Slides - Clinical Trial Results
advertisement

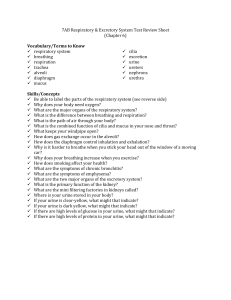
REMEDIAL II REnal Insufficiency Following Contrast MEDIA Administration II TriaL RenalGuard system in high risk patients for contrast induced acute kidney injury Carlo Briguori, MD, PhD Laboratoy of Interventional Cardiology Clinica Mediterranea, Naples - Italy Disclosure Statement of Financial Interest I, Carlo Briguori DO NOT have a financial interest/arrangement or affiliation with one or more organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation. Background Contrast-induced acute kidney injury (CI-AKI) is a powerful predictor of unfavorable early and late outcome1-3 Several studies showed the advantages of the prophylaxis by sodium bicarbonate solution 4-5 N-acetylcysteine (NAC) 6-7 However, in high risk patients the rate of CI-AKI is still high 1. McCullough PA. J Am Coll Cardiol 2008;51:1419-28 2. Solomon R. et al. Clin J Am Soc Nephrol 2009;4:1162-1169 3. Briguori C, et al. Circulation 2010;121:2117-2122. 4. Merten GJ et al. JAMA 2004;291:2328-2334 5. Briguori C, et al. Circulation 2007;115:1211-1217. 6. Tepel M et al. N Engl J Med 2000;343:180-184. 7. Trivedi H, et al. Am J Med 2009;122:874 e9-15 High risk patients Hypotension 5 IABP 5 Risk Score Risk of CIAKI Risk of Dialysis CHF 5 5 7.5% 0.04% Age > 75 years 4 Anemia 3 6 to 10 14% 0.12% Diabetes 3 11 to 16 26.1% 1.09% 16 57.3% 12.6% Contrast media volume Serum creatinine >1.5 mg/dl OR eGFR <60 mlmin1.73 m2 1 for each 100 cc3 4 2 for 40-60 4 for 20-60 6 for <20 Mehran R et al J Am Coll Cardiol 2004; 44:1393-9 Background Creating and maintaining a high urine output is beneficial to prevent kidney damage. This high urine flow rate, indeed, should allow the body to rapidly eliminate contrast, reducing its toxic effects. Data from the PRINCE study indicate that increasing the urine flow rate (≥150 ml/h) reduces the toxic effect of contrast media 1 A forced diuresis regime is usually achieved by high dose of furosemide which may be deleterious, potentially due to a negative fluid balance 2,3 1. Stevens MA et al. J Am Coll Cardiol 1999;33:403-411 2. Weinstein JM et al. Nephron 1992;62:413-415 3. Solomon R, et al. N Engl J Med 1994;331:1416-1420. Background The RenalGuardTM automated hydration matching system (PLC Medical System, Inc.) was developed in order to achieve precise real-time high volume fluid balance using a closed loop hydration monitoring and infusion system RenalGuard system Resnic F. et al. J Am Coll Cardiol 2009 53: A36 RenalGuard System RenalGuard System closed loop fluid management system high volume fluid pump high accuracy dual weight measuring system single use intravenous set; urine collection system that interfaces with a standard Foley catheter real-time display of urine and hydration fluid volume user set net fluid gain and fluid bolus administration for patients that require rehydration prior to and during the procedure automatic battery back-up automatic priming of infusion set timely alerts to drain urine bag or to replace the hydration fluid bag. Purpose We performed a prospective, randomized study comparing the prophylactic effectiveness of 2 different strategies for preventing CI-AKI: Sodium Bicarbonate plus N-Acetylcysteine (Control Group) Hydration with RenalGuard system (RenalGuard Group) REMEDIAL II • DESIGN: Prospective, randomized, double-arm, multicenters clinical study Elective contrast media administration in patients at high risk for CI-AKI (risk score ≥11 and/or eGFR≤30 ml/min/1.73 m2) RenalGuard group Control group CI-AKI (sCr ≥0.3 mg/dL at 48 h) Sample size • Hypothesis: — Reduction in the primary endpoint from 25% in the Control group to 10% in the RenalGuard group • Sample size: – A total of 266 patients (133 each group) will be necessary to gave the study 90% power and a significance level <0.05 Inclusion criteria Age 18 y Chronic kidney disease High risk for CI-AKI: eGFR ≤30 ml/min/1.73 m2 and/or Mehran score ≥ 11 Exclusion criteria • Primary or rescue PCI Pregnancy Recent (≤ 7 days) contrast media exposure Chronic dialysis and/or history or previous dialysis multiple myeloma pulmonary edema acute myocardial infarction Administration of theophylline, dopamine, mannitol, or fenoldopam or sodium bicarbonate. REMEDIAL II trial Sodium Bicardonate & Acetylcysteine Hydration by sodium bicarbonate (3 ml/Kg i.v. 1 h before and 1 ml/kg for 6 h after) & NAC 1200 mg BID x 2 & 1.5 g e.v. during the procedure RenalGuard group Hydration with normal saline (urine flow ≥ 300 ml/h) & NAC (1.5 g/L) & limited (0.25 mg/kg) furosemide dose RenalGuard group Pre-procedure Procedure Post- procedure Biomarkers: sCr = baseline, 2, 6, 12, 24 and 48 hours sCyC = baseline, 2, 6, 12, 24 and 48 hours NGAL = baseline, 2, 6, 12, 24 and 48 hours Furosemide (0.25 mg/kg) 500 300 200 RenalGuard system Prime (≤250 mL) 400 Foley Catheter Urine flow rate (ml/h) 600 Continuous real-time matched replacement fluid 100 0 0 30 60 90 Patient ready for procedure when urine flow rate is ≥300 ml/h 120 150 180 210 240 270 Time (minutes) 300 330 360 400 RenalGuard System Endpoints • Primary endpoint: – Rate of CI-AKI, defined as a serum creatinine (sCr) increase 0.3 mg/dLat 48 hours • Secondary endpoints: – an increase in the sCr concentration 25% and 0.5 mg/dl at 48 hours after contrast exposure – changes in the serum cystatin C (sCyC) concentration at 24 and 48 hours after contrast exposure – the rate of acute renal failure requiring dialysis – the rate of in-hospital, and 1 month major adverse events (MAE), including a) death, b) renal failure requiring dialysis, and c) acute pulmonary edema – changes in the serum and urine NGAL concentrations at 2, 6, 12, 24 and 48 hours after contrast exposure Enrollement Assessed for eligibility ( n= 806) Exclusion (n = 512) Not meeting inclusion/exclusion criteria (n = 485 ) Refused to partecipate (n = 27) Allocation Patients allocated in the Control group (n = 147) Received allocated treatment (n = 146) Did not receive the allocated treatment (n= 1) Patients lost at follow-up (n = 0) Discontinued treatment (n = 2) Patients lost at follow-up (n = 0) Discontinued treatement (n = 0) Patients analized ( n = 146) Patients excluded from analysis (n = 0) Patients analized ( n = 146) Patients excluded from analysis (n = 0) Analysis Patients allocated in the RenalGuard group (n = 147) Received allocated treatment (n = 146) Did not receive the allocated treatment (n =1) Follow-up Randomized (n = 294) Clinical Characteristics Age, yrs (mean SD) Male, % BMI (kg/m2) Blood pressure (mm Hg) Systolic Diastolic Mean LVEF, % (mean SD) LVEDP (mm Hg) Diabetes mellitus Hypertension, % Drugs: ACE inhibitor Calcium channel blocker Angiotensin II receptor inhibitor Diuretics blocker Statins Control Group (N=146) RenalGuard Group (N=146) P 75 9 76 8 0.31 103 (70.5%) 88 (60.5%) 0.065 29 5 28 5 0.16 152±27 78±10 103±13 48 10 14±7 104 (71%) 144 (98%) 152±27 77±13 102±15 46 11 14±7 101 (69%) 143 (98%) 0.99 0.76 0.85 0.10 0.81 0.51 0.95 67 (46%) 44 (30%) 45 (31%) 85 (58%) 88 (60%) 111 (76%) 70 (48%) 36 (25%) 42 (29%) 93 (64%) 92 (63%) 108 (74%) 0.77 0.37 0.77 0.36 0.66 0.73 Biochemical Characteristics eGFR (ml/min/1.73 m2) GFR ≤ 30 Serum Urea Nitrogen (mg/dL) Baseline after 48 h Control Group (N=146) 32 7 62 (44%) RenalGuard Group (N=146) 32 9 69 (48.5%) 0.83 0.41 78 31 70 ± 30 80 35 71±35 0.57 0.84 140 5 139± 6 140 3 140 ± 5 0.37 0.87 4.7 0.7 4.3 ± 0.6 4.6 0.7 4.2 ± 0.6 0.55 0.17 P Serum Sodium (mEq(L) Baseline after 48 h Serum Potassium (mEq/L) Baseline after 48 h Procedural Characteristics Control Group (N=146) Performed procedure coronary angiography PCI coronary angiography & PCI peripheral procedure Volume of contrast media (ml) Contrast ratio >1 RenalGuard Group (N=146) P 0.36 60 (41%) 58 (40%) 17 (11%) 11 (6%) 51 (35%) 71 (49%) 11 (7.5%) 13 (9%) 145 79 35 (24%) 135 76 28 (19%) 0.29 0.32 Distribution of the Risk score 120 Number of patients 100 72.5% 80 60 40 20 2% 13% ≥5 ≥6-10 12.5% 0 ≥11-15 Risk score ≥16 Urine Volume at 24 hours 3000 p <0.001 2500 2000 1500 1000 500 0 Control Group RenalGuard group RenalGuard group Pre-procedure Procedure 7 h & 54 minutes (4.7-11.5 h) 400 Foley Catheter 300 200 Furosemide (14±8mg; range = 0-50) 500 RenalGuard system Prime (223±45 mL; range = 50-300) 600 Urine flow rate (ml/h) Post- procedure 100 Biomarkers: sCr = baseline, 2, 6, 12, 24 and 48 hours sCyC = baseline, 2, 6, 12, 24 and 48 hours NGAL = baseline, 2, 6, 12, 24 and 48 hours Continuous real-time matched replacement fluid 0 0 30 60 90 Time to reach Target urine flow rate 58±19 min (30-120) 120 150 180 210 240 270 Time (minutes) 300 330 360 400 RenalGuard Group 4000 Volume (ml) 3500 3000 2500 infusion 2000 1500 urine 1000 500 0 15 45 75 105 135 165 195 225 255 285 315 345 375 Time (minutes) RenalGuard Group 900 Mean urine flow rate: 352±131 ml/h Urine flow rate (ml/h) 800 700 600 Target reached in 93% of patients (416±19 ml/h) 500 400 300 Below the target in 7% of patients (117±48 ml/h) 200 100 0 15 45 75 105 135 165 195 225 Time (minutes) 255 285 315 345 375 sCr kinetic serum creatinine (median) 2.4 2.2 2.0 1.8 1.6 1.4 1.2 Control group p = 0.008; F = 4.97 RenalGuard group 1.0 Baseline 24 Time (hours) 48 Primary endpoint 25 Odds ratio = 0.47; 95% CI= 0.24-0.92 p = 0.025 20.5% 20 CI-AKI (%) 30/146 15 11% 10 16/146 5 0 Control group RenalGuard group Secondary endpoints Control group (n= 146) RenalGuard group (n= 146) P 30 (20.7%) 22 (15%) 19 (13%) 11 (7.5%) 16 (11%) 9 (6%) 4 (2.7%) 1 (0.7%) 0.025 0.003 0.001 0.003 21 (15.5%) 33 (24%) 23 (17%) 14 (10%) 11 (8.5%) 22 (16%) 17 (12%) 5 (3.5%) 0.07 0.13 0.29 0.04 29 (21%) 47 (34%) 35 (25.5%) 23 (17%) 16 (12%) 29 (22%) 21 (16%) 11 (8.5%) 0.045 0.027 0.050 0.039 Changes in creatinine at 48 hours Increase ≥0.3 mg/dL Increase ≥0.5 mg/dL Increase ≥25% Increase ≥50% Changes in cystatin C at 24 hours* Increase ≥0.3 mg/dL Increase ≥10% Increase ≥15% Increase ≥25% Changes in cystatin C a 48 hours* Increase ≥0.3 mg/dL Increase ≥10% Increase ≥15% Increase ≥25% sCyC kinetic 2.4 serum cystatin C (median) 2.2 2.0 1.8 1.6 1.4 1.2 Control group p = 0.004; F = 5.52 RenalGuard group 1.0 Baseline 24 Time (hours) 48 Secondary endpoint Events rate at 1-month p = 0.52 10 9 8 7 6 % 5 4 3 2 1 0 9.6 6.8 p = 0.031 p = 1.0 4.8 4.1 4.1 p = 0.62 2.1 0.7 Dialysis 0.7 Pulmonary Edema Control Group Death Cumulative RenalGuard Group Conclusions The RenalGuard therapy, including hydration with normal saline plus high dose of NAC controlled by the RenalGuard system in combination with limited (0.25 mg/kg) dose of furosemide, is an effective renoprotective strategy for patients at high- risk for CIAKI. REMEDIAL II Investigators • Clinica Mediterranea, Naples – – – – C. Briguori (P.I.) A. Focaccio G. Visconti B. Golia • Multimedica IRCCS, Milan – – – – F. Airoldi D. Tavano S. Di Biase S. Bertoli • University of Ferrara, Ferrara – M. Valgimigli – R. Ferrari • University of Modena, Modena – G.M. Sangiorgi – M. G. Modena