Analgesia for Labor and Vaginal Delivery
advertisement

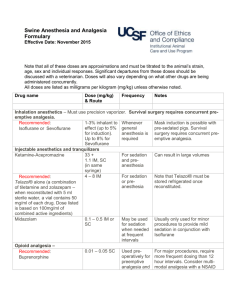
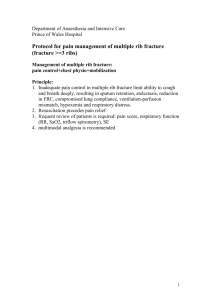
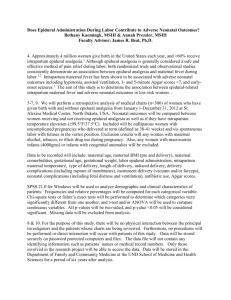
Analgesia for Labor and Vaginal Delivery Hirmanpour A . MD Pain perception by the parturient is a dynamic process that involves both peripheral and central mechanisms. On the McGill pain questionnaire, labor pain is one of the most intense pains that a woman can experience, and it is typically worse than a toothache, backpain, and pain associated with a deep laceration. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Psychoprophylaxis “Natural childbirth” stems from a phrase coined by Grantley Dick-Read in 1933; He believed that childbirth was a painless process that did not need medical intervention. He opined that the pain of childbirth results from a ‘‘feartension-pain-syndrome.’’ Fernand Lamaze introduced the Western world to psychoprophylaxis. “natural childbirth” was popularized after Marjorie Karmel described and published her childbirth experience under the care of Dr. Lamaze. (Lamaze method) American society for Psychoprophylaxis was born. Karmel M. Thank You, Dr. Lamaze: A Mother’s Experiences in Painless Childbirth. 2nd edition. New York, Harper & Row, 1981. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Transcutaneous Electrical Nerve Stimulation TENS is thought to reduce pain by nociceptive inhibition at a presynaptic level in the dorsal horn by limiting central transmission. TENS involves the transmission of low-voltage electrical current to the skin via surface electrodes. It is most widely used for childbirth in Scandinavia and the United Kingdom. Transcutaneous Electrical Nerve Stimulation A systematic review of eight trials in more than 700 women concluded that evidence for TENS-mediated reduction in pain during labor is weak. Carroll D, Tramer M, McQuay H, et al. Transcutaneous electrical nerve stimulation in labour pain: A systematic review. Br J Obstet Gynaecol 1997; 104:169-75. Transcutaneous Electrical Nerve Stimulation Electrical stimulation activates low-threshold myelinated nerves. Inhibit unmyelinated small c fibers by blocking impulses to target cells in the substantia gelatinosa of the dorsal horn. TENS is also thought to enhance release of endorphins and dynorphins centrally. Placement of electrodepads over the lower back region in the distribution of T10-L1 may provide some analgesia for parturients in early labor. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Systemic Medication Opioids are the most commonly used class of drugs Sedative – transqualizer Meperidine Meperidine is the most commonly used parenteral opioid analgesic during labor. IM : 50 to 100 mg( peak onset of effect at 40 to 50 minutes); IV : 25 to 50 mg ( 5 to 10 minutes). The analgesic effect lasts up to 3 to 4 hours. Fetal exposure to meperidine is highest between 2 and 3 hours after maternal administration. Meperidine Cause less respiratory depression in the neonate than morphine does; So, it is more commonly used. It may cause loss of beat-to-beat variability of FHR tracings. A meta-analysis failed to prove that other opioids(tramadol, meptazinol, diamorphine, pentazocine, nalbuphine,and butorphanol) were superior to meperidine for labor analgesia. Some investigators have proposed fentanyl and remifentanil as superior choices. Meperidine Metabolized in the liver to produce normeperidine, Normeperidine Pharmacologically active metabolite A potent respiratory depressant Crosses the placenta. Half-life of 60 hours in the neonate. Fentanyl An alternative analgesic option For patients in whom neuraxial anesthesia is contraindicated. Its short half-life makes it suitable for prolonged use in labor, Use as an IV bolus or as an analgesic administered by means of a PCA delivery system. Provides reasonable levels of analgesia with minimal neonatal depression. Fentanyl The usual dose : 25 to 50 µg (IV). The peak effect occurs within 3 to 5 minutes and has a duration of 30 to 60. Eisele found IV fentanyl 1 µg/kg provided good analgesia with no appreciable hemodynamic effect and no adverse effects on Apgar scores, fetal acidbase status, or neurobehavioral scores at 2 and 24 hours. Fentanyl Another advantage: Can be administered in non parenteral modalities, Subcutaneously-Orally- Patch. These uses, have not been adequately evaluated in laboring patients. Butorphanol and Nalbuphine Opioid agonist-antagonists Structurally related to oxymorphone and naloxone. The potential advantages of producing less nausea and vomiting Butorphanol Is a κ-agonist and a µ-antagonist Minimal affinity for σ-receptors. Dose : 1 to 2 mg IM or IV Duration of action up to 4 hours. Nalbuphine Is a partial κ-agonist and a potent µ-antagonist Minimal σ-receptor activity. A dose of 10 mg IM or IV is equivalent to 10 mg of morphine IV : Onset 2 to 3 minutes IM: Onset 10 to 15 minutes It can offer analgesia for up to 6 hours. One advantage of these agents over µ-agonists They demonstrate a “ceiling effect” By increasing doses do not produce further respiratory depression. Unfortunately, The use of these drugs is limited in clinical practice Because of rapidly transferred across the placenta and have produced ominous sinusoidal FHR patterns. The use of antagonists or agonist-antagonists may precipitate acute withdrawal syndrome in the mother and the newborn of an opioid-dependent parturient. This syndrome has been reported after parenteral or neuraxial routes of administration. Naloxone There is no neonatal benefit to the maternal administration of naloxone during labor or just before delivery. Naloxone reverses opioid depression of newborn minute ventilation and increases the slope of the CO2-response curve in infants affected by the maternal administration of an opioid. The recommended dose is 0.1 mg/kg of a 1 mg/mL or 0.4 mg/mL solution. Not recommended during the primary steps of neonatal resuscitation, Naloxone Only use if respiratory depression continues and after PPV, normal heart rate and color of neonate appears (In mother received an opioid within the previous 4 hours). Preferred route of administration is intravenous. If IV access is not available, IM administration is acceptable, although absorption may be delayed. Endotracheal administration of naloxone is not recommended. Remifentanil A potent, short-acting µ-opioid receptor agonist Approved for clinical use in the US since1996. Contains an ester linkage that allows metabolism by nonspecific esterases throughout the blood and muscles. This metabolism gives it a unique pharmacologic profile in comparison to other opioids. Remifentanil has an extremely rapid plasma clearance and offset of action. Half life : 1.3 mins Remifentanil Prolonged administration does not cause accumulation of this drug. UV/M= 0.88. Fetal exposure to the drug is minimized because of its rapid metabolism or redistribution, or both. An attractive alternative systemic analgesic in parturients in whom regional anesthesia is contraindicated. Remifentanil PCA with IV remifentanil : Bolus dose of 0.4 µg/kg with a lockout time of 1 minute Continuous infusion of remifentanil at 0.05 µg/kg/min with a bolus of 25 µg and a lockout time of 5 minutes provides satisfactory labor analgesia. Systemic Medication Opioids are the most commonly used class of drugs Sedative – transqualizer Sedative-Tranquilizers used for sedation,anxiolysis, or both during early labor and before cesarean delivery. Barbiturates Phenothiazines Hydroxyzine Benzodiazepines Secobarbital were once popular, they are currently unfashionable because of antianalgesic effects in the mother and prolonged depressant effects inthe neonate. Even with small doses of barbiturates that result in no depression of the Apgar score, the newborn’s attention span may be depressed for more than 4 days. Promethazine The most commonly phenothiazine used in obstetrics. Used with meperidine Doses : 25 to 50 mg to prevent emesis. Promethazine appears in fetal blood within 1 to 2 minutes after IV injection in the mother and reaches equilibrium within 15minutes. Ketamine N-methyl-d-aspartate (NMDA) receptor antagonist Produces dissociative anesthesia Its mechanism: With phencyclidine receptors located in the limbic and corticothalamic areas of the brain. Subanesthetic doses: 0.5 to 1 mg/kg or 10 mg every 2 to 5 minutes to a total of 1 mg/kg in 30 minutes during labor. ketamine In addition to its use in labor….. Ketamine in dose of 25 to 50 mg can be used to supplement an incomplete neuraxial blockade for C/S. Its main disadvantages are the potential for hypertension and emergence reactions. High doses (>2 mg/kg)can produce psychomimetic effects and increased uterine tone, which may cause low Apgar scores and abnormalities in neonatal muscle tone. Benzodiazepines can be used as sedatives and anxiolytics in labor. Diazepam (Valium), Lorazepam(Ativan), Midazolam (Versed), Disadvantages: cross the placenta, with elimination halflives as long as 48 hours for diazepam and upward of 120 hours for its main metabolite N-desmethyldiazepam. Exposure to BNZ early in utero may result in malformations such as cleft lip. Benzodiazepines Use of BNZ during labor no effect on fetal malformations, But may be with other problems in the neonate: Sedation Hypotonia Cyanosis Impaired metabolic responses to stress. BNZ are potent amnestic agents, a parturient may not be able to remember her birthing experience. Many of the adverse effects can be reversed by flumazenil, which is a competitive benzodiazepine receptor antagonist. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Inhalational techniques Definition : administration of subanesthetic concentrations of inhaled anesthetics to relieve pain during labor. This pain relief technique should not be confused with inhaled anesthesia that produces unconsciousness and loss of protective laryngeal reflexes. Although inhaled analgesia provides a limited amount of pain relief, it is not adequate to provide sufficient pain relief for most mothers. Inhalational techniques Inhaled analgesics can be administered either intermittently (during contractions) or continuously. They can be self-administered, but the patient should have a health care provider present to ensure an adequate level of consciousness and proper use of the equipment. Inhalational techniques Entonox (50 : 50 N2O/O2 mixture) has been used for many years as both a sole analgesic and an adjuvant to systemic and regional techniques for labor. Side effects include dizziness, nausea, dysphoria, and lack of cooperation. The maximum analgesic effect : after 45 to 60 seconds, Should use in early onset of contractions and discontinue its use after the peak of the contraction. Entonox Inhalational techniques Inhalational techniques The lack of scavenging systems in labor may theoretically put staff at risk of exposure to excessive levels in prolonged period. The administration of N2O and O2 in a 50 : 50 combination appears to have no effect on hepatic, renal, cardiac, or pulmonary functions. A recent meta-analysis by Kronberg and Thompson concludes that inhaled N2O relieves labor pain to a significant degree in most patients but does not provide complete analgesia for many. The analgesic effect of N2O is dose dependent, which supports its analgesic efficacy during labor. Inhalational techniques Desflurane (0.2%), enflurane, and isoflurane (0.2% -0.25%) sevoflurane (0.8%)as an effective labor analgesic. Sevoflurane, when compared with Entonox, provided superior pain relief but more intense sedation, without adverse effects and which was acceptable to mothers. The use of these volatile analgesics is limited by drowsiness, unpleasant smell, and high cost. The major risk with VA : Accidental overdose Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Regional Analgesia The ideal labor analgesic technique Safe for both the mother and the baby, Does not interfere with the progress of labor and delivery Provides flexibility in response to changing conditions. Techniques of Noraxial Analgesia Epidural, Spinal, Combined spinal-epidural blocks. Patient Evaluation and Preparation Medical and obstetric history, Clinical examination Evaluating the airway. Use of herbal medications A 7.1%incidence of herbal use by parturients after 20 weeks’gestation has been reported. Garlic , Ginkgo, Ginseng, Ginger may have anesthetic implications. The anesthesiologist should explain the procedure and the potential complications of the technique. Neuraxial blocks A full check of emergency equipment should be performed to ensure the immediate availability of resuscitative drugs and equipment. An intravenous infusion should be started, and appropriate maternal and fetal monitoring should be in place before starting the procedure. Epidural Analgesia Low doses of LA or opioid combinations are administered(usually by infusion) to provide a continuous T10-L1 sensory block during the first stage of labor. Further supplementation maybe required during the late first stage and second stage to achieve a sacral block. Laber is divided into three stages: The first stage----has two phases: 1- Latent phase ( is defined as the period between the onset of labor and the point at which a change in cervical dilatation is noted) and Phase of maximal dilatation(which usually begins at approximately 3-cm dilation). 2- Active phase of labor, uterine contractions occur approximately every 3 minutes, have a duration of about 1 minute. The second satage----- interval between full cervical dilation and delivery of the infant. The third stage ------- delivery of the placenta. During the first stage of labor, visceral pain impulses entering the spinal cord at T10 to L1 must be blocked. During the second stage of labor, somatic impulses entering the spinal cord fromS2 to S4 must also be blocked . T10 & L1, lower part of the back and perineum and the upper part of the legs. T11 & T 12 T10 & L1 perineum Figure 69-7 Distribution and intensity of labor pain during each stage of labor and delivery. First stage of labour Epidural Analgesia The benefits: Effective pain relief without appreciable motor block, Reduction in maternal catecholamines Decreased α & β adrenergic receptor stimulation Result in better uteroplacental perfusion and more effective uterine activity. Influence of epidural analgesia on maternal plasma concentrations of catecholamines during labor. *P < .05 comparedwith before epidural.Shnider SM, Abboud TK, Artal R,et al. Maternal catecholamines decrease during labor after lumbar epidural anesthesia. Am J Obstet Gynecol 1983; 147:13-5.) contraindications Patient refusal Overt maternal coagulopathy Frank infection at the needle site Maternal hemodynamic instability High-risk conditions, such as fixed cardiac output states (critical aortic stenosis), Must be considered on a case-by-case basis, with riskbenefit analysis for each patient. Epidural Analgesia The use of ultrasound is increasing . Ultrasound imaging of the lumbar spine can aid identification of necessary landmarks for epidural placement and estimate the depth of the epidural space in the pregnant patient . It may be especially beneficial in the obese parturient or in patients known to have previous difficult epidural placement. In a survey of 1000 consecutive women who chose a variety of analgesic techniques for labor and vaginal delivery(including nonpharmacologic methods, transcutaneouselectrical nerve stimulation, intramuscular meperidine,inhalation of nitrous oxide, epidural analgesia, and a combination of these techniques), pain relief and overall satisfaction with the birth experience were greater in patients who received epidural analgesia. Paech MJ. The King Edward Memorial Hospital 1,000 mother survey of methods of pain relief in labour. Anaesth Intensive Care 1991; 19:393-9. Epidural Test Dose Contravertial for the use of epinephrine. Epinephrine produces a reliable increase in HR when the epidural has been sited in a blood vessel. In laboring patient, maternal HR variability from the pain of uterine contractions may confuse interpretation of the heart rate response, and intravenous epinephrine may have deleterious effects on uterine blood flow. Epidural Test Dose The lack of sensitivity and specificity of the test dose calls into question its usefulness as a diagnostic tool. Leighton ----- injection of 1 to 2 mL of air into the epidural catheter while listening over the precordium with the maternal external Doppler monitor for evidence of air. If continuous infusion of dilute LA is administered and the patient remains comfortable, without a motor block, proper epidural catheter placement is ensured. That is, after several hours, if the epidural catheter were intravascular the patient should have inadequate pain relief, and if the catheter were subarachnoid, a solid motor block would develop. The safe practice of administering labor epidural analgesia dictates Initial catheter aspiration, Incremental injections, Continuous monitoring for evidence of local anesthetic toxicity. Spinal Analgesia Provides effective and rapid onset of labor analgesia In very early labor In a distressed parturient to enable epidural placement under more controlled conditions. For instrumental deliveries in women who do not have an indwelling epidural catheter. For routine labor analgesia in some hospitals. (No flexibility of catheter) Continuous spinal analgesia with a “macrocatheter” • • • Indications: Considered in cases of accidental dural puncture Very high-risk parturients Provides excellent analgesia and the assurance of a spinal catheter. Reduce the incidence of post–dural puncture headache (PDPH)after an accidental dural puncture with an epidural needle. Inform all personnel involved in the care of a parturient with a spinal catheter in place to avoid accidental over dose of LA. Continuous spinal analgesia with a “microcatheter” Introduced into clinical practice in the late 1980s Quickly gained popularity Convenience, Fast onset, Potential for decreased risk of PDPH. Reports of cauda equina syndrome associated with their use for C/S led the FDA to withdraw these microcatheters from clinical practice. Explanations for the occurrence of cauda equina syndrome Possible inadequate mixing of local anesthetic within the intrathecal space The use of high concentrations of potentially neurotoxic local anesthetic (5% lidocaine) that can result in neural damage. Combined Spinal-Epidural Analgesia Effective, Rapid-onset analgesia with minimal risk of toxicity or impaired motor block. The ability to prolong the duration of analgesia, If operative delivery becomes necessary, the catheter can be used to provide operative anesthesia. Made ambulation possible with minimal motor block so termed “the walking epidural.” Methods of CSE (1) Epidural catheter insertion followed by spinal needle placement at a lower interspace; (2) An epidural needle beside the spinal needle at the same interspace with the use of specially designed needles; (3) The most commonly used “needle-through-needle” technique, Combined Spinal-Epidural Analgesia Set The epidural needle is sited in the epidural space. The long spinal needle is passed through the epidural needle and punctures the dura mater. After removal of the spinal needle stylet CSF is seen spontaneously dripping from the spinal needle. Combined Spinal-Epidural spinal needle Spinal fluid coming from spinal needle Slide 82 courtesy of Alex Pue, MD epidural needle The spinal needle is withdrawn, and the epidural catheter is threaded through the epidural needle into the epidural space Advantages of CSE versus Epidural analgesia No incomplete(patchy) blockade, No motor block, No poor sacral spread. Significantly reduced duration of the first stage of labor in primiparous parturients. The original description of spinal labor analgesia involved sufentanil or fentanyl. The addition of isobaric bupivacaine to the opioid produces a greater density of sensory blockade while still minimizing motor blockade. Originally,25 µg of fentanyl or 10 µg of sufentanil was advocated, Later studies have suggested using smaller doses of opioid combined with a local anesthetic. Many clinicians are now routinely using 5 µg of sufentanil or 15 µg of intrathecal fentanyl. Other studies have suggested that ropivacaine and levobupivacaine can be substituted for intrathecal bupivacaine to provide labor analgesia. Side effects of intrathecal opioid Pruritus, Nausea and vomiting, Urinary retention. Respiratory depression as a result of cephalad spread of opioid is rare but has occurred when using lipidsoluble opioids. Pruritus Unrelated to histamine release Pruritus is mediated through central µ-opioid receptor Antagonizing central inhibitory neurotransmitters (e.g., gamma-aminobutyric acid [GABA] and glycine) Interaction with central 5-HT3 receptors. These receptors are concentrated in areas of the CNS with high µ-opioid receptor density (e.g., trigeminal nerve nucleus and dorsal horn of the spinal cord). 1- Waxler B, Dadabhoy ZP, Stojiljkovic L, Rabito SF. Primer of postoperative pruritus for anesthesiologists. Anesthesiology 2005; 103:168-78. 2- Ganesh A, Maxwell LG. Pathophysiology and management of opioid- induced pruritus. Drugs 2007; 67:2323-33. Treatment of pruritus The most effective treatment is a centrally acting µ-opioid antagonist (e.g., naloxone or naltrexone) or a partial agonistantagonist such as nalbuphine (Table 23-8). Antihistamines(e.g., diphenhydramine) are usually ineffective because the mechanism of pruritus is not related to histamine release. Ondansetron (8-16mg) Subhypnotic doses of propofol (10- 20 mg) Warwick JP, Kearns CF, Scott WE. The effect of subhypnotic doses of propofol on the incidence of pruritus after intrathecal morphine for caesarean section. Anaesthesia 1997; 52:270-5. Use of a continuous epidural infusion of dilute local anesthetic plus opioid (e.g.,0.0625% to 0.1% bupivacaine) provides sensory analgesia without motor block; Before ambulation, however, women should be observed for the preceding 30 minutes to ensure maternal and fetal well-being, and they should be assessed for adequate motor function. An increased frequency of FHR tracings and fetal bradycardia occurs with CSE. fetal bradycardia is usually short in duration and typically resolves within 5 to 8 minutes. Etiology of fetal bradycardia after CSE (may be related to) : Acute reduction in circulating maternal catecholamine levels after the quick onset of analgesia. Imbalance between epinephrine/norepinephrine levels causes α-adrenoceptor effects on uterine tone and decreases uterine blood flow.(controversy) Continuous Epidural Infusion Most obstetric anesthesiologists now advocate the use of continuous infusions of dilute LA solutions. Local anesthetics such as bupivacaine, ropivacaine, and levobupivacaine in concentrations ranging from 0.0625% to 0.125% ± opioid. The addition of epinephrine enhance the quality of the analgesia by: 1) Reducing vascular uptake and systemic absorption of LA 2) Direct agonist effect on α2 spinal receptors. Patient-controlled epidural analgesia (PCEA) Effective labor analgesia and excellent patient satisfaction. It reduces total amount of LA used; so lessens unwanted effects such as motor block and hypotension. It reduces the demands on staff on the labor floor, The catheter is connected to the PCEA device and the patient can then self-administer further boluses as required. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Lumbar Sympathetic Blocks Another nerve block as an alternative to central neuraxial blocks Block transmission of pain from the uterus during the first stage of labor. It is a technically difficult block to perform, it appears to be associated with fewer complications than paracervical blockade. Labor analgesia options are: Psychoprophylaxis Transcutaneous electrical nerve stimulation(TENS) Systemic medication Inhalational techniques Neuraxial blocks Lumbar sympathic block Paracervical and pudendal block(infrequently) Paracervical and Pudendal Blocks For who does not want or cannot receive a neuraxial block. LA is injected submucosally into the fornix of the vagina lateral to the cervix to block nerve transmission through the paracervical ganglion, which lies lateral and posterior to the junction of the cervix and uterus. Anesthetic agent is injected into the cervix laterally at 3 and 9 o'clock. Because this block does not affect somatic sensory fibers from the perineum, it offers no pain relief for the second stage of labor. Technique of paracervical block. Paracervical block Its use in obstetrics has been limited Because of : Profound fetal bradycardia, Systemic local anesthetic toxicity, Nostpartum neuropathy, Infection. (Paracervical, retropsoal, or subgluteal abscess) Paracervical block The cause of this fetal bradycardia : 1) Reflex Bradycardia, 2) Uterine and/or Umbilical Artery Vasoconstriction 3) Decreased uterine blood flow 4) High fetal blood levels of LA. Paracervical block Usually, we use: Lidocaine Chloroprocaine, 5 to 10 ml of a 1% solution. Bupivacaine is contraindicated because of an increased risk of cardiotoxicity. Pudendal block The pudendal nerves are derived from the lower sacral nerve roots (S2-S4) Sensory innervation for the lower part of the vagina, the vulva, and the perineum, Motor innervation to the perineal muscles. The nerves are easily anesthetized through a transvaginal approach, which is accomplishedby depositing local anesthetic behind each sacrospinous ligament. Local infiltration of the pudendal nerve. (Transvaginal technique) Pudendal block Provides analgesia for vaginal delivery as well as outlet forceps delivery, but it is not useful for labor analgesia. However, it is generally inadequate for midforceps delivery, repair of vaginal lacerations, or exploration of the uterine cavity. Maternal complications from this technique are rare, but include systemic local anesthetic toxicity, infection, and hematoma formation. Local Anesthetics Bupivacaine Levobupivacaine Ropivacaine Lidocaine 2-Chloroprocaine Bupivacaine An amide local anesthetic Commonly used in spinal and epidural anesthesia and analgesia in obstetric practice The placental transfer depends on two factors: 1) the degree of ionization at physiologic pH 2) the extent of protein binding. pKa = 8.05 (highly ionized at physiologic pH) and is 95% protein bound; Limited transfer to the placenta . Bupivacaine The UV/M ratio for bupivacaine ranges from 0.31to 0.44 and is much lower than that for lidocaine. Due to Reports of several deaths related to the cardiovascular or cardiac toxicity of bupivacaine, FDA prohibited the use of a 0.75% epidural solution in obstetric practice. Bupivacaine Bupivacaine consists of two stereoisomers, S− and R+, and is marketed as a racemic mixture of these isomers. When separated, the R component was found to contribute to bupivacaine’s unwanted toxicity. This finding led to develop the use of S isomers for clinical practice: Ropivacaine Levobupivacaine Ropivacaine A homolog of mepivacaine and bupivacaine. Was the first S isomer of a local anesthetic to be marketed. Less soluble than bupivacaine so less potent. Minimum local anesthetic concentration (MLAC) studies have found that the analgesic potency of ropivacaine was 0.60 (0.47 to 0.75) relative to bupivacaine. Minimum local anesthetic concentration (MLAC) Definition: The potency of local anesthetics for neuraxial labor analgesia MLAC is the median effective concentration of local anesthetic solution when administered as a 20-mL bolus. It is lower both for women in early labor and when the local anesthetic is combined with a lipid-soluble opioid. Capogna G, Celleno D, Lyons G, et al. Minimum local analgesia concentration of extradural bupivacaine increases with progression of labor. Br J Anaesth 1998; 80:11-3. Levobupivacaine Long-acting local anesthetic with a clinical profile similar to that of bupivacaine. The lethal dose of levobupivacaine was 1.3- to 1.6-fold higher than other recemic bupivacaine in most animal studies, thereby providing supportive evidence for the greater safety of levobupivacaine should accidental intravascular injection occur. Levobupivacaine Assesment of block with 0.5% bupivacaine and 0.5% levobupivacaine in C/S demonstrated no difference in: 1) Adequacy of the block Time taken to reach a surgically adequate block. Onset or duration of sensory block, Fade-out of sensory and motor blockade, The quality of anesthesia, and muscle relaxation 2) 3) 4) 5) Levobupivacaine Provide epidural analgesia for labor. Levobupivacaine and bupivacaine have equivalent analgesic efficacy. motor blockade was similar between the groups. Fentanyl significantly reduces levobupivacaine requirements for epidural analgesia in labor. Levobupivacaine is not currently being marketed in the United States but is available in many other countries. Lidocaine Used for many years in obstetrics. Quick onset of action with an intermediate duration of action. UV/M ratios= 0.4 to 0.6 Not popular for labor analgesia because of motor block. Lidocaine Controversy in use of 5% hyperbaric lidocaine for SA because of reports of transient neurologic symptoms(TNS). Recent data indicates that the 2.5% and 2% solutions may still cause transient radicular irritation. 2-Chloroprocaine An ester local anesthetic Rapid onset time and short-lived duration of action. Rapid metabolism by ester hydrolysis (half-life, 45 seconds) makes it a safe agent for use in obstetrics because almost no drug crosses the placenta. Disadvantage of chloroprocaine Interfer with the action of epidural opioids. due to antagonism at the µ- and κ-opioid receptors. May also interfere with the action of epidural bupivacaine. Previous preparations of 2-chloroprocaine were considered to be neurotoxic( arachnoiditis after unintentional subarachnoid injection ) Replacement of metabisulfite and methylparaben has eliminated the risk of neurotoxicity. . Chloroprocaine Caution is advised because despite the availability of preservative-free preparations marketed as MPF (methylparaben free), formulations containing preservatives are still commercially available. Recent reports, advocate the use of spinal chloroprocaine. Thank you for your attention