Cultural Competence
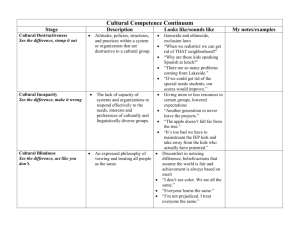
advertisement

CULTURAL COMPETENCE IN PUBLIC HEALTH (OR ANYWHERE ELSE) Robert Lucio, Ph.D., MSW College of Public Health Department of Community and Family Health College of Behavioral & Community Sciences Department of Child and Family Studies 2010 Cultural Competence Seminar Tampa, FL – December 03, 2010 Purpose What is culture? Why is culture important to health? What is cultural competence? What is meant by the concept of “health disparities?” To share a framework for building organizational cultural competence Assumption Underlying The Training Culture and society play pivotal roles in health, illness, and health services Understanding the wide-ranging roles of culture and society enables the health field to design and deliver services that are more responsive to the needs of culturally and linguistically diverse people Cultural Competence Starts with the recognition & awareness of one’s own Biases/Prejudices Culture Exercise Know your potato What Is Culture? Culture has been defined in various ways by different disciplines and for numerous purposes (Kao, Hsu, & Clark, 2004) Culture represents the histories, attitudes, behaviors, languages, values, beliefs and uniqueness, which distinguished each racial or sub-cultural group in a society. Each of us has a historical heritage and a contemporary heritage that comprise our present culture (Coggins, 2004) What Is Culture? Culture is the customs, beliefs, values, knowledge, and skills that guide people along shared paths (Linton, 1947) Culture is reflected in the social norms, mores, sanctions, and in the art, history, folklore, and institutions of a group of people The term culture refers to the way of life of people and includes the tools or methods by which they extract a livelihood from their environment (Corsini, 1987) Maslow’s Hierarchy Of Needs: Humanistic Theory Self Actualization Esteem and Identity Love and Belonging Safety and Security Physiologic (e.g., Food, Water) (Cross, Bazron, Dennis, & Isaacs, 1989) Why is culture important? Background Culture has been conceptualized as either a static trait characteristic of a group of people or a dynamic process. Static – People are subjected to cultural structures and are seen as passive carriers of culture inter-generationally. Dynamic process – People are seen as more active learners of their cultures. (Kao, Hsu, & Clark, 2004) Seeing Culture Culture is omnipresent and frequently invisible, especially to those enmeshed within a particular culture Since one is born into a culture, one experiences that culture as always already there, part of the world that one sees, not as a way of seeing the world (Steeves & Kahn, 1995, p. 183) Underlying Assumptions Everyone in the room has a culture Understanding your own culture is key Culture influences most, if not all aspects of human social interactions Although culture is omnipresent, it is frequently invisible, especially to those enmeshed within a particular culture. What is culture? Material Culture What we see Immaterial Culture Hidden Culture Artifacts Myths Language Folklore Dress Stories Behaviors Feelings Color Values Food Oral Culture Songs Spiritualism (Coggins, 2010) Why Culture is Important The dramatic change in our nation’s ethnic composition is altering the way we think about ourselves The deeper significance of America’s becoming a majority nonwhite society is what it means to the national psyche, to individuals’ sense of themselves and their nation – their (our) idea of what it is to be American (Takaki, 1993) American society is increasingly diversified. The federal funding agencies require participation of multicultural populations for health research Why Culture is Important Hispanic and Latino Americans accounted for almost half (1.4 million) of the national population growth of 2.9 million between July 1, 2005, and July 1, 2006 Immigrants and their U.S.-born descendants are expected to provide most of the U.S. population gains in the decades There are 45.5 million Hispanics living in the United States, accounting for 15 percent of the U.S. population Blacks comprise the second-largest minority group, with 40.7 million (13.5 percent), followed by Asians, with 15.2 million (5 percent). (The Office of Minority Health, 2010) Why is culture important Colors Perhaps explaining why some native English-speaking children, familiar with the rainbow of colors in the Crayola 64-pack, actually can tell “rust” from “brick” or “moss” from “sage,” while children who grow up speaking languages with fewer color names lump such hues together (Namibia) Math Skills The lack of number-words seems to preclude the ability to entertain concepts of exact number in certain cultures (Pirahã) Dingfinger, S. F. (2005). Fuzzy Math. Monitor on Psychology, 36(2), 30-31. Adelson, R. (2005). Hues and Views. Monitor on Psychology, 36(2), 26-29 Why is culture important? Intelligence Intelligence cannot be fully or even meaningfully understood outside its cultural context. Research that seeks to study intelligence without considering the context risks the imposition of an investigator’s world-view on the rest of the world. Moreover, research on intelligence within a single culture may fail to do justice to the range of skills and knowledge that may constitute intelligence broadly defined and risks drawing false and hasty generalizations. Sternberg, R. (2004). Culture and Intelligence. American Psychologist, 59, 325-338. Why is culture important? Intelligence and Development Some things are constant across cultures (mental representations and processes), whereas others are not (the contents to which they are applied and how their application is judged) African infants sit and walk earlier than do their counterparts in the United States and Europe Sternberg, R. (2004). Culture and Intelligence. American Psychologist, 59, 325-338. Why is culture important? Behavior Behavior that in one cultural context is smart may be, in another cultural context, stupid (Cole, Gay, Glick, & Sharp, 1971) Stating one’s political views honestly and openly, for example, may win one the top political job, such as the presidency, in one culture and the death penalty in another Sternberg, R. (2004). Culture and Intelligence. American Psychologist, 59, 325-338. Why is culture important? health, healing, and wellness belief systems; how illness, disease, and their causes are perceived; both by the patient/consumer the behaviors of patients/consumers who are seeking health care and their attitudes toward health care providers as well as the delivery of services by the provider who looks at the world through his or her own limited set of values, which can compromise access for patients from other cultures Why is culture important? The increasing population growth of racial and ethnic communities and linguistic groups, each with its own cultural traits and health profiles, presents a challenge to the health care delivery service industry in this country The provider and the patient each bring their individual learned patterns of language and culture to the health care experience which must be transcended to achieve equal access and quality health care Some Points to Remember About Cross-Cultural Relationships What seems to be right, logical, sensible, important, or obvious to a person in one culture may seem wrong, irrational, silly, unimportant, or confusing to someone in another culture When people talk about cultures, they tend to emphasize the importance of differences and tend to neglect explaining human commonalities Differences between cultures are too often perceived as threatening or bothersome and are described in negative terms Cultural Competence A class divided A class divided part I A class divided part II Definition Of Cultural Competence The ability to work effectively across cultures in a way that acknowledges and respects the culture of the person or organization being served “Cultural Competence” is a set of congruent behaviors, attitudes, and policies that come together in an agency that enables employees to work effectively in cross-cultural situations J. H. Hanley (1999) - Beyond the tip of the Iceberg: Five Stages toward cultural competence Hernandez, M. Nesman, T., Isaacs, M., Callejas, L. M., & Mowery, D. (Eds.). (2006). Examining the research base supporting culturally competent children’s mental health services. Tampa, FL: USF, Louis de la Parte Florida Mental Health Institute, Research & Training Center for Children’s Mental Health. Online at: http://rtckids.fmhi.usf.edu/rtcpubs/CulturalCompetence/services/CultCompServices.pdf Cultural Competence Continuum Cultural Proficiency (Level 6) Culture Competence (Level 5) Cultural Pre-Competence (Level 4) Cultural Blindness (Level 3) Cultural Incapacity (Level 2) Cultural Destructiveness (Level 1) (Coggins, 2010) Cultural Destructiveness “See the difference; stomp it out.” Using one’s power to eliminate the culture of another. Represented by attitudes, policies, and practices that are destructive to cultures and the individuals within the culture. Examples Genocide or Ethnocide Exclusion Laws English only Speaking laws Forms not available in another language Denying clients access to their natural healers. Shun/Avoid certain curriculum topics Dress policies that single out specific ethnic groups Cecil County Public Schools Cultural Destructiveness “See the difference; stomp it out.” What you might hear “When we redistrict we can get rid of THAT neighborhood!” “Why are those kids speaking Chinese here?” “There are so many problems coming from Southside.” “If we could get rid of the special needs students, our scores would improve.” Cecil County Public Schools Cultural Incapacity “See the difference; make it wrong.” Believing in the superiority of one’s own culture and behaving in ways that disempower another’s culture Examples Lacks the capacity or will to help minority clients and employees Disproportionate allocation of resources to certain groups Lowered expectations Expecting “others” to change: My way or the highway Practices of discrimination in hiring and promotion; Subtle messages that some cultural groups are neither valued nor welcomed Sending away domestic violence victims in Albuquerque from a hospital to Indian health clinic Lack of an equal representation of staff/administrators that reflect diversity Cecil County Public Schools Cultural Incapacity “See the difference; make it wrong.” What you might hear “Another generation to never leave the trailer park.” “His mom admitted he was special education when she went to school, so we can’t expect him to do well” “The apple doesn’t fall far from the tree.” Cecil County Public Schools Cultural Blindness “See the difference; act like you don’t.” Acting as if cultural differences do not matter or as if there are not differences among or between cultures Examples Beliefs/actions that assume world is fair and achievement is based on merit Color or culture make no difference and that all people are the same. Ignores cultural strengths Believes that the helping approaches by dominant culture are universally acceptable and applicable Encourages assimilation; thus, those who don’t are isolated Blames victim for their problems Views ethnic minorities as culturally deprived Using light colored band aids in hospitals that are marked as flesh colored (but only Cecil County Public Schools to fair skinned people) Cultural Blindness “See the difference; act like you don’t.” What you might hear “Our organization does not need to focus on multicultural educationwe have no diversity” “We treat everyone the same” “That isn’t a problem in our organization” “Just don’t recognize their religion. We don’t want to offend” “I’m not prejudiced. I don’t see color ” Cecil County Public Schools Cecil County Public Schools Cultural Pre-Competence “See the difference; respond to it inappropriately.” Recognizing the limitations of one’s skills or an organization's practices when interacting with other cultural groups. Examples Delegate diversity work to others, to a committee Quick fix, packaged short-term programs What can we do?” Desire to deliver quality services; commitment to civil rights. Realizes its weaknesses and attempts to improve some aspect of their services. Explores how to better serve minority communities. Agency may believe that their accomplishment of one goal or activity fulfills their obligation to minority communities; may engage in token hiring practices. Often only lacks information on possibilities and how to proceed May feel a false sense of accomplishment that prevents further movement. Cultural Pre-Competence “See the difference; respond to it inappropriately.” What you might hear “I’ll do my best to make the Special Education student feel part of the Honors course.” “Make sure you do an activity for Black History month.” Cecil County Public Schools Cultural Competence “See the difference; understand the difference that difference makes.” Interacting with others using the five essential elements of cultural proficiency as the standard for behavior and practice. Examples Acceptance and respect for difference. Expands cultural knowledge and resources. Continuous self-assessment. Pays attention to dynamics of difference to better meet client needs. Variety of adaptations of service models. Seeks advice and consultation from the minority community. Commits to policies that enhance services to diverse clientele. Advocacy On-going education of self and others Adapts evidence based promising practices that are culturally and linguistically competent. Cecil County Public Schools Cultural Competence “See the difference; understand the difference that difference makes.” What you might hear “I think it is interesting to look at another’s perspective through another lens.” Cultural Proficiency “See the difference; respond positively. Engage and adapt.” Esteem culture; knowing how to learn about organizational culture; interacting effectively in a variety of cultural groups. Examples Holds cultures in high esteem. Agency seeks to add to its knowledge base. Agency advocates continuously for cultural competence throughout the system. Differentiate to the needs of all patients. Cultural Empowerment is reflected in a philosophy that the client/staff are co-equal partners in the treatment and learning process Cecil County Public Schools Cultural Proficiency “See the difference; respond positively. Engage and adapt.” What you might hear “With the addition of _____, our staff experience has become richer. The other employees are learning from him also.” “Thank you for talking to the patients and explaining in Spanish about our services.” Cecil County Public Schools Essential Elements of Cultural Competence The culturally competent system of care is made up of culturally competent institutions, agencies, and professionals. Five essential elements contribute to a system’s, institution’s, or agency’s ability to become more culturally competent. The culturally competent system would: Cross, Bazron, Dennis, & Isaacs, (1989). Towards a culturally competent system of care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed: Volume I Washington, DC: Georgetown University Child Development Center. Value diversity; Have the capacity for cultural self-assessment; Be conscious of the dynamics inherent when cultures interact; Institutionalize cultural knowledge; and Develop adaptations to diversity Organizational Cultural Competence A Value Base for Cultural Competence Respects the unique, culturally-defined needs of various client populations. Acknowledges culture as a predominant force in shaping behaviors, values, and institutions. Views natural systems (family, community, church, healers, etc.) as primary mechanisms of support for minority populations and are different for various subgroups Starts with the “family,” as defined by each culture, as the primary and preferred point of intervention. Believes that diversity within cultures is as important as diversity between cultures. Acknowledges and accepts that cultural differences exist and have an impact on service delivery. Acknowledges that when working with minority clients process is as important as product. Cross, Bazron, Dennis, & Isaacs, (1989). Towards a culturally competent system of care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed: Volume I Washington, DC: Georgetown University Child Development Center. A Value Base for Organizational Cultural Competence Culturally competent agencies are characterized by acceptance of and respect for difference continuing self-assessment regarding culture, careful attention to the dynamics of differences continuous expansion of cultural knowledge and resources, and adaptations of service models. Culturally competent agencies work to hire unbiased employees and seek advice and consultation from their clients; They seek staff who represent the racial and ethnic communities being served and whose self-analysis of their role has left them committed to their community and capable of negotiating a diverse and multicultural world. Culturally competent agencies understand the interplay between policy and practice, and are committed to policies that enhance services to diverse clientele. Cross, Bazron, Dennis, & Isaacs, (1989). Towards a culturally competent system of care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed: Volume I Washington, DC: Georgetown University Child Development Center. Background A foundational definition for cultural competence states that it includes behaviors, attitudes, and policies within a system, agency, or among professionals that enable them to work effectively in cross-cultural situations (Cross, Bazron, Dennis, & Isaacs, 1989) Underlying the definition by Cross et al. (1989): Children’s health services must acknowledge and incorporate the importance of culture, race, and ethnicity at all levels of functioning and treatment to provide optimal access to quality services The recognition that culture, race, and ethnicity have significant influence on the behavior and thinking of providers and service recipients is an important feature of cultural competence. Defining Organizational Cultural Competence Operationalizing cultural competence is an important step toward being able to test its effectiveness in improving health service delivery. A definition of organizational cultural competence and conceptual model were developed by Hernandez and Nesman (2006) based on a thematic analysis conducted for a literature review and protocol assessment. Implementation-focused Definition of Cultural Competence Within a framework of addressing health disparities, the level of a human service organization’s/system’s cultural competence can be described as the degree of compatibility and adaptability between the cultural/linguistic characteristics of a community’s population AND the way the organization’s combined policies and structures/processes work together to impede and/or facilitate access, availability, and utilization of needed services/supports (Hernandez & Nesman, 2006) Conceptual Model for Accessibility of Health Services to Culturally/Linguistically Diverse Populations Definition: Within a framework of addressing health disparities within a community, the level of a human service organization’s/system’s cultural competence can be described as the degree of compatibility and adaptability between the cultural/linguistic characteristics of a community’s population AND the way the organization’s combined policies and structures/processes work together to impede and/or facilitate access, availability and utilization of needed services/supports (Cross, Bazron, Dennis, & Isaacs, 1989; Siegel, 2004; CMHS, 1997). Degree of compatibility defines level of organizational/systemic cultural competence Community Context Cultural/Linguistic characteristics of a community’s population Compatibility Outcomes: Reducing health disparities Organization’s/System’s Infrastructure Domain/ Functions Direct Service Domain/ Functions (Hernandez & Nesman, 2006) Conceptual Model for Accessibility of Health Services to Culturally/Linguistically Diverse Populations Degree of compatibility defines level of organizational/systemic cultural competence Community Context Cultural/Linguistic characteristics of a community’s population Compatibility Organization’s/System’s combined policies, structures, and processes The compatibility between the organization’s/system’s Outcomes: Reducing health disparities structures and processes and the community’s populations determines the level of organizational cultural competence. The model shows the need to adapt an organization’s structures and processes to the characteristics of the community being served. Compatibility between the community’s populations and organizational structures and processes are determined by the level of access and utilization of appropriate services. (Hernandez & Nesman, 2006) Community Context Important in the development of compatibility between organizations and populations served. Based on the recognition that children/adolescents and their families respond to health problems and concerns within a context of the larger social environment that guides or pushes them toward or away from various types of services. Also recognizes that organizations and systems function within larger community, state, and national contexts that impact their attempts to serve their local community. (Hernandez & Nesman, 2006) Characteristics of the Community Population Assessing compatibility (cultural competence) is dependent on having information about the community’s populations, context, and the organization’s policies, structures, and processes. Cultural/Linguistic characteristics of a community’s population This includes awareness of the influences of culture, ethnicity, race, socioeconomic status, and related social factors on the provision of services and help-seeking. Compatibility Important to link interventions the factors that contribute to a lack of engagement and to recognize that these factors will vary across groups and service types (Staudt, 2003). Development of compatible strategies will not be possible without this information. An organization’s/system’s combined policies, structures and processes (Hernandez & Nesman, 2006) Characteristics of the Community Population Cultural/Linguistic characteristics of a community’s population Facilitators Cultural View of Health: The common perception of health that is related to the culture and facilitates service use History: History of the community or population and the effects of that history Language Characteristics: Primary language of the population Resource Characteristics: Resources of the population Strength Characteristics: Strengths of the population Compatibility An organization’s/system’s combined policies, structures and processes (Hernandez & Nesman, 2006) Characteristics of the Community Population Inhibitors Cultural/Linguistic characteristics of a community’s population Cultural View of Health: Common cultural perceptions of health that present barriers to service use Need Characteristics: Needs of the population Compatibility An organization’s/system’s combined policies, structures and processes (Hernandez & Nesman, 2006) Domains of Organizational Cultural Competence Infrastructure Domain/Function Direct Service Domain/Function Cultural/Linguistic characteristics of a community’s population Compatibility • Organizational Values • Policies/Procedures/ Governance • Planning/Monitoring/ Evaluation Compatibility between the • Communication infrastructure and direct • Human Resources service functions of an Development organization • Community & Consumer Participation • Facilitation of a Broad Service Array • Organizational Infrastructure/ Supports Access Infra- Direct structure Service The ability to enter, navigate, and exit appropriate services and supports as needed Utilization Availability The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence Infrastructure Domain/Function Direct Service Domain/Function • Organizational Values • Policies/Procedures/ Governance • Planning/Monitoring/ Evaluation Compatibility between the • Communication infrastructure and direct • Human Resources service functions of an Development organization • Community & Consumer Participation • Facilitation of a Broad Service Array • Organizational Infrastructure/ Supports Access The ability to enter, navigate, and exit appropriate services and supports as needed Utilization The rate of use or usability of appropriate health services Availability Having services and supports in sufficient range and capacity to meet the needs of the populations they serve To better illustrate the conceptual model, a more detailed diagram (pictured here) was developed to show the direct link between the organizational infrastructure level and the direct service level. (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence Direct Service Domain/Function Infrastructure Domain/Function • Organizational Values • Policies/Procedures/ Governance • Planning/Monitoring/ Evaluation Compatibility between the • Communication infrastructure and direct • Human Resources service functions of an Development organization • Community & Consumer Participation • Facilitation of a Broad Service Array • Organizational Infrastructure/ Supports The Access The ability to enter, navigate, and exit appropriate services and supports as needed Availability Utilization The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve left triangle highlights the infrastructure component, which includes organizational functions that are based on the domains identified in through an analysis of cultural competence protocols. Organizational/System Implementation Domains for Improving Cultural Competence • • • • • • • • Infrastructure Domain/Function Organizational Values Policies/Procedures/ Governance Planning/Monitoring/ Evaluation Communication Human Resources Development Community & Consumer Participation Facilitation of a Broad Service Array Organizational Infrastructure/ Supports (Hernandez & Nesman, 2006) The Infrastructure domain is made up of multiple functions that are typical of organizations, each of which must be adapted for cultural competence. Organizational values, policies, procedures and governance contribute to cultural competence when they promote compatibility with the community served and provide support for staff to carry out needed culturally competent service practices. Likewise, planning and evaluation processes contribute to cultural competence when they include communities of color as fully contributing partners with shared responsibilities, and when they collect data that reflects the diversity of the community. Organizational/System Implementation Domains for Improving Cultural Competence Communication that supports cultural competence includes two-way communication and learning within the organization and between the organization and the community. • • • • • • • • Infrastructure Domain/Function Organizational Values Policies/Procedures/ Governance Planning/Monitoring/ Evaluation Communication Human Resources Development Community & Consumer Participation Facilitation of a Broad Service Array Organizational Infrastructure/ Supports Human resources and service array domains include strategies to increase bilingual/bicultural capacity, recruitment, and retention, and availability of services that are appropriate and of high quality for the target population. Methods of outreach to communities and opportunities for community/consumer participation are important mechanisms that can lead to greater compatibility. Organizational infrastructure can promote cultural competence by bringing in financial, technological and other needed resources. (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence Infrastructure Domain/Function The • Organizational Values • Policies/Procedures/ Governance • Planning/Monitoring/ Evaluation Compatibility between the • Communication infrastructure and direct • Human Resources service functions of an Development organization • Community & Consumer Participation • Facilitation of a Broad Service Array • Organizational Infrastructure/ Supports right triangle highlights the direct service domain, which includes aspects of access, availability, and use of services. Findings are based an analysis of literature related to services for racially/ethnically diverse children and families. Direct Service Domain/Function Access The ability to enter, navigate, and exit appropriate services and supports as needed Availability Having services and supports in sufficient range and capacity to meet the needs of the populations they serve Utilization The rate of use or usability of appropriate health services Organizational/System Implementation Domains for Improving Cultural Competence Access is defined as mechanisms that facilitate entering, navigating, and exiting appropriate services and supports as needed. Availability is defined as having services and Direct Service Domain/Function Access The ability to enter, navigate, and exit appropriate services and supports as needed supports in sufficient range and capacity to meet the needs of the populations they serve. This may include availability of bilingual personnel and/or trained translators. Utilization Availability Utilization The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve is defined as the rate of use of services or their usability for populations served. Utilization may include issues such as length of time in service, retention, or dropout rates. (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence This model shows that there is a need for compatibility between the organizational infrastructure and direct service. It also highlights the need for compatibility between Direct Service Domain/Function Access The ability to enter, navigate, and exit appropriate services and supports as needed each of the direct service domains. Availability Dynamic relationships are shown by two-way arrows between infrastructure supports, access mechanisms, and availability of needed/ Utilization The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve appropriate services. (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence Direct Service Domain/Function An example of this relationship might be as follows: Access is increased through a one-stop family services center, but there is a lack of availability of bilingual services and lack of trust in the organization because it is not connected with the community. This lack of trust or bilingual capacity results in low levels of utilization of services and little improvement in outcomes. Access The ability to enter, navigate, and exit appropriate services and supports as needed Availability Utilization The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve (Hernandez & Nesman, 2006) Organizational/System Implementation Domains for Improving Cultural Competence Direct Service Domain/Function This relationship is especially important to recognize as organizations change. Changes in one area may affect other areas. Lack of change in one area may cancel out efforts in other areas. Incorporating cultural competence into every aspect of the organization or system requires careful consideration of compatibility of policies and strategies with the population served as well as with the other organizational functions. . Access The ability to enter, navigate, and exit appropriate services and supports as needed Availability Utilization The rate of use or usability of appropriate health services Having services and supports in sufficient range and capacity to meet the needs of the populations they serve (Hernandez & Nesman, 2006) Achieving Outcomes Statement of overall mission or desired change related to reducing disparities, or increasing access, availability, or utilization for specific racial/ethnic communities. Degree of compatibility Community Context (Hernandez & Nesman, 2006) Cultural/Linguistic characteristics of a community’s population Compatibility Organization’s/System’s Infrastructure Domain/ Functions Direct Service Domain/ Functions Outcomes Defining Disparities Health Disparities: Main Assumptions It is generally recognized that an individual’s helpseeking behavior style for health and mental health problems is linked to cultural and ethnic factors. The process of seeking help by various people of color, and the interactions that result with both formal and informal sources of help, serves as a filter that often discourages contact with health and mental health professionals. (Leong, et al. 1995) Mental Health Disparities: Main Assumptions Parents from various cultural backgrounds have been found to differ in the degree to which they identify child behavior and emotional problems as serious. Differences have also been found across cultural groups in their beliefs about whether these child problems are likely to improve in the absence of professional support. (Wiesz & Weiss, 1991) Maslow’s Hierarchy Of Needs: Humanistic Theory and Health Disparities Self Actualization Esteem and Identity Love and Belonging Safety and Security Physiologic (e.g., Food, Water) (Cross, Bazron, Dennis, & Isaacs, 1989) Examples of Disparities in Mental Health Children with mental health problems have lower educational achievement, greater involvement with the criminal justice system, and fewer stable and longer-term placements in the child welfare system than children with other disabilities. Striking disparities for people of color in mental health services despite having similar community rates of mental disorders. People of color have less access to mental health care than do whites. People of color are less likely to receive needed care When they receive it, it is more likely to be poor in quality. Children’s Mental Health Facts for Policymakers. By: Rachel Masi and Janice Cooper. Publication Date: November 2006. Online at: http://nccp.org/publications/pub_687.html#10. Examples of Disparities in Health African Americans In 2005, the death rate for African Americans was higher than Whites for heart diseases, stroke, cancer, asthma, influenza and pneumonia, diabetes, HIV/AIDS, and homicide. The infant mortality rate for African American mothers with over 13 years of education was almost three times that of Non-Hispanic White mothers in 2005. (The Office of Minority Health, 2010) Examples of Disparities in Mental Health Latinos/Hispanic Americans Hispanics have the highest uninsured rates of any racial or ethnic group within the United States. Hispanics have higher rates of obesity than nonHispanic Caucasians. Puerto Rican infants were twice as likely to die from causes related to low birthweight, as compared to nonHispanic white infants. (The Office of Minority Health, 2010) Examples of Disparities in Mental Health Asian American/Pacific Islanders Asian American women have the highest life expectancy (85.8 years) of any other ethnic group in the U.S. Life expectancy varies among Asian subgroups: Filipino (81.5 years), Japanese (84.5 years), and Chinese women (86.1 years). Asian/Pacific Islander men are twice as likely to die from stomach cancer as compared to the non-Hispanic white population, and Asian/Pacific Islander women are 2.6 times as likely to die from the same disease. (The Office of Minority Health, 2010) Examples of Disparities in Health American Indians/Alaska Natives American Indians and Alaska Natives have an infant death rate 40 percent higher than the rate for Caucasians American Indian/Alaska Native babies are twice as likely as non-Hispanic white babies to die from sudden infant death syndrome (SIDS) American Indian/Alaska Native babies are 30% more likely to die from complications related to low birth weight or congenital malformations compared to nonHispanic whites babies. (The Office of Minority Health, 2010) Barriers Associated with Disparities Across Ethnic, Racial, and Cultural Groups Income, Geographic Location, Language Managed Care, Medicare/Medicaid Stigma Lack of trust Insurance and related policies System bias and institutional racism Hernandez, M. Nesman, T., Isaacs, M., Callejas, L. M., & Mowery, D. (Eds.). (2006). Examining the research base supporting culturally competent children’s mental health services. Tampa, FL: USF, Louis de la Parte Florida Mental Health Institute, Research & Training Center for Children’s Mental Health. Online at: http://rtckids.fmhi.usf.edu/rtcpubs/CulturalCompetence/services/CultCompServices.pdf What is Meant by the Term “Disparity”? Gamble and Stone (2006) label the term disparity as descriptive: Used to explain differences in health status or access across population groups. In this sense, the term carries no moral nuance, implying neither rightness nor injustice. They use the term inequity to describe injustice/bias: What ought to be rather than what actually is. See: Gamble, V. N., & Stone, D. (2006). U.S. Policy on health inequities: The interplay of politics and research. Journal of Health Politics, Policy and Law, 31(1), 93-126. Definitions of Health Disparity Healthy People 2010 (2000): “…differences that occur by gender, race, or ethnicity, education, or income, disability, living in rural localities, or sexual orientation.” Institute of medicine (2002): “…racial or ethnic differences in the quality of health care that are not due to access-related factors or clinical needs, preferences and appropriateness of intervention.” See: Carter-Pokras, O., & Baquet, C. (2002). What is a "Health Disparity"? Public Health Reports, 117(5), 426-434. Health Focused Approach To Defining Disparities Eliminating Health Disparities Leads to focus on health Access Quality Problem is that social inequities exist and that there is a relationship between social inequities and health (Hernandez, 2009; Office of Minority Health , 2010) Aligned Approach: What are the implications for solutions to reducing health disparities? Problem with the single sector definition approach. For example, the presence of over-representation in other sectors Eliminating Health Disparities Over-representation in: Question then becomes how do these two areas come together? Child Welfare Education Negative Health and Birth Outcomes (Hernandez, 2009; Office of Minority Health , 2010) Aligned Approach: What are the implications for solutions to reducing health disparities? Eliminating Health Disparities How do these areas come together? Over-representation in Child Welfare: 35% of the children in foster care are African American, but they make up only 15% of the child population 39% of the children in foster care are Caucasian, while they represent 59% of the child population On September 30, 2003 over fifty percent (59% or 304,910) of the 523,085 children living in foster care placements were children of color, although they represented only 41% of the child population in the United States (Hernandez, 2009; Office of Minority Health , 2010) Aligned Approach: What are the implications for solutions to reducing mental health disparities? Eliminating Health Disparities How do these areas come together? Over- and Under-representation in Education: Among all students, African-American students are more likely to be suspended or expelled than their white peers (40% vs. 15%) African-American preschoolers were about twice as likely to be expelled as White and Latino preschoolers and over five times as likely as Asian-American preschoolers (Hernandez, 2009; Office of Minority Health , 2010) Aligned Approach: What are the implications for solutions to reducing mental health disparities? Eliminating Health Disparities How do these areas come together? Over- Representation in Poor Birth Outcomes: African American are 3 times more likely to have a baby die than white nonHispanic mothers American Indians and Alaska Natives have an infant death rate 40 percent higher than the rate for Caucasians. American Indian/Alaska Native babies are twice as likely as non-Hispanic white babies to die from sudden infant death syndrome (SIDS) (Hernandez, 2009; Office of Minority Health , 2010) Aligned Approach: What are the implications for solutions to reducing mental health disparities? Eliminating Health Disparities How do these areas come together? Over- Representation in Poor Health Outcomes: Hispanics have higher rates of obesity than non-Hispanic Caucasians. (Hernandez, 2009; Office of Minority Health , 2010) Why Is The Conversation So Confusing? When we talk about disparity issues, we often confuse sectors, their solutions, and their goals Holistic solutions are few since each sector focuses on it’s particular goals and solutions Solutions are elusive because the concerns and issues facing different populations are inter-connected What is the inter-relationship between sectors and the social concerns they are focused upon? (Hernandez, 2009) Why Is The Conversation So Confusing? Unrelated Solutions, Sectors, and Their Goals Health OverRepresentation Disparity Quality Appropriate Access Social control sectors, poor health outcomes Social Inequities UnderRepresentation EducationDrop-Out (Hernandez, 2009) Racism Economics Housing Transportation Aligned Approach Linked Goals Eliminating Health Disparities and Beyond Reducing OverRepresentation in Other Sectors This leads to planning and “solution making” that: Focuses on a community as a whole Focuses on the linkages across sectors (Hernandez, 2009) Aligned Approach Social Inequities: Economic, Job, Neighborhood Conditions, Chronic Stress, Housing, Education, Food Security, Social Policies, and Racism/Discrimination Reducing Over-Representation in Poor Health Outcomes Eliminating Health Disparities Linked Goals Reducing Over-Representation in Child Welfare Reducing Over- and UnderRepresentation in Education (Hernandez, 2009) Example Of A New Definition Lack of insurance coverage. Without health insurance, patients are more likely to postpone medical care, more likely to go without needed medical care, and more likely to go without prescription medicines. Minority groups in the United States lack insurance coverage at higher rates than whites. Lack of a regular source of care. Without access to a regular source of care, patients have greater difficulty obtaining care, fewer doctor visits, and more difficulty obtaining prescription drugs. Compared to whites, minority groups in the United States are less likely to have a doctor they go to on a regular basis and are more likely to use emergency rooms and clinics as their regular source of care. Lack of financial resources. Although the lack of financial resources is a barrier to health care access for many Americans, the impact on access appears to be greater for minority populations. (The Medical News, ND) Example Of A New Definition The health care financing system. The Institute of Medicine in the United States says fragmentation of the U.S. health care delivery and financing system is a barrier to accessing care. Racial and ethnic minorities are more likely to be enrolled in health insurance plans which place limits on covered services and offer a limited number of health care providers. Legal barriers. Access to medical care by low-income immigrant minorities can be hindered by legal barriers to public insurance programs. For example, in the United States federal law bars states from providing Medicaid coverage to immigrants who have been in the country fewer than five years. Structural barriers. These barriers include poor transportation, an inability to schedule appointments quickly or during convenient hours, and excessive time spent in the waiting room, all of which affect a person's ability and willingness to obtain needed care. (The Medical News, ND) Example Of A New Definition Scarcity of providers. In inner cities, rural areas, and communities with high concentrations of minority populations, access to medical care can be limited due to the scarcity of primary care practitioners, specialists, and diagnostic facilities. Linguistic barriers. Language differences restrict access to medical care for minorities in the United States who are not English-proficient. Health literacy. This is where patients have problems obtaining, processing, and understanding basic health information. For example, patients with a poor understanding of good health may not know when it is necessary to seek care for certain symptoms. While problems with health literacy are not limited to minority groups, the problem can be more pronounced in these groups than in whites due to socioeconomic and educational factors. (The Medical News, ND) Example Of A New Definition Lack of diversity in the health care workforce. A major reason for disparities in access to care are the cultural differences between predominantly white health care providers and minority patients. Only 4% of physicians in the United States are African American, and Hispanics represent just 5%, even though these percentages are much less than their groups' proportion of the United States population. Age. Age can also be a factor in health disparities for a number of reasons. As many older Americans exist on fixed incomes which may make paying for health care expenses difficult. Additionally, they may face other barriers such as impaired mobility or lack of transportation which make accessing health care services challenging for them physically. Also, they may not have the opportunity to access health information via the internet as less than 15% of Americans over the age of 65 have access to the internet. This could put older individuals at a disadvantage in terms of accessing valuable information about their health and how to protect it. (The Medical News, ND) Example Of A New Definition Within a community-context, the goal of eliminating health disparities and beyond, must be linked to the elimination of the over-representation of children and youth in all sectors (education, child welfare, health and mental health outcomes) in order to support the wellbeing of children and their families A class divided A class divided part I A class divided part II Unnatural Causes Wealth equals health How Racism Impacts Pregnancy Outcomes Unraveling the mystery of white and black differences in infant mortality (8:53) Arriving Healthy