pks/day X # years) – Substance abuse ETOH – risk for aspiration pneumonia IV drugs and AIDS risk for pnuemonia – Activity Tolerance SOB or fatigue with daily activities? How far/fast can you walk? Subjective Data Specific Symptoms – Cough How long? Onset (gradual, sudden); When (a.m., all day?) How often? Productive? How much? Color (yellow/green – bacteria; frothy pink – pulmonary edema) Odor? Blood? Subjective Data Specific Symptoms – Shortness of breath (SOB) Precipitating factors, severity, duration Effect of position (lying down? Upright?) Association with other symptoms (chest pain, cough) What makes it better/worse (rest, oxygen, inhalers, meds) Effect on activities? – Chest pain PQRST (does breathing affect the pain?) Objective Data Mouth, nose, pharynx, neck, heart Lungs and thorax Objective Data: Inspection Note position (upright, leaning on table?) Evidence of respiratory distress/quality of respirations Nasal flaring, accessory muscles, intercostal retraction or bulging Shape and symmetry of chest Normal AP:transverse ratio is 1:2 – 5:7 Barrel chest: increased AP diameter in relation to transverse Objective Data: Inspection Respiratory rate (N = 12 – 20) Respiratory pattern Tachypnea – rapid, shallow, > 24/min Bradypnea – slow (< 10/min) Hyperventilation – increased rate and depth Hypoventilation – shallow Cheyne-Stokes Objective Data: Inspection Skin color – Cyanosis (indicative of deoxygenated blood) Nails – Clubbing (increased angle between base of nail and fingernail to 180 degrees or more – Usually accompanied by increased depth, bulk and sponginess of end of fingers Objective Data: Palpation Symmetric expansion Tactile fremitus Palpable vibration generated by vocal cords “99” Using palmar base of fingers, palpate from side to side Increased when lung is fluid-filled/more dense Decreased when lung is farther from hand or if hyper-inflated Absent over areas of collapse (pneumothorax, atelectasis) Objective Data: Percussion To assess density or aeration Dull over areas of consolidation (e.g. pneumonia) Hyper-resonance over areas of hyperinflation (e.g. asthma, COPD) Objective Data: Auscultation Normal breath sounds Vesicular – Soft, low pitch, gentle rustling – Heard over peripheral lungs Bronchial – Loudest, high pitch, like air through hollow pipe – Over trachea and larynx Bronchovesicular – – – – Medium pitch and louness Mix of above qualities Anteriorly – over bronchi, either side of sternum Posteriorly – between scapula Objective Data: Auscultation Abnormal/adventitious breath sounds – Discontinuous sounds Crackles (fine) Crackles (coarse) Pleural friction rub – Continuous sounds Rhonchi Wheeze Stridor Objective Data: Auscultation Discontinuous sounds – Crackles (fine) Short, crackling, popping sound at end-inspiration When collapsed alveoli or bronchioles snap open Associated with pneumonia, early pulmonary edema, atelectasis – Crackles (coarse) Short, low-pitched bubbling sounds, mostly during inspiration Caused by air passing through airway that is intermittently occluded with secretions in larger airways Associated with pnuemonia, pulmonary edema – Pleural friction rub Creaking, grating sound (like leather being rubbed together) During inspiration and/or expiration Due to inflamed pleural surfaces rubbing together Associated with pleurisy, pneumonia Objective Data: Auscultation Continuous sounds – Rhonchi Low pitch, snoring, moaning sound mostly on expiration Air passing through large airways with secretions COPD, pneumonia – Wheeze High pitched squeaking sound, mostly on expiration Sometimes audible without stethescope Caused by air passing through narrowed airways (d/t spasm, swelling, tumors, secretions) – Stridor High pitch crowing sound; often audible without stethescope Caused by partial obstruction of larynx or trachea Associated with croup, epiglottitis, laryngeal edema or spasm (post extubation) Diagnostic Tests Sputum studies – – – – C&S Gram stain (classifies as gram + ve or – ve) AFB (acid fast bacilli) – for TB Cytology – examination for abnormal cells Bronchoscopy – Bronchi visualized with fiberoptic tube inserted through nose into airways – Can take biopsy, remove foreign bodies, mucus plugs – NPO and sedation pre-test – Post procedure: NPO until gag returns; assess for laryngeal edema,, hemorrhage (if bx taken), recovery from sedation Diagnostic Tests Pulmonary Function tests – Measures lung volumes and airflow Arterial blood gases (ABGs)