Laboratory Values
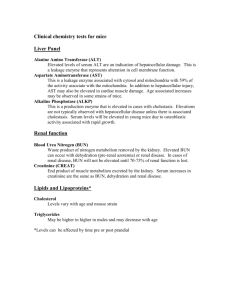
advertisement

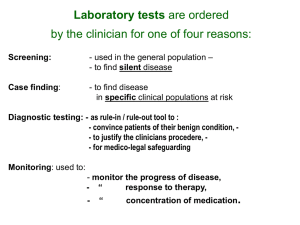
Laboratory Tests The central theme of the General Medicine course is as follows: Systemic diseases cause alterations in normal physiology and function. These alterations complicate the diagnosis and treatment of dental problems. Clinicians need to identify and classify systemic disorders and appropriately modify diagnosis and treatment planning in order to avoid systemic complications. Diagnosis is based on: previous history, medication lists, symptoms, clinical signs, clinical tests such as radiographs and laboratory data. To fully appreciate laboratory data as a diagnostic tool, one must have an understanding of: Organ systems: cardiovascular, respiratory, renal, hepatic, etc. Anatomy and physiology Disease states and classification Diagnosis and treatment including pharmacology Example: Diabetes mellitus Organ: endocrine pancreas Anatomy: endocrine gland (alpha cells: glucagon, beta cells: insulin), secretes directly into the systemic circulation Physiology: glucose is regulated within a relatively narrow range (in part) by the effects of insulin which drives the uptake of glucose into cells and glucagon which stimulates the production of glucose through the metabolism of glycogen and release of the glucose into the blood Disease: diabetes (Type I or II) as a result of loss of pancreatic insulin production or systemic cellular sensitivity leading to a build up of serum glucose. There is an inability of cells to take up glucose and a resulting “cellular starvation” leading to alternate metabolic pathways (ketoacidosis). Treatment: diet and exercise management, oral hypoglycemics or insulin Test: Measurement of serum glucose gives the clinician insight into the presence or absence of disease, its severity, patient compliance and control. As we progress through the course, a number of lab values will come up as important markers of organ function, dysfunction or treatment. This list is not meant to be exhaustive. It is intended to be a reference for the more commonly used (and therefore important) ones. Commonly ordered tests: CBC (complete blood count) offers insight into the function of the haematopoeitic system … the production of hemoglobin, red blood cells, white blood cells and platelets. Hemoglobin male female male female 135 - 170 g/L 115 - 160 g/L Hematocrit 0.40 - 0.51 0.34 - 0.48 RBCs 4.50 - 6.00 x 1012/L RBC indices are useful to the hematologist in diagnosing a patient’s anemia, for example iron deficiency vs. pernicious anemia eg. MCV (mean corpuscular volume), MCH (mean corpuscular hemoglobin), MCHC (mean corpuscular hemoglobin concentration) WBCs 4.0 - 10.0 x 109/L WBC differential (neutrophils, lymphocytes, monocytes, eosinophils, basophils) Platelets 150 - 400 x 109/L Disturbances to hemoglobin include anemia due to iron or other deficiency, bleeding or marrow suppression such as chemotherapy. WBC increases are due to steroid use, infection or leukemia, decrease due to marrow suppression. Platelet decreases are due to increased consumption (ITP or spenlomegaly), or decreased production due to marrow suppression. Coagulation Studies INR (International normalized ratio 0.9 - 1.1 of PT or prothrombin time) Therapeutic coumadin 2.0 - 3.0 Mechanical heart valves 2.5 - 3.5 PTT (partial thromboplastin time) 21 - 33 seconds Therapeutic heparin 60 - 85 seconds INR and PTT may be elevated due to loss of factor production in liver disease, due to congenital deficiency such as hemophilia, or suppression with drugs such as coumadin or heparin. Renal function Electrolytes … the common ions that are important in serum Sodium 135 - 145 mmol/L Potassium 3.5 - 5.5 mmol/L Chloride 98 - 107 mmol/L Bicarbonate 24 - 32 mmol/L Electrolyte disturbances may be due to renal failure, alterations in hydration (hypo or hyper), drug use (diuretics), alterations in pH (acidosis or alkalosis), diabetic ketoacidosis, adrenal disease, etc. Renal function tests (more specific) BUN (blood urea nitrogen) 2.5-8.0 mmol/L Creatinine 60-125 umol/L (from which is calculated creatinine clearance) Renal failure (and increasing BUN and creatinine) may be due to acute tubular necrosis (due to hypotension), glomerulonephritis, diabetic nephropathy, urinary tract infection, etc. Liver function Albumin Bilirubin AST (aspartate aminotransferase) ALT (alanine aminotransferase) 35 - 50 3.4 - 17.1 10 - 42 10 - 40 g/L umol/l U/L U/L In liver failure (due to hepatitis or cirrhosis) serum albumin will be decreased due to reduced production, serum bilirubin will be increased due to loss of liver metabolic function, serum enzymes will be increased due to “leakage” of contents of damaged cells. Respiratory function ABGs (arterial blood gases) ph PO2 PCO2 7.35 - 7.45 70 - 104 mm Hg 35 - 45 PFTs (pulmonary function tests) FEV1 (forced expiratory volume in one second / percent of predicted based on total forced expiratory volume) Normal moderate disease >70% 40 to 60 % mild disease severe disease < 60% <40% Endocrine function Calcium 2.12 - 2.62 mmol/L Calcium levels will be reduced with dietary Vitamin D or calcium deficiency, loss of parathyroid function (for example post thyroid surgery), etc. TSH Suppressed Elevated 0.35 - 5.00 < 0.10 > 15.0 mIU/L mIU/L mIU/L TSH is elevated in hypothyroidism due to primary thyroid deficiency disease. TSH is depressed with excess exogenous thyroid hormone, Grave’s disease or a secreting thyroid adenoma Glucose (random) 3.6 - 11.0 mmol/L Glucose (fasting) 3.9 - 6.1 mmol/L Glycated hemoglobin (long term (3 month) measure of diabetic control) Normal 4.0 - 6.0 % Good <7.0 % Fair 7.0 to 8.9 % Poor >9.0 % Increased serum glucose may be related to either undiagnosed diabetes, or poorly controlled diabetes due to non-compliance or the “brittleness” of the underlying disease. Decrease serum glucose is typically due to insulin overdose or inadequate dietary intake of calories in the face of insulin or oral hypoglycemic use HIV studies CD4 count essentially normal immunity Mild Moderate Severe End Stage >400 301 – 400 201 – 300 101 – 200 0 – 100 x 106/L x 106/L x 106/L x 106/L x 106/L