hemoglobin - 3.LF UK 2015
advertisement

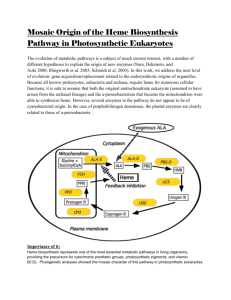
Structure, function and metabolism of hemoglobin Pavla Balínová Figure was adopted from http://themedicalbiochemistrypage.org/hemoglobin-myoglobin.html Hemoglobin (Hb) is a hemoprotein only found in the cytoplasm of erythrocytes (ery) transports O 2 and CO2 between lungs and various tissues normal concentration of Hb in the blood: adult males 135 – 175 g/L adult females 120 – 168 g/L Data were assumed from Department of biochemistry and pathobiochemistry FNKV Structure of hemoglobin • Hb is a spherical molecule consisting of 4 peptide subunits (globins) = quartenary structure • Hb of adults (Hb A) is a tetramer consisting of 2 - and 2 βglobins → each globin contains 1 heme group with a central Fe2+ ion (ferrous ion) Figure is found at http://faculty.etsu.edu/currie/images/hemat3.jpg Heme structure Heme is a metaloporphyrine (cyclic tetrapyrrole) Heme contains: conjugated system of double bonds → red colour 4 nitrogen (N) atoms 1 iron cation (Fe2+) → bound in the middle of tetrapyrrole skelet by coordination covalent bonds methine bridge pyrrole ring Figure is found at http://www.nebrwesleyan.edu/people/nfackler/lecturelinks/images/ Overheads/Fig%2015-A.jpg Properties of iron in heme • Coordination number of iron in heme = 6 6 bonds: • 4x pyrrole ring (A,B,C,D) • 1x link to a protein • 1x link to an oxygen Figure is found at http://www.mun.ca/biochem/courses/3107/images/VVP/Ch07/7-2.jpg In which compounds can we find a heme group? Hemoproteins • Hemoglobin (Hb) • Myoglobin (Mb) • Cytochromes • Catalases (decomposition of 2 H2O2 to 2 H2O and O2) • Peroxidases Figure was assumed from http://en.wikipedia.org/wiki/Heme Myoglobin (Mb) • is a single-chain globular protein of 153 AA, containing 1 heme group • transports O2 in skeletal and heart muscle • is found in cytosol within cells • is a marker of myocard damage Figure is found at http://en.wikipedia.org/wiki/Myoglobin Heme biosynthesis - repetition • in bone marrow (85% of Hb) and liver (cytochromes) • cell location: mitochondria / cytoplasm / mitochondria • substrates: succinyl-CoA + glycine • important intermediates: ● -aminolevulinic acid (= 5-aminolevulinic acid, ALA) porphobilinogen (PBG = pyrrole derivate) uroporphyrinogen III (= porphyrinogen – heme precursor) protoporphyrin IX (= direct heme precursor) key regulatory enzyme: ALA synthase δ-aminolevulinic acid (ALA) • synthesis of heme starts in mitochondria • succinyl-CoA and Gly undergo a condensation → ALA • reaction is catalyzed by enzyme ALA synthase Figure was assumed from textbook Harper´s Illustrated Biochemistry 26th ed./ R.K.Murray; McGraw-Hill Companies, 2003, ISBN 0-07-138901-6. Porphobilinogen (PBG) • ALA leaves the mitochondria → cytoplasm • 2x ALA condense together to form porphobilinogen • reaction is catalyzed by porphobilinogen synthase (ALA dehydratase) Figure was assumed from textbook Harper´s Illustrated Biochemistry 26th ed./ R.K.Murray; McGraw-Hill Companies, 2003, ISBN 0-07-138901-6. Uroporphyrinogen → coproporphyrinogen III • enzyme hydroxymethylbilane synthase catalyzes the linkage of four PBG molecules to yield uroporphyrinogen III • 4 acetate residues are decarboxylated into methyl groups → coproporphyrinogen III returns to the mitochondria again Figure was assumed from book T. M. Devlin et al.: Textbook of Biochemistry With Clinical Correlations, 4th ed., Wiley-Liss, Inc., New York, 1997. Protoporphyrinogen IX → protoporphyrin IX • oxidation of protoporphyrinogen IX produces the conjugated π-electrone system of protoporphyrin IX Figure was assumed from book T. M. Devlin et al.: Textbook of Biochemistry With Clinical Correlations, 4th ed., Wiley-Liss, Inc., New York, 1997. Final formation of heme • Fe2+ is incorporated into protoporphyrin IX • reaction is catalyzed by enzyme ferrochelatase Figure was assumed from http://www.porphyrin.net/mediporph/_netbiochem/synthesis/ ferrochelatase.html Regulation of heme biosynthesis ALA synthase is a key regulatory enzyme ● it is an allosteric enzyme that is inhibited by an end product - heme (feedback inhibition) ● requires pyridoxal phosphate as a coenzyme ● certain drugs and steroid hormones can increase heme synthesis Porphobilinogen synthase is inhibited by lead ions Pb2+ in case of lead poisoning. Ferrochelatase (heme synthase) can be also inhibited by Pb2+. Its activity is influenced by availability of Fe2+ and ascorbic acid. Figure was assumed from book Color Atlas of Biochemistry / J. Koolman, K.H.Röhm. Thieme 2005. ISBN 3-13-100372-3 Hemoglobin degradation In the human body approx. 100 – 200 million ery are broken down every hour. Degradation of Hb begins in ER of reticuloendothelial cells (RES) of the liver, spleen, bone marrow and skin. Hb is degraded to: ● globins → AAs → metabolism ● heme → bilirubin ● Fe2+ → transported with transferrin and used in the next heme biosynthesis Not only Hb but other hemoproteins also contain heme groups which are degraded by the same pathway. Convertion of heme to bilirubin green red-orange Figure is found at http://themedicalbiochemistrypage.org/heme-porphyrin.html Futher fate of bilirubin Bilirubin (Bil) is released from RES into the blood. BUT! Bil is only poorly soluble in plasma, and therefore during transport it is bound to albumin („nonconjugated Bil“). ↓ LIVER In the hepatocytes, Bil is conjugated by 2 molecules of glucuronic acid → bilirubin diglucuronide (soluble in water, „conjugated Bil“) ↓ BILE ↓ INTESTINE Bil is reduced to urobilinogen and stercobilinogen bilirubin-diglucuronide = conjugated bilirubin is soluble in water → „direct bilirubin“ Figure is found at http://themedicalbiochemistrypage.org/heme-porphyrin.html In intestine: Urobilinogen and stercobilinogen can be: a) reabsorbed and returned to the liver (= enterohepatic circulation) b) oxidized (in the presence of O2) to pigments urobilin (orange) and stercobilin (yellow) → they are excreted in the stool Urobilinogen also appears in the urine. Bile pigments: • bilirubin • urobilin • stercobilin Figure was assumed from book Color Atlas of Biochemistry / J. Koolman, K.H.Röhm. Thieme 2005. Clinical correlations Determination of bilirubin (Bil) in serum Blood tests Bil reacts directly when reagents are added to the blood sample → conjugated bilirubin = direct Bil (up to 3.4 µmol/L) free Bil does not react to the reagents until alcohol (methanol) or caffeine is added to the solution. Therefore, the measurement of this type of bilirubin is indirect → unconjugated bilirubin = indirect Bil (up to 13.6 µmol/L) total bilirubin measures both unconjugated and conjugated Bil (normal value up to 17 µmol/L). Types of hemoglobin Adult Hb (Hb A) = 2 α and 2 β subunits HbA1 is the major form of Hb in adults and in children over 7 months. HbA2 (2 α, 2 δ) is a minor form of Hb in adults. It forms only 2 – 3% of a total Hb A. Fetal Hb (Hb F) = 2 α and 2 γ subunits - in fetus and newborn infants Hb F binds O2 at lower tension than Hb A → Hb F has a higher affinity to O2 After birth, Hb F is replaced by Hb A during the first few months of life. Hb S – in β-globin chain Glu is replaced by Val = an abnormal Hb typical for sickle cell anemia Figure is found at http://en.wikipedia.org/wiki/Sickle-cell_disease Fetal Hb vs. adult Hb Pressure units: 1 mmHg = 1 Torr 1 mmHg = 133.22 Pa 1 Pa = 0.0075 mmHg Figure is found at http://en.wikipedia.org/wiki/Fetal_hemoglobin Derivatives of hemoglobin Oxyhemoglobin (oxyHb) = Hb with O2 Deoxyhemoglobin (deoxyHb) = Hb without O2 Methemoglobin (metHb) contains Fe3+ instead of Fe2+ in heme groups Carbonylhemoglobin (HbCO) – CO binds to Fe2+ in heme in case of CO poisoning or smoking. CO has 200x higher affinity to Fe2+ than O2. Carbaminohemoglobin (HbCO2) - CO2 is non-covalently bound to globin chain of Hb. HbCO2 transports CO2 in blood (about 23%). Glycohemoglobin (HbA1c) is formed spontaneously by nonenzymatic reaction with Glc. People with DM have more HbA1c than normal (› 7%). Measurement of blood HbA1c is useful to get info about long-term control of glycemia. Function of hemoglobin • Hb is a buffer (Hb/Hb-H+) in the erythrocytes • Hb is a carrier of O2 and CO2 Binding of O2 is a cooperative. Hb binds O2 weakly at low oxygen pressures and tightly at high pressures. The binding of the first O2 to Hb enhances the binding futher O2 molecules → allosteric effect → S-shaped (sigmoidal) saturation curve of Hb Figures are found at http://www.chemistry.wustl.edu/~edudev/labTutorials/Hemoglobin/ MetalComplexinBlood.html and http://en.wikipedia.org/wiki/Hemoglobin Process of O2 binding to Hb Hb can exist in 2 different forms: T-form and R-form. T-form (T = „tense“) has a much lower oxygen affinity than the R-form. The subunits of Hb are held together by electrostatic interactions. The binding of the first O2 molecule to subunit of the T-form leads to a local conformational change that weakens the association between the subunits → R-form („relaxed“) of Hb. Increasing of oxygen partial pressure causes the conversion of T-form to R-form. T R Hb + ↑pO2 HbO2 Agents that influence oxygen binding 2,3-bisphosphoglycerate (2,3-BPG) only binds to deoxyHb (β-chains) → deoxyHb is thus stabilized ● H+ ions (lower pH) – binding of H+ by Hb lowers its affinity for O2 → Bohr effect ● CO2 – high CO2 levels in the plasma also result in a right shift of saturation curve = Bohr effect ● Figures are found at http://en.wikipedia.org/wiki/Bohr_Effect and http://themedicalbiochemistrypage.org/hemoglobin-myoglobin.html Transport of O2 and CO2 in lungs Figure is found at http://www.mfi.ku.dk/ppaulev/chapter15/Chapter15.html Transport of O2 and CO2 in tissues Figure is found at http://www.mfi.ku.dk/ppaulev/chapter15/Chapter15.htm Metabolism of erythrocyte • ATP is generated by anaerobic glycolysis → ATP is used for ion transport across the cell membrane • glycolysis produces 2,3-BPG and lactate • approx. 5 to 10% of Glc is metabolized by hexose monophosphate pathway → production of NADPH → it is used to maintain glutathione in the reduced state Figure is found at http://themedicalbiochemistrypage.org/hemoglobin-myoglobin.html Porphyrias - disturbances of heme synthesis • are hereditary or acquired disturbances of heme synthesis • in all cases there is an identifiable abnormality of the enzymes which synthesize heme • this leads to accumulation of intermediates of the pathway and a deficiency of heme → excretion of heme precursors in feces or urine, giving them a dark red color ● accumulation of porphyrinogens in the skin can lead to photosensitivity • the neurological symptoms Thalassemias – inherited autosomal recessive blood diaseases • genetic defect results in reduced rate of synthesis of α- or β-globin chain → it causes the formation of abnormal Hb molecules → anemia • are prevalent in populations where malaria was endemic – Arab-Americans, people of Mediterranean origin and Asians • genetic counseling and genetic testing is recommended for families that carry a thalassemia trait