File - Kriti Acharya
advertisement

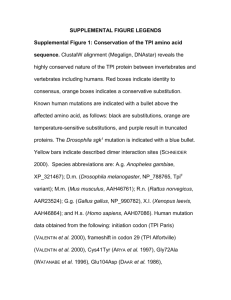
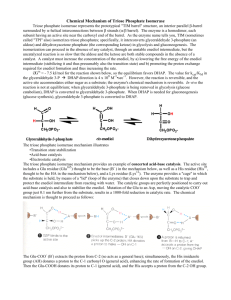
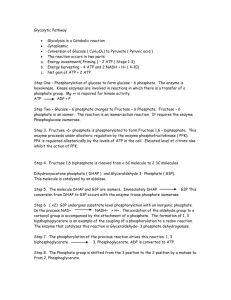
Kriti Acharya Loras College, Dubuque Iowa Division of Molecular and Life Science Biochemistry DYOD Assignment December 3, 2010 A single amino acid substitution at position 95 (H95G) of Triose-phosphate Isomerase (TPI) causes excess glycogen deposition in liver and muscles and leads to obesity. The second stage of glycolysis begins with the splitting of fructose 1, 6-bisphosphate into glyceraldehyde 3-phosphate (GAP) and dihydroxyacetone phosphate (DHAP). Glyceraldehyde 3-phosphate is on the direct pathway of glycolysis whereas dihydroxyacetone phosphate is not. Unless a means exist to convert dihydroxyacetone phosphate into glyceraldehyde 3-phosphate, a three carbon fragment useful for generating ATP will be lost. Triose-phosphate Isomerase (TPI) is a major enzyme that catalyzes the reversible interconversion of dihydroxyacetone phosphate (DHAP) and D-glyceraldehyde 3-phosphate (GAP). At equilibrium, 96% of the triose-phosphate is DHAP whereas only 4% is GAP (Harris T.K. et al). X-ray crystallographic and other studies show two important residues Glu165 and His95 located on the active site pocket of TPI that play important role in isomerization reaction (Alber T. et al). Fig 1. Catalytic mechanism of Triosephosphate Isomerase As shown in figure 1, Glu165 acts as a general base by abstracting a proton (H+) from carbon 1 and then donates it to carbon 2. This process is assisted by His95 located adjacent to Glu165. His95 acts as a general acid and stabilizes the negative charge that develops on the Carbon 2 by donating its proton. Glu165 now acting as a general acid donates a proton to Carbon 2 while His95 removes a proton from the OH of Carbon 1 (Komives E.A. et al). There are several diseases associated with the enzyme Triose- Phosphate isomerase. TriosePhosphate isomerase deficiency is a severe multisystemic disease with autosomal recessive inheritance. It is mainly characterized by early-onset chronic hemolytic anemia, always present, and progressive neurological involvement that starts between 6 and 30 months of age. Other clinical signs can be observed, in particular, diaphragm paralysis that requires assisted ventilation, cardiomyopathy and an increased susceptibility to infections. The incidence is not known and only 30 or so cases have been described in the world. The TPI gene is located on chromosome 12, diverse mutations have been identified. Prenatal diagnosis can be obtained by enzymatic assay and/or molecular biology. (Livet, 2003) A group of people in certain community show unusual disease with enlarged muscles and liver containing heavy amount of glycogen deposition, less mobility of body, neurologic disorder and physical inability to perform vigorous exercise. Also these people required twice the amount of food to perform everyday activities. It was known that this group of people had single amino acid mutation in one important enzyme involved in glycolysis. A single amino acid substitution at position 95 (H95G) of Triosephosphate Isomerase was hindering its isomerization functionality. It is because glycine, unlike histidine, cannot stabilize the negative charge that develops on DHAP since it cannot donate a proton. Hence, the catalysis cannot come to completion. As a result, one molecule of glucose (6C) can only form one molecule of GAP (3C), which will almost reduce the energy production by half the quantity. DHAP (3C) produced will not yield any ATP or energy production. This will slow the glycolytic cycle and the glucose 6- phosphate will in fact take alternative pathway for the synthesis of glycogen in liver and muscles. In fact, excessive accumulation of DHAP inside the cytoplasm might increase the pH of the cytoplasm (due to its negative charge on phosphate moiety) or randomly phosphorylate other proteins involved in normal physiological function. This might be a cause of neurological disorder. In order to detect this disease process, first we need to acquire the entire sequence of all the proteins involved in glucose related pathways both from healthy cell and diseased patients as well. Then, we need to compare the sequence of amino acids in both of these samples. We should focus more on the residues at the active catalytic site of these proteins. It is because small amino acid mutations in the catalytic site can drastically change the activity and functionality of the enzyme. This will take us to the active site of TPI. Other way of detection would be to measure the elevated level of Triosephosphate (DHAP and GAP) level inside the cytoplasm. This can be performed by exploiting the physical properties of these compounds. Also it has been reported in humans that deficiencies in TPI are associated with a progressive, severe neurological disorder and is characterized by chronic hemolytic anemia (Orosz F. et al). Relevance to any of these symptoms can also help us predict where the problem might be. In order to treat this disease, we need to find an activator of mutant Triosephosphate Isomerase (MTPI) that can increase its activity. In order to do that, we first need to standardize a kinetic assay where we can detect the activity of MTPI under lab conditions. We will first have to find a substrate (S) which is acted upon by MTPI via same mechanism by which it acts on DHAP and GAP. Also this substrate (S) should exhibit some physical properties such as absorbance, fluorescence radioactivity by itself or when it is acted upon by enzyme MTPI. Once this substrate is detected, we will next prepare mutant Triosephosphate Isomerase protein using recombinant DNA technology. E. coli strains can be used to transform plasmid containing MTPI gene. After taking through different rounds of cell culture, cell lysis, purification, column chromatography and concentration, MTPI can be extracted and used for kinetic purposes. Our kinetic assay will require DHAP as a substrate, MTPI as an enzyme and buffer solution for maintaining the pH close to 7.5 (physiological pH). We will first find a range at which we can see linear activity of enzyme. Activity can be detected by measuring the amount of change in its absorbance/fluorescence/radioactivity. Once we optimize our activity assay, we now need to screen for activators. In order to do so, we will perform kinetic experiment in the presence of lots of compounds. These compounds are called chemical libraries and the process is called High Throughput Screening. With this method we can screen hundreds of thousands of compounds with few hours. By screening all those many compounds, I expect to find some compounds that might mimic the function of His95 and bind on to the same site. This can re-establish the function of MTPI and help it catalyze its substrate more effectively. Further, these compounds will be tested in vivo in human cells to see if it reestablishes the glycolytic function. If so, then these compounds will be taken further for preclinical and clinical studies. A flowchart showing the process of drug discovery and development is shown below in figure 2. Figure 2. Process of drug discovery and drug development Bibliography: Harris T.K., Cole R.N. (1998). Proton transfer in the Mechanism of Triosephosphate Isomerase. Biochemistry 37 (47) 16828-16838 Alber T., Banner D.W. (1981). On the three-dimensional structure and catalytic mechanism of Triosephosphate Isomerase. Phil. Trans. R. Soc. 293 (1063) 159-171 Orosz F., Olah J. (2008). Triosephosphate Isomerase deficiency: facts and doubts.IUBMB life 58 (12) 703-715 Komives E.A., Chang L.C. (1991). Electrophilic catalysis of Triosephosphate Isomerase: the role of Histidine 95. Biochemistry 30(12) 3011-3019 Livet, M.O; Triose-phosphate isomerase deficiency. Orphanet encyclopedia, September 2003. Boyer Rodney. (2006). Concepts in Biochemistry. (3rd ed.). Hoboken NJ: Von Hoffman Press.