CBCL Baseline by 18-Months
advertisement

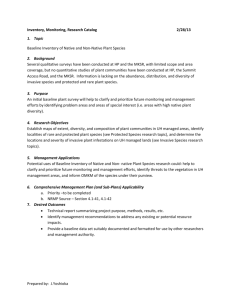
Lessons from the U.S. National Survey of Child and Adolescent Well-Being (NSCAW): How Are the Children Faring and Did Mental Health Services Help? Richard P. Barth School of Social Work University of Maryland Presented at ACWA Annual Conference Research Forum University of WashingtonAugust 15, 2006 The research for this presentation was funded by the Administration on Children, Youth, and Families of the U.S. Department of Health and Human Services. Although I am grateful to the NSCAW Research Group for their work, points of view or opinions in this presentation and accompanying documents are those of the presenter and do not necessarily represent the position or policies of the U.S. DHHS or of my NSCAW colleagues. Results are preliminary and not to be quoted in print or other media. I am grateful to the Fulbright Commission for an award as a Senior Specialist First National Random Sample Study Of CWS • Extended Research Team included: – Research Triangle Institute – University of North Carolina – San Diego Children’s Hospital, CASRC – CSRD, Pitt Medical Center – National Data Archive on Child Abuse and Neglect, Cornell – 92 Local Child Welfare Agencies – Federal Admin. For Children and Families – Children and Families – Taxpayers of US who have provided more than $40,000,000 in support NSCAW Cohort at Baseline Total 6,231 Long-term foster care 727 Enter through investigation 5,504 No services 1,725 Other gateways 600 Ongoing services 3,779 In home 2,312 Out-of-home 1467 Wellbeing Measures • Infant Development (0 – 2 years) – Battelle Developmental Inventory (BDI) – Bayley Infant Neurodevelopmental Screener (BINS) – Vineland Adaptive Behavior Screener (VABS) • Cognitive Domain – Preschool Language Scale-3 (PLS-3) – Mini-Battery of Achievement (MBA) • Social Domain – Vineland Adaptive Behavior Scale Screener, Daily Living Skills domain (VABS) – Social Skills Rating System (SSRS) • Behavioral Domain – Child Behavior Checklist (CBCL) • Risky Behaviors (11+ years) – Self-Report Delinquency (SRD) – Substance Abuse – Sexual Behavior – Suicide Family Cumulative Risk Score • Risk Assessment section (CW worker) • 23 items (e.g., including trouble meeting basic needs, substance abuse, past CW involvement, domestic violence, parent psychopathology) • Proportional score created – Low risk (< 22%) – Medium risk (22% to 40%) – High risk (40%) When using as predictor of child behavior (e.g., CBCL), child behavior variables are omitted from this score Risky Behavior Domain (11 to 15 at BL) Self-Report Delinquency (SRD) • Modified version of the SRD (Elliott & Ageton, 1980) used for Wave 7 (1987) of the NLSY • 72 Questions: – 36: Acts committed in previous 6 months – 36: Frequency of acts • Scoring: Acts weighted by seriousness & multiplied by frequency • Cronbach’s α = .98 Substance Abuse • Modified from Youth Risk Behavior Survey items • 14 questions: 7: Substances used past 30 days 7: Frequency of use • Scoring: Acts weighted by seriousness & multiplied by frequency Risky Domain (11 to 15 at BL) Voluntary Sexual Behavior Suicidal Behavior Risk Three items ask (1) Had youth ever had intercourse; (2) Consistency of use of protection for sexual intercourse; and (3) Had youth ever been pregnant or gotten someone pregnant (0 = “No” or not applicable, 1 = “Yes”). Scores ranged from 0 to 5 • No risk (0, Never had intercourse or Items from the Youth Self Report, and the Children’s Depression Inventory Six items ask the youth and caregiver about thoughts, plans, and suicides attempts of the child Scores range from 0 to 17 • No risk (0, No suicidal behavior • • first experience was coerced) Low risk (1, Has had intercourse but used protection consistently and has never been/gotten someone pregnant) Medium/High risk (2-5, Inconsistent use of protection and possible pregnancy) reported) • • Low risk (1 – 3, Suicidal thoughts in the past two weeks) Medium/High risk (4–17, Has deliberately tried to harm self and/or has had suicidal thoughts in the past two weeks, and has a plan) Change in Developmental Well-Being of Children Involved with CWS from Baseline to 18 Months 1. Conditional Probability of Change 2. Change scores and effect sizes 3. Assessment of Contributors to Well-Being Using General Estimating Equations Age Groups andWell-Being Measures Domain Measure Age Group 0-2 3-5 6-10 Development Bayley Infant Neurodevelopmental Screener (BINS) x Social x Vineland Adaptive Behavior Scales Screener (VABS) Social Skills Rating System (SSRS) Cognitive Battelle Developmental Inventory (BDI) x Preschool Language Scale-3 (PLS-3) x x x x x x Mini Battery of Achievement (MBA) Behavior Child Behavior Checklist (CBCL) x x x Proportion of Developmental/Clinical Cutting Scores Per Child^ 40 40 35 Baseline (W1) 18 months (W3) Percent 30 25 20 15 15 10 5 12 11 9 7 6 8 8 7 2 9 4 1 1 2 4 1 1 0 .3 1 0 .11 0 .3 2 0 0.00 0.17 0.20 0.25 0.33 0.40 0.50 0.60 0.67 0.75 0.80 0.83 1.00 Proportion of Clinical Scores ^Number of possible measures per child varies from 4 to 7 Changes in Cognitive Development Score (BDI) for 0-2 Year Old Children: Baseline to 18-Months Baseline Mean (SE) 18 months Mean (SE) Effect Size In-home at baseline and 18 months (n=881) 42.0 (.97) 42.1 (1.25) +.01 Out-of-home at baseline and 18 months (n=312)** 44.2 (2.02) 40.1 (1.83) -.32 Total (n=1493) 42.6 (.92) 42.0 (1.04) -.05 Setting Note: 454 cases were deleted such that the number of cases with valid scores at Baseline and 18 Months were equal for the purposes of comparison. All analyses are on weighted data. Total group also includes cases with mixed placement types across waves (I.e., in-home to out-of-home, and out-ofhome to in-home). ** p < .01 Changes in Risk for Developmental Delay or Neurological Impairment (BINS) for Children 0-2, Baseline to 18-Months Risk for Developmental Delay or Neurological Impairment at 18 Months Risk for Developmental Delay or Neurological Impairment at Baseline Low Moderate High Low (n=59) .02 .04 .02 Moderate (n=132) .03 .13 .15 .07 .20 .35 High (n=367) All analyses are on weighted data. Red (upper) triangle shows negative change, Green (lower) shows improvement. Change in (BINS) for Children 0-2, BL to 18Months (In-Home Only) Risk for Developmental Delay or Neurological Impairment at Baseline Risk for Developmental Delay or Neurological Impairment at 18 Months Low Moderate High Low (n=31) .01 .05 .02 Moderate (n=78) .04 .13 .16 .07 .15 .38 High (n=167) All analyses are on weighted data. Red (upper) triangle shows negative change, Green (lower) shows improvement. Change in (BINS) for Children 0-2, BL to 18Months (Out-of-Home Only) Risk for Developmental Delay or Neurological Impairment at 18 Months Risk for Developmental Delay or Neurological Impairment at Baseline Low Moderate High Low (n=16) .05 .02 .01 Moderate (n=21) .00 .14 .14 .07 .23 .34 High (n=110) All analyses are on weighted data. p<.001 (Bowker’s test); Red (upper) triangle shows negative change,Green (lower) shows improvement. Changes in Language Skills Score (PLS-3) for 0-2 Year Old Children: Baseline to 18-Months Baseline Mean (SE) 18 months Mean (SE) Effect Size In-home at baseline and 18 months (n=879)* 91.3 (1.31) 87.8 (1.03) -.20 Out-of-home at baseline and 18 months (n=317) 90.0 (1.31) 86.5 (1.72) -.22 Total (n=1501)** 91.3 (1.05) 87.8 (.89) -.20 Setting Note: 438 cases were deleted such that the number of cases with valid scores at Baseline and 18 Months were equal for the purposes of comparison All analyses are on weighted data. Total group also includes cases with mixed placement types across waves (I.e., in-home to out-of-home, and out-ofhome to in-home). * p < .05; ** p < .01 Changes in Language Skills Score (PLS-3) for 3-5 Year Old Children: Baseline to 18-Months Baseline Mean (SE) 18 months Mean (SE) Effect Size In-home at baseline and 18 months (n=252)** 88.4 (1.84) 94.6 (2.90) +.36 Out-of-home at baseline and 18 months (n=41)* 76.1 (5.87) 82.6 (6.88) +.33 Total (n=345)** 88.1 (1.67) 95.0 (2.48) +.39 Setting Note: 401 cases were deleted such that the number of cases with valid scores at Baseline and 18 Months were equal for the purposes of comparison All analyses are on weighted data. Total group also includes cases with mixed placement types across waves (I.e., in-home to out-of-home, and out-ofhome to in-home). * p < .05; ** p < .01 Changes in Daily Living Skills (VABS) Baseline to 18-Months by Setting and Age Age at baseline In-home at baseline and 18 months Out-of-home at baseline and 18 months + change change + change change 3-5 25% 19% 8% 19% 6-10 15% 11% 21% 8% 0-2 Red shows negative change, Green shows improvement. CBCL Changes for Children (Ages 3-5): Served at Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .53 .07 .08 2. Borderline .05 .01 .03 3. Clinical .06 .03 .14 Baseline Total unweighted n =529. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Changes for Children (Ages 3-5): Served Out-of-Home* CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical .34 .05 .07 0 0 .01 .10 .01 .41 Baseline 1. Normal 2. Borderline 3. Clinical Total unweighted n =74. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Change Over 18 months (Children Aged 3 to 5 Years at BL) Child Gender* Male* Female Child Race/Ethnicity* Black/Non-Hispanic* White/Non-Hispanic Hispanic Other Parent Cumulative Risk Low Medium High* Beta (Units Change in CBCL Score) 3.25 Reference Group -3.45 Reference Group -1.85 1.74 Reference Group 3.03 3.27 Non-significant Variables: Wave, Proportion of Time of Out-of-Home Care, In-Home at Both Waves, Poverty Level *p<.05 **p<.01 ***p<.001 CBCL Changes for Children (Ages 6-10): Served at Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .55 .02 .04 2. Borderline .04 .01 .03 3. Clinical .11 .03 .16 Baseline Total unweighted n =877. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Changes for Children (Ages 6-10): Served Out-of-Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .36 .04 .04 2. Borderline .03 .01 .03 3. Clinical .19 .04 .28 Baseline Total unweighted n =152. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Changes Over 18 Months (Children Aged 6 to 10 Years at BL) Gender* Beta Male* 2.13 Female Reference Group Child Race/Ethnicity Black/Non-Hispanic -0.28 White/Non-Hispanic Reference Group Hispanic** -3.89 Other -1.89 Wave*** Baseline Reference Group 18 Months*** -2.56 Proportion of Time in Out-of-Home Care* In-Home Reference Group Out-of-Home 4.74 Mixed* 4.70 Non-significant Variables: In-Home at Both Waves, Poverty Level, Parent Cumulative Risk **p<.05 **p<.01 ***p<.001 CBCL Changes for Children (Ages 11+): Served at Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .38 .03 .06 2. Borderline .06 .03 .04 3. Clinical .10 .04 .27 Baseline Total unweighted n =654. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Changes for Children (Ages 11+): Served Out-of-Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .29 .07 .13 2. Borderline .07 <.01 .01 3. Clinical .14 .01 .28 Baseline Total unweighted n =147. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Scores^ Over 18 months (Children Aged 11 to 15 Years at BL) Significant Predictor TIME (WAVE)* Baseline 18 Months* Beta Reference Group -1.43 *p<.05 Non-significant Predictor: Gender, Child Race/Ethnicity, Proportion of Time in Out-of-Home Care, In-Home at Both Waves, Poverty Level, Parent Cumulative Risk, Substance Abuse, and Delinquency ^Measured using Child Behavior Checklist CBCL Changes for Children (Ages 2-15): Served at Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .51 .04 .05 2. Borderline .05 .01 .03 3. Clinical .09 .03 .18 Baseline Total unweighted n =2244. Red (upper) triangle shows negative change, Green (lower) shows improvement. CBCL Changes for Children (Ages 2-15): Served Out-of-Home CBCL Total Score 18 Months Group 1. Normal 2. BRDL 3. Clinical 1. Normal .33 .05 .08 2. Borderline .03 <.01 .02 3. Clinical .15 .02 .30 Baseline Total unweighted n =401. Red (upper) triangle shows negative change, Green (lower) shows improvement. Summary of Changes in CBCL Baseline to 18-Months by Setting and Age Age at baseline In-home at baseline and 18 months Out-of-home at baseline and 18 months + change change + change change 3-5 14% 16% 11% 13% 6-10 18% 9% 26% 11% 11+ 20% 13% 22% 21% Red shows greater negative change, Green shows greater improvement. • 3-5 year olds show more negative change across settings than 6-10 year olds • 6-10 year olds show more positive change at home •11-15 year olds show more positive change across settings CBCL Changes for All Children Since BL Non-significant Variables: Gender, InHome at Both Waves, and Poverty Level Child Age at Baseline*** Beta 2 years*** -5.62 3-5 years*** -3.87 6-10 years*** -3.73 11+ years Reference Group Child Race/Ethnicity* Black/Non-Hispanic -0.90 White/Non-Hispanic Reference Group Hispanic** -3.10 Other -0.24 Wave*** Baseline Reference Group 18 Months*** -1.55 Proportion of Time in Out-of-Home Care** In-Home Reference Group Out-of-Home** 4.36 Mixed 2.31 Parent Cumulative Risk*** Low Reference Group Medium** 2.59 High*** 3.42 **p<.05 **p<.01 ***p<.001 Self-Reported Delinquency Changes for Children (Ages 11-15) Served at Home Delinquency Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .41 .09 .05 .01 Low .08 .04 .04 .02 Medium .04 .03 .03 .02 High .02 .02 .03 .06 Unweighted n=624 Red (upper) shows negative change, Green (lower) shows improvement. Self-Reported Delinquency Changes for Children (Ages 11-15) Served Out of Home Delinquency Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .40 .07 .10 .01 Low .04 .02 .02 .01 Medium .07 .07 .02 .02 High .03 .02 .03 .07 Unweighted n=141 Red (upper) shows negative change, Green (lower) shows improvement. Suicide Risk Changes for Children (Ages 11-15) Served in Home Suicide Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .55 .08 .01 .02 Low .10 .05 .01 .01 Medium .02 .01 <.01 .00 High .08 .03 .01 .03 Unweighted n=664 Red (upper) shows negative change, Green (lower) shows improvement. Suicide Risk Changes for Children (Ages 11-15) Served Out of Home Suicide Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .57 .06 .00 .01 Low .14 .01 .03 .01 Medium 0 0 0 0 High .05 .08 .01 .04 Unweighted n=156 Red (upper) shows negative change, Green (lower) shows improvement. Substance Abuse Risk Changes for Children (Ages 11-15) Served at Home Substance Abuse Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .48 .11 .10 .02 Low .06 .03 .03 .01 Medium .03 .01 .06 .02 High .01 <.01 .02 .02 Unweighted n=605 Red (upper) shows negative change, Green (lower) shows improvement. Substance Abuse Risk Changes for Children (Ages 11-15) Served Out of Home Substance Abuse Risk Level at 18 Months Baseline No Risk Low Medium High No Risk .59 .09 .05 .01 Low .02 .02 .01 .00 Medium .06 .02 .05 .01 High <.01 <.01 .03 .03 Unweighted n=135 Red (upper) shows negative change, Green (lower) shows improvement. Summary of Changes in Risk Behavior to 18Months by Setting and Age Risk In-home at baseline and 18 months Out-of-home at baseline and 18 months + change change + change change Delinquency 22% 23% 26% 23% Suicide 25% 13% 28% 11% Substance Abuse 14% 29% 15% 17% Red shows greater negative change, Green shows greater improvement. CTS-PC (Child) Scores for Inappropriate Parenting, BL to 18 Months (Children 11+) Baseline Mean (SE) 18 months Mean (SE) Effect Size In-home at baseline and Wave 3 (n=536) 12.3 (1.6) 12.0 (16) .02 Out-of-home at baseline and 18 months (n=161) 21.7 (3.4) 9.4*** (3.4) .39 13.6 (1.4) 11.7 (1.4) .08 Setting Total (n=848)^ ^Total includes children in mixed placement settings p<.05**, p<.01***, p<.001 CTS-PC (Child) Scores for Severe Violence, BL to 18 Months (Children 11+) Baseline Mean (SE) 18 months Mean (SE) Effect Size In-home at baseline and Wave 3 (n=536) 2.1 (.39) 1.0* (.23) .16 Out-of-home at baseline and 18 months (n=161) 7.2 (2.2) 3.1** (1.9) .21 2.8 (.38) 1.3*** (.25) .54 Setting Total (n=848)^ ^Total includes children in mixed placement settings p<.05**, p<.01***, p<.001 Predictors of Change in Well-Being for Multivariate (GEE) Models • • • • • • • • • • • • • Age (at Baseline) Gender Race/Ethnicity: Black, White, Hispanic, Other Urbanicity: Urban, Nonurban Child Setting: In-home, Out-of-home, Mixed Most Serious Maltreatment Type: Physical, Sexual, Failure to Provide (FTP), Failure to Supervise (FTS), Other Parent Cumulative Risk Score: Low, Medium, High Change in Parental Figure in 18 months (Y/N) Prior CWS History (Y/N) Chronic Health Problem (Y/N) Ratio of Children to Adults in Household (continuous) Poverty Rate (continuous) HOME-SF Score (continuous) Infants: Other Significant Findings • BINS: victims of sexual abuse comprised the only maltreatment type subgroup at higher risk at 18-months • VABS: children in out-of-home care have a greater decline in this measure than inhome children or children in mixed settings Summary: Age 0-2 • No significant measured improvements in development for infants • In general, infants < 2 years decline in all measures, those 25-35 months improve • Children with lower HOME-SF scores see greater declines in three of the four measures • Children in nonurban PSUs see higher risk for developmental delay and neurological impairment and worsening language skills • Males decline in cognitive development and social skills Toddlers: Other Significant Findings • SSRS: children in mixed settings exhibited a large decline in social skills, significantly so compared with the relatively stable skills of in-home children • PLS-3: victims of Other abuse exhibited a decrease, while children in all other abuse type groups exhibited an increase Summary: Age 3-5 • Slight decline in social skills; improvement in language skills; stable level of problem behavior • Age in months is a significant predictor of change, but not in a consistent direction • Prior CWS history is a predictor of change for both social and language skills – Could be that they receive greater level of intervention, this time – Could be that prior involvement already raised the level of their care or treatment School-Age Children: Other Significant Findings • CBCL: Being male, living in nonurban areas, and more poverty are associated with greater decreases in problem behavior • MBA-Math: Children with low parent cumulative risk and those in mixed settings exhibited increases, in contrast to their counterparts Summary: Age 6-10 • Only age group that showed improvements, although slight, in all developmental measures examined • Only age group where age is not a significant predictor of rate of change for any domain • Maltreatment type is the only significant predictor across more than one domain, yet with varied results Maltreated Adolescents Risky and Risk-Taking Behaviors Problem Behaviors • Approximately 40% of maltreated adolescents have borderline/clinical levels of problem behavior, compared to only 5% of children in the general population (Achenbach, 1991) • Maltreated adolescents need assistance in dealing with more than the maltreatment incident (e.g., aggression, attention problems) Delinquency • Delinquency is fairly stable but 6% of youth are reporting consistently high levels of serious/violent behaviors • Confirms other research (see Loeber & Farrington, 1998) that a small proportion of youth are committing the most serious/violent offenses (e.g., gang fights, robbery, rape) Risky Sexual Behavior • Youth living in out-of-home care are reporting more risky sexual behavior. • Probably attributable to the fact that out-ofhome youth are often removed from very high-risk homes (Carpenter, Clyman, Davidson, & Steiner, 2001). Are youth living in out-of-home care being monitored sufficiently? How can we assist youth in out-of-home care to engage in less unsafe sex? Substance Abuse • A small portion (4%) of youth are reporting consistently high levels of substance abuse and 15% report high use at 18 months. • Higher achievement may serve as protection against increases in substance use for maltreated youth. How can we explain the increase in the probability of substance abuse that nonaggressive youth are reporting? Suicide Risk Behavior • Youth in a mixture of placements are experiencing more increases in suicide risk behavior. – What does this finding tell us? • Could be attributable to factors related to placement moves over the 18 months. • Race/ethnicity differences appear somewhat different from national trends in suicide (CDC, 2004) but NSCAW is not measuring actual suicides. Summary of Well-Being Findings NAPCWA told us that child welfare agencies were not in control of enough resources to achieve gains in wellbeing…….. they were prescient. Cognitive Well-Being over 18 Months • • • • Worsened since BL for children 0-2 yrs Improved for children 3-5 and 6-10 yrs Males ≤ 5 yrs doing worse than females ≤ 5 yrs Generally higher for White than non-White children • Abuse type has more effect on infants than older children • Poverty associated with lower cognitive wellbeing for youngest (0-2 yrs) and oldest (11-15 yrs) children Social Well-Being over 18 Months • Worsened since BL for children 0-2 yrs • For children aged 3-5 and 6-10 yrs, social skills for : • Non-White children > White children • Children with low family cumulative risk > for children with higher family cumulative risk • For children aged 6-10 yrs and 11-15 yrs, social skills for: • IH children > OOH children • Above poverty > Below poverty Behavioral Well-Being over 18 Months • Behavior showed significant improvement over time for 6- to 10-year-olds only • For children aged 3-5 and 6-10 yrs, behavior problems for : • Males > females • White children > non-White children • Children with high family cumulative risk > for children with lower family cumulative risk • High levels of substance abuse were associated with more problem behavior (11-15 yrs) Risky Behavior over 18 Months •Delinquent behavior was fairly stable over 18 months •Substance abuse levels were fairly stable over 18 months •Voluntary risky sexual behavior increased •Suicidal behavior decreased Infant Development over 18 Months BDI Children at 50-99% poverty had significantly lower cognitive development scores than children at 150-199% and 200%+ poverty. BINS The risk of developmental delays & neurological impairments worsened over 18 months for infants. This was particularly the case for: •African American children compared to White children. •Children at <50% poverty compared to children at 150-199% and 200%+ poverty. •HOME-SF (Home environment) was used as predictor in these models Cognitive Well-Being over 18 Months • • • • Worsened since BL for children 0-2 yrs Improved for children 3-5 and 6-10 yrs Males ≤ 5 yrs doing worse than females ≤ 5 yrs Generally higher for White than non-White children • Abuse type has more effect on infants than older children • Poverty associated with lower cognitive wellbeing for youngest (0-2 yrs) and oldest (11-15 yrs) children Conclusions: Re-Report • Although the majority of re-reports are not substantiated, about one-in-five children have at least one re-report over the 18 months • Children in out of home care still have some risk of recurrent maltreatment – Possible explanations for maltreatment include: • occurred prior to child entering foster care • occurred during visit with biological family • child on child maltreatment in foster or group home • Receipt of parenting services associated with increased likelihood or re-report – Possible explanations include: • Families with greater needs selected into services • Agency surveillance • Services do not adequately family needs Caregiver Report of Violent Parenting Tactics • Many caregivers (8%) report using severe violence toward their child following child welfare involvement • A large proportion of severe violence remains unreported. This is especially true for infants and toddlers. • Violence between intimate partners often leads to an increase in the amount of severe violence children experience Implications • Parenting services – Rigorous evaluation needed – Developmentally appropriate • Linkages to ongoing family support services – Assist families to address ongoing needs – Early intervention services, as required by CAPTA 2003 • Child welfare workers must identify and intervene to address violence toward caregivers General Discussion • We are not achieving what I had hoped—at least in the shortterm—regarding children’s well-being – Out of home care has changed (see next slide) • Our models of out of home care may not be working the way they once had (assuming that prior research in NYC and San Diego was correct that foster care is restorative) – Services are not used or don’t help Alternate Explanations for Findings • PSM did not match for important unobserved covariates • Services may not have been used in full • Substance abuse services may interfere with parental adequacy – Focus is on parent’s recovery not child’s welfare – Time and effort for SAT can be burdensome to parent • Services may result in greater surveillance which results in more observed behaviors that might place children at risk, thus more reports – But there was also a tendency for more placements into foster care (p < .10). Caregiving Environments Have More Commitment but Fewer Resources • Many children in out-of-home care live below the poverty line • Many children in out-of-home care live in large households or with single parents (and sometimes both) • Many children in out-of-home care live with caregivers without a HS education Changes in the “Foster Care” Model Agency Resources Agency Resources Kinship Family Social Capital Foster Family Social Capital Commitment to Child Commitment to Child Caregiving Caregiving General Discussion (continued) • Findings are consistent with other research that children in foster care have serious developmental risks • They receive substantial levels of service, although they are still underserved – Children with the most significant problems receive the most clinical mental health services, although only between a third and half of children with a clinical CBCL score receive specialty mental health services. – Young children at high risk of developmental problems are not routinely referred for supplementary or special education—especially if they are in kinship care. – Children in non-kinship and group care receive high levels of supplementary educational services. • The services may not be what they need or be sufficient, or both A Needed Change in Focus • Service Access • Foster Family as Resource • Substance Abuse Treatment as Resource to Mothers (it may still be protective of children) • More voluntary and flexible services • Service Quality • Foster Family as Recipient of Resources • Substance Abuse Treatment as Risk for Mothers (it may still be protective of children) • More voluntary, flexible, and family focused services Summary of Findings: Top 20 1. Significant developmental needs of children receiving CWS at home are evident across many domains and not often addressed, especially among young children (US DHHS, 2005, US DHHS, 2003, and Stahmer, et al, in press) 2. The diversity in apparent reasons for entering care is considerable and does not always include severe maltreatment (US DHHS, 2005 and Barth et al, in press (a)) 3. There is considerable prior CWS involvement--this is one of the best predictors of many service and developmental outcomes (US DHHS, 2005) 4. Mental health problems of mothers are very common (US DHHS, 2005) Summary of Findings II 5. Substance abuse among mothers was less common than expected (US DHHS, 2005 and Gibbons et al., in press) 6. Domestic violence in families entering CWS is frequent, but relatively few placements among those cases (US DHHS, 2005, Kohl, et al. in press, Kohl et al, in press) 7. Many foster families have incomes at 100% of the poverty rate or lower (US DHHS, 2005, US DHHS, 2003 Report, and Barth et al., in press (b)) 8. Large (5 or more children) nonkinship foster families are common [about 1/3rd of all nonkinship homes] (US DHHS, 2003, US DHHS, 2005, and Summary of Findings III 9. Caregiving environments for children in out of home care are generally not stimulating (US DHHS, 2005 and Barth et al., in press (b)) 10. Mental health services to children with behavioral problems were fewer than expected, given prior research on the extensive cost of mental health services to foster children (US DHHS, 2005 and Burns, et al., in press) 11. African American children with serious mental health problems are served at rates that are comparable to white children but African with fewer problems get less preventative mental health care (Leslie, et al., 2004). 12. Mental health services that are closely coordinated with CWS appear to reduce the extent of underservice for black children (Hurlburt, et al., in press) Summary of Findings IV 13. Almost every relationship between case characteristics and services vary significantly by the age of the child (US DHHS, 2005, US DHHS, 2003, Burns et al., in press) 14. Less service use by children in kinship care—especially among younger children (US DHHS, 2003; 2005) 15. Caregiver evaluations of CWWs are more positive than caregiver evaluation of services (US DHHS, 2005, Chapman et al., 2003) 16. Children in out of home care generally (>80%) report feeling close to their caregivers (US DHHS, 2005, Chapman, et al., 2004); children in group care are one important exception. Summary of Findings V 17. Substance abuse and domestic violence by caregivers (selfreport) are often not known to CWWs (US DHHS, 2005, Gibbons & Barth., in press; Hazen, et al., in press) 18. Termination of parental rights almost always follows reunification efforts—reunification bypasses are not common (Barth, Wulczyn, & Crea, in press). 19. At 18-months, about one-third of children are receiving care in multiple care sectors (i.e., special education and specialty mental health) (Farmer et al., under review) 20. The substantiation status of sexual abuse allegations explains service rates more so than children's exhibited needs (McCrae, Chapman, & Christ, in press). References I Barth, R.P., Wildfire, J., & Green, R. L. (in press (a)). Placement into foster care and the interplay Nof urbanicity, child behavior problems, and poverty. American Journal of Orthopsychiatry. Barth, R. P., Green, R., Wall, A., Webb, M. B., Gibbons, C., & Craig, C. D. (in press (b)).Characteristics of out-of-home caregiving environments provided under child welfare services. Child Welfare. Barth, R.P., Wulczyn, F. & Crea, T. (in press (c)). Adoption from foster care since the Adoption and Safe Families Act. Journal of Law and Social Policy. Burns, B.J., Phillips, S.D., Wagner, H.R., Barth, R.P., Kolko, D.J., & Campbell, Y. (2004). Mental health need and access to mental health services by youth involved with child welfare. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 960970. Chapman, M. V., Wall, A., & Barth, R.P. (2004). Children's voices: The perceptions of children in foster care. American Journal of Orthopsychiatry, 74(3), 293-304. Chapman, M. V., Gibbons, C, B., Barth, R.P., & McCrae, J.S. (2003). Parental views of inhome services: What predicts satisfaction with child welfare workers?, Child Welfare, 82(5), 571-596. Farmer, E.M.Z., Mustillo, S.A., Wagner, H.R., Burns, B.J., Kolko, D.J., Barth, R.P., et al. (under review). Multi-sector service use by youth in contact with child welfare. Gibbons, C., & Barth, R.P. (in press). Prevalence of substance abuse among in-home caregivers in a U.S. child welfare population: Caregiver vs. child welfare worker report. Child Abuse & Neglect. Gibbons, C., Barth, R.P., & Martin, S. (under review (a)). Characteristics of substance-abusing mothers involved with child welfare services. Gibbons, C., Barth, R.P., & Martin, S. (under review (b)). Substance abusing mothers in child welfare:Who gets treatment? References II Hazen, A., Connelly, C.D., Kelleher, K., Landsverk, J., & Barth, R.P. (in press). Intimate partner violence among female caregivers of children reported for child maltreatment. Child Abuse & Negect. Hurlburt, M.S., Leslie, L.K., Landsverk, J., Barth, R. P., Burns, B. J., Gibbons, R.D., et al. (in press). Contextual predictors of mental health services use among a cohort of children open to child welfare services. Archives of General Psychiatry. Kohl, P.L., Barth, R.P., Hazen, A.L., & Landsverk, J.A. (in press). Child welfare as a gateway to domestic violence services: Findings from the National Survey of Child and Adolescent Well-Being. Children & Youth Services Review. Kohl, P.L., Edleson, J.L., English, D.J., & Barth, R.P. (in press). Domestic violence and pathways into child welfare services: Findings from the National Survey of Child and Adolescent Well-Being. Children & Youth Services Review. Leslie, L. K., Hurlburt, M. S., Landsverk, J., Barth, R., & Slymen, D.J. (2004). Outpatient mental health services for children in foster care: a national perspective. Child Abuse and Neglect, 28(6), 697-712. McCrae, J., Chapman, M. V., & Christ, S.L. (in press). Profile of children investigated for sexual abuse, psychopathology, and services. American Journal of Orthopsychiatry. Stahmer, A.C., Leslie, L. K., Hurlburt, M., Barth, R.P., Webb, M.B., Landsverk, J., et al. (in press).Developmental and behavioral needs and service use for young children in child welfare. Pediatrics. U.S. Department of Health and Human Services Administration for Children and Families. (2005). National Survey of Child and Adolescent Well-Being: Children involved with the child welfare services (Baseline Report). Washington, DC, ACF, US DHHS. U.S. Department of Health and Human Services Administration for Children and Families (2003). National Survey of Child and Adolescent Well-Being: Children living for one year in foster care. Washington, DC, ACF, US DHHS