(sydney, courtney, michelle) - 34-601ClinicalAnatomy
advertisement

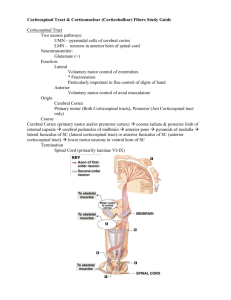
Corticospinal Tract & Corticonuclear (Corticobulbar) Fibers Study Guide Corticospinal Tract • • Two neuron pathways: • UMN – pyramidal cells of cerebral cortex • LMN – neurons in anterior horn of spinal cord Neurotransmitter: • • Glutamate (+) Function: • • Lateral • Voluntary motor control of extremities • * Fractionation • Particularly important in fine control of digits of hand Anterior • • Voluntary motor control of axial musculature Origin • Cerebral Cortex • Primary motor (Both Corticospinal tracts), Premotor (Ant Corticospinal tract only) • Course • Cerebral Cortex (primary motor and/or premotor cortex) corona radiata & posterior limb of internal capsule cerebral peduncles of midbrain anterior pons pyramids of medulla lateral funiculus of SC (lateral corticospinal tract) or anterior funiculus of SC (anterior corticospinal tract) lower motor neurons in ventral horn of SC • Termination • Spinal Cord (primarily laminae VI-IX) Lesions • Myasthenia Gravis • Moderate to profound weakness of skeletal muscles; caused by circulating antibodies that react with postsynaptic nicotinic acetylcholine receptors. • Patients with this present with progressive fatigability throughout the day. • Ocular muscles effected – 85% of pts • Symptoms: weakness in limb muscles, facial/oral weakness, diplopia, ptosis, dysphagia, dysarthria • • Lateral Corticospinal Tract Lesion • Ipsilateral UMN signs (Lesion below the level of decussation) • Contralateral UMN signs (Lesion above the level of decussation) • Tumors or MS affect the lateral corticospinal tract • Symptoms: weakness, hypotonia, hyperflexia Any lesion in SC will result in ipsilateral UMN signs because the deccussation occurs at the medulla (SC is below the level of deccussation) Corticonuclear (Corticobulbar) Fibers • Two neuron pathway: • UMN – cells of cerebral cortex • • LMN – motor cranial nerve nuclei in brainstem Fibers influence motor nuclei of oculomotor, trochlear, trigeminal, abducens, facial, glossopharyngeal, vagus, accessory, & hypoglossal nerves • • Function • Controls muscles of face, head & neck • Initiation and control of voluntary & fine movements Neurotransmitter • • Glutamate (+) Innervated by the cranial motor nuclei (V, VII, XII), nucleus ambiguus (IX and X) & by accessory nucleus • DOES NOT innervate nuclei for nerves III, IV, and VI • Fibers do NOT project to the oculomotor, trochlear, and abducens DIRECTLY (from frontal eye fields to terminate in mesencephalon [sup colliculus] and then relay input to the motor nuclei • Origin • Precentral gyrus - somatomotor cortex, area 4 (primary motor cortex) • Frontal eye fields - areas 6 and 8 • Postcentral gyrus - areas 3, 1, 2 (some) • Course • Precentral gyrus descends through corona radiata genu of internal capsule (few fibers in the posterior limb of the internal capsule) crus cerebri brainstem • Major Structures • Precentral gyrus, corona radiate, genu of internal capsule, posterior limb of internal capsule, cerebral peduncles (midbrain), brainstem (medulla & pons), cranial nerve nuclei • Termination • • Frontal eye fields • Rostral Interstitial Nucleus of the MLF • Paramedian Pontine Reticular Formation Precentral gyrus • Brainstem motor nuclei: CN V (bilateral), CN VII (contralateral), CN XII (contralateral tongue) • Nucleus Ambiguus (bilateral): CN IX, CN X (soft palate, pharynx, larynx) • Accessory Nucleus (bilateral): CN XI Upper half of the facial motor nucleus receives BILATERAL corticonuclear projections Lower half of the facial motor nucleus receives only CONTRALATERAL projections • Pseudobulbar Palsy • Bilateral lesion • • Inability to control facial movements • Caused by variety of neurological disorders (ALS, MS, Parkinson’s) • Symptoms: Dysphagia, Dysarthria, Paresis of tongue, loss of emotional control One-and-a-Half Syndrome • Results from unilateral lesion of the paramedian pontine reticular formation (PPRF) and the ipsilateral MLF • Loss of ipsilateral abduction (lateral rectus), adduction & contralateral loss of adduction (EYE MOVEMENT) • Only remaining horizontal movement is contralateral abduction