Document
advertisement

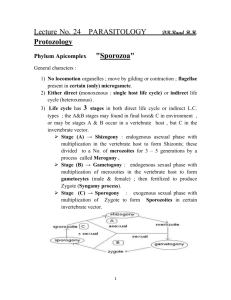
Infection case 12 I2 許師偉 報告日期:2005/10/31 General Data M/28 HIV-seropositive Low CD4 count (50 cells/mm3) for approximately 1 year Chief Complant Diarrhea for 10 weeks and a recent weight loss of 20 lb Subjective Finding Watery diarrhea and profuse but nonbloody Antidiarrheal medications (e.g., loperamide HC1 [Imodium]) were not successful in alleviating his condition. Objective Finding Signs of dehydration on examination A stool specimen was collected for routine culture for bacterial pathogens.(Negative finding) Three stool specimens, collected on alternate days, were examined for ova and parasites.(Positive finding) Positive stool exam finding Pale oval structures The permanent stained trichrome smear showed evidence of a protozoan parasite A modified acid-fast procedure(a special stain for coccidia ) revealed elliptical pink structures measuring 25 to 30 μm. Each structure was surrounded by a clear, double-layer wall. QUESTIONS 1 Which protozoan parasite do you think is causing this patient's illness? What are the structures seen in the patient's stool specimen? Ans:(1)Isospora belli (2) An oocyst of Isospora belli showing 1 sporocyst Adapt from UKNEQAS Parasitology 1. 2. 3. 4. Routine procedure for the microscopic examination of faecal samples for parasites Direct microscopy should be done on all unformed and liquid samples by mixing a small amount of the specimen in 0.9% sodium chloride solution. This permits detection of trophozoites of Entamoeba histolytica and Giardia lamblia. It can also provide information on the content of the stool ie the presence of leucocytes and red blood cells. A formol-ether concentrate should be done on all faecal samples examined for parasites. This reveals the presence of most protozoan cysts, eggs of nematodes, cestodes and trematodes and also the larval stages of some nematodes. A permanently stained direct faecal smear should be used for all bloody, liquid or semi-formed stools. The smear can reveal the presence of intestinal parasites which can be either destroyed or missed by the formol-ether concentration method eg. Dientamoeba fragilis. Specimens from patients with HIV should be left in 10% formalin for hour before proceeding with parasite examination. Adapt from UKNEQAS Parasitology Faecal smears are made for the following reasons: Provide information on the exudate present. (Romanowsky stains) Helpful in accurately identifying flagellates. (Romanowsky stains, Iron haematoxylin) When parasites cannot be detected in either the direct wet preparation or concentrated deposit, a permanent stain of a fresh faecal smear can reveal the presence of intestinal parasites. (Romanowsky stains, Trichrome stain, modified Ziehl-Neelsen) Useful in demonstrating the nuclear patterns of cysts thus facilitating identification. (Iron haematoxylin, Trichrome stain) Adapt from UKNEQAS Parasitology Trichrome Stain The trichrome method for staining protozoa is especially recommended for identifying features of amoebic cysts and trophozoites Adapt from UKNEQAS Parasitology Modified Ziehl-Neelsen Use of the modified Ziehl-Neelsen stain for faecal smears has already been established for coccidian protozoa, in particular, oocysts of Cryptosporidium species, but it is also useful to confirm the presence of oocysts of Isospora belli and Cyclospora cayetanensis. J Antimicrob Chemother. 1996 May;37 Suppl B:61-70. Recently recognised microbial enteropathies and HIV infection. Farthing MJ, Kelly MP, Veitch AM Digestive Diseases Research Centre, Medical College of St Bartholomew's Hospital, London, UK. At least 80% of cases of persistent diarrhoea in patients with HIV/AIDS can be attributed to a specific enteropathogen. The coccidian parasites Cryptosporidium parvum, Isospora belli and Cyclospora and the Microsporidia account for at least 50% of cases of persistent diarrhoea in the industrialised and developing world Adapt from UKNEQAS Parasitology Oocysts are thin walled, transparent and ovoid in shape. They can be demonstrated in faeces after formal ether concentration where they appear as translucent, oval structures measuring 20-33μm by 10-19μm. Alternatively, oocysts can be seen in a faecal smear stained by a modified Ziehl-Neelsen method , where they stain a granular red colour against a green background, or by phenolauramine. QUESTIONS 2 Why was the modified acid-fast procedure needed to definitively identify the parasite? Adapt from UKNEQAS Parasitology Modified Ziehl-Neelsen Use of the modified Ziehl-Neelsen stain for faecal smears has already been established for coccidian protozoa, in particular, oocysts of Cryptosporidium species, but it is also useful to confirm the presence of oocysts of Isospora belli and Cyclospora cayetanensis. Method a. Faecal smears are made either directly from the stool sample or from the concentration deposit. b. Allow to air dry. c. Fix in methanol for 3 minutes. d. Stain with strong carbol fuchsin for 15-20 minutes. e. Rinse thoroughly in tap water. f. Decolourise in acid alcohol (1% HCl in methanol) for 1520 seconds. g. Rinse thoroughly in tap water. h. Counterstain with 0.4% malachite green (or methylene blue) for 30-60 seconds. i. Rinse thoroughly and air dry. j. Examine using x40 and x100 objectives. QUESTIONS 3 Which other two coccidian parasites give a similar reaction when stained by the modified acid-fast procedure? Adapt from UKNEQAS Parasitology Cryptosporidium parvum Cyclospora cayetanensis Adapt from UKNEQAS Parasitology Cryptosporidium parvum Definitive diagnosis of cryptosporidiosis is by finding the characteristic spherical oocysts in faecal samples. Sporulated oocysts measuring 4-6 m in diameter and containing up to 4 sporozoites are passed into the faeces. Adapt from UKNEQAS Parasitology Cyclospora cayetanensis The oocysts of C. cayetanensis are spherical, measuring 810 in diameter QUESTIONS 4 How would you distinguish these three parasites? Adapt from UKNEQAS Parasitology Microscopic Characterists cs Cryptosporidiu m parvum Isospora belli Cyclospora cayetanensi s Size 4-6 20-33 & 10 - 19 8 - 10 Identified in formol-ether concentrate by light microscopy No Yes Yes Identified by modified Ziehl- Yes Yes Yes Shape of the oocyst spherical oval spherical Identified by Phenol Auramine Yes Variable No Neelsen stain QUESTIONS 5 Describe the life cycle of the parasite causing this patient's infection Adapt from UKNEQAS Parasitology The life cycle of Isospora belli involves an asexual (schizogonic stage) and a sexual (sporogonic stage) Infection with I. belli occurs in both immunocompetent and immunocompromised patients and begins when the mature oocyst is ingested in water or food.The mature oocyst contains 2 sporocysts, each containing 4 sporozoites. The sporulated oocyst is the infective stage of the parasite and they excyst in the small intestine releasing sporozoites which penetrate the epithelial cells, thus initiating the asexual stage of the lifecycle. The sporozoite develops in the epithelial cell to form a schizont which ruptures the epithelial cell containing it, liberating merozoites into the lumen. These merozoites will then infect new epithelial cells and the process of asexual reproduction in the intestine proceeds. Some of the merozoites form macrogametes and microgametes (sexual stages) which fuse to form a zygote which matures to form an oocyst. QUESTIONS 6 Why would this patient pose less risk to laboratory personnel than patients infected with other coccidian parasites? Cryptosporidium parvum Thick wall sporulated oocysts, containing 4 sporozoites, are excreted by the infected host through feces and possibly other routes such as respiratory secretions . Transmission of Cryptosporidium parvum occurs mainly through contact with contaminated water (e.g., drinking or recreational water). Occasionally food sources, such as chicken salad, may serve as vehicles for transmission. Cyclospora cayetanensis When freshly passed in stools, the oocyst is not infective (thus, direct fecal-oral transmission cannot occur; this differentiates Cyclospora from another important coccidian parasite, Cryptosporidium). In the environment , sporulation occurs after days or weeks at temperatures between 22°C to 32°C, resulting in division of the sporont into two sporocysts, each containing two elongate sporozoites. Fresh produce and water can serve as vehicles for transmission and the sporulated oocysts are ingested (in contaminated food or water) . Isospora belli At time of excretion, the immature oocyst contains usually one sporoblast (more rarely two) . In further maturation after excretion, the sporoblast divides in two (the oocyst now contains two sporoblasts); the sporoblasts secrete a cyst wall, thus becoming sporocysts; and the sporocysts divide twice to produce four sporozoites each . Infection occurs by ingestion of sporocysts-containing oocysts QUESTIONS 7 How is infection with this parasite transmitted? Infection is a result of the ingestion of a infective of sporulated oocyst. QUESTIONS 8 How should this patient be treated? NEJM Volume 320:1044-1047 April 20, 1989 Number 16 Treatment and prophylaxis of Isospora belli infection in patients with the acquired immunodeficiency syndrome JW Pape, RI Verdier, and WD Johnson I. belli responds well to treatment with trimethoprim-sulfamethoxazole, but there is a high rate of recurrence. We conclude that isosporiasis in patients with AIDS can be treated effectively with a 10-day course of trimethoprim(160 mg) sulfamethoxazole(800 mg) four times a day , and that recurrent disease can subsequently be prevented by ongoing prophylaxis with either trimethoprimsulfamethoxazole or sulfadoxinepyrimethamine.