Cardiology Review
advertisement

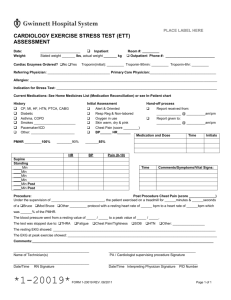
Cardiology Review 6/3/2009 A 28 yom is evaluated for palpitations. He reports a 5 year history of palpitations. These episodes used to occur once or twice a year, but over the past 6 months, he has been experiencing them on a monthly basis. He reports that his heart starts racing suddenly for no reason, and the episode usually terminates abruptly after he takes a few deep breaths. Episodes typically last 10 to 15 minutes, although one episode last month lasted 30 minutes. He is otherwise healthy, denies other symptoms, and takes no medications. Results of his physical examination are within normal limits. A baseline EKG is obtained and shown. The ECHO demonstrated a subtle anterior wall motion abnormality but is otherwise WNL. A 24 hr holter demonstrates a narrow complex regular tachycardia with rate of 205 during an episode of palpitations. What is the next step? RF ablation metoprolol stress test verapamil WPW A 28 yom is evaluated for palpitations. He reports a 5 year history of palpitations. These episodes used to occur once or twice a year, but over the past 6 months, he has been experiencing them on a monthly basis. He reports that his heart starts racing suddenly for no reason, and the episode usually terminates abruptly after he takes a few deep breaths. Episodes typically last 10 to 15 minutes, although one episode last month lasted 30 minnutes. He is otherwise healthy, denies other symptoms, and takes no medications. Tesults of his physical examination are within normal limits. A baseline EKG is obtained and shown. The EKG demonstrated a subtle anterior wall motion abnormality but is otherwise WNL. A 24 hr holter demonstrates a narrow complex regular tachycardia with rate of 205 during an episode of palpitations. What is the next step? RF ablation metoprolol stress test verapamil WPW Short PR interval +delta wave +h/o tachycardia = WPW Two circuits: 1. 2. AV node retrograde accessory pathway QRS in narrow since there is conduction via AV node The WMA is a result of abnormal depolarization via the accessory pathway. RF ablation is first line Avoid metoprolol, CCB, and adenosine; they blocks the AV node but not the accessory. Use Procainamide A 45 yof is evaluated in the emergency department for palpitations. She has no history of CV disease but does have a h/o intermittent palpitations. This is her first prolonged episode, and cough and strain maneuvers that she has used in the past to terminate the episodes have been ineffective this time. PE is unremarkable with the exception of tachycardia. The BP is 110/70. EKG shown. What is the diagnosis: AV nodal reentrant tachycardia AV reentrant tachycardia ectopic atrial tachycardia multifocal atrial tachycardia a flutter A 45 yof is evaluated in the emergency department for palpitations. She has no history of CV disease but does have a h/o intermittent palpitations. This is her first prolonged episdoe, and the cough and strain maneuvers that she has used in the past to terminate the episodes have been ineffective this time. PE is unremarkable with the exception of tachycardia. The BP is 110/70. EKG shown. What is the diagnosis: AV nodal reentrant tachycardia AV reentrant tachycardia ectopic atrial tachycardia multifocal atrial tachycardia a flutter AVNRT Narrow No P waves; buried in the QRS complex Usual Tx complex tachycardia rate 160-180 with IV adenosine Compare to: AVRT- P waves are visible MAT- irregular with 3 P wave morphologies. AV Nodal Block 1st degree: 2nd degree: prolonged PR Look for drug effect (dig, beta blocker, CCB) Mobitz I: PR progressively lengthens, then a dropped beat Mobitz II: Intermittent non-conducted beats 3rd degree: complete dissociation PM: asymptomatic Mobitz II and complete block. Torsades Atypical Vtach Look for hypoK or hypoMg Worse prognosis than V tach Management is different from other VTs Avoid Class I, Ic or III antiarrhythmics (prolong QT) Give Magnesium acutely Things that cause torsades: arsenic, ciapride, droperidol, Li, methadone, fluoroquinolones A 79 yof is seen for an annual examination. She is in good health except for osteopenia, for which she takes Ca and VitD supplements. She walks regularly to and from the bus stop several times per week. It now takes her 25 min to get to the bus stop; whereas it only took her 10 min a year ago. She describes dyspnea midway in her walk, causing her to stop and catch her breath. She denies angina, presyncope, syncope or pedal edema. PE: HR 80, BP 165/86. Lungs CTAB, carotid upstrokes delayed. S1 nl, single S2, and S4. Grade 3/6 late peaking systolic murmur at R 2nd intercostal, radiates to R carotid. TTE with concentric LVH. EF 69%, no WMA. Trileaflet AV with heavy calcification, aortic jet 4.8/ m/sec, peak transaortic gradient of 92, valve area of 0.7 cm2. What will improve her quality of life? Begin ACEI Percutaneous aortic balloon valvuloplasty AVR Cardiac rehab Stop Calcium supplement AS A 79 yof is seen for an annual examination. She is in good health except for osteopenia, for which she takes Ca and VitD supplements. She walks regularly to and from the bus stop several times per week. It takes her 25 mimn to get to the bus stop whereas it only took her 10 min a year ago. She describes dyspnea midway in her walk, causing her to stop and catch her breath. She denies angina, presyncope, syncope or pedal edema. PE: HR 80, BP 165/86. Lungs CTAB, carotid upstrokes delayed. S1 nl, single S2, and S4. Grade 3/6 late peaking systolic murmur at R 2nd intercostal, radiates to R carotid. TTE with concentric LVH. EF 69%, no WMA. Trileaflet AV with heavy calcification, aortic jet 4.8/ m/sec, peak transaortic gradient of 92, valve area of 0.7 cm2. What will improve quality of life? Begin ACEI Percutaneous aortic balloon valvuloplasty AVR Cardiac rehab Stop Calcium supplement Aortic Stenosis Severe AS: valve area below 0.8 Most common cause: progressive valvular Ca Initial compensatory mechanism is myocardial hypertrophy Indication onset of cardiac symptoms NOT prophylactically Triad for AVR: of symptoms: Angina CHF Syncope ACEIs contraindicated: afterload reduction may increase effective pressure gradient across stenotic valve. Murmurs Sounds Maneuvers Other Mitral Stenosis Mitral Regurg Opening snap following S2 on LSB or apex. Middiastolic rumble. Loudest after exercise. RAD, negative biphasic P in V1 Aortic stenosis Harsh, crescendo/decrescendo, at R 2nd intercostal Paradoxical splitting of S2, radiates to carotids with slow upstoke, louder with squatting or expiration. LVH Aortic regurg Faint, blowing between S2 and S1, diastolic, at LSB 3/4th intercostal Wide pulse pressure, prominent carotid pulses. LVH VSD Holosystolic at LLSB Louder with handgrip ASD Fixed split S2 Primum: LAD, RBBB Secundum: RAD, RBBB Holosystolic, blowing, over PMI, radiates to L axilla LAD, LVH, Primum needs Abx prophy Primum may have AV block 42 yof with recent onset of exertional dyspnea and occasional palpitations. She has been told for many years that she has a heart murmur. PE: BP 129/78 in both upper extremities, JVP elevated with both a and v waves. Apical pulse unremarkable. Parasternal impulse present. 2/6 midsystolic murmur noted at 2nd L intercostal and 2/6 holosystolic murmur at the apex and L sternal border. Fixes splitting of S2. Which is the most likely cause of the symptoms? secundum atrial septal defect primum atrial septal defect PFO sinus venosus atrial septal defect ASD 42 yof with recent onset of exertional dyspnea and occasional palpitations. She has been told for many years that she has a heart murmur. PE: BP 1269/78 in both upper extremities, JVP elevated with both a and v waves. Apical pulse unremarkable. Parasternal impulse present. 2/6 midsystilic murmur noted at 2nd L intercostal and 2/6 holosystolic murmur at the apex and L sternal border. Fixes splitting of S2. Which is the most likely cause of the symptoms? secundum atrial septal defect primum atrial septal defect PFO sinus venosus atrial septal defect ASD Fixed splitting of S2: hallmark of ASD Exam: Parasternal impulse: R sided cardiac enlargement (also seen on CXR) Systolic murmur at the apex: mitral regurg L sternal border: TVR midsystolic murmur: flow across the pulmonary valve. EKG PE shows first degree AV vlock and LAD= primum for PFO is normal Why does this matter: Secundum and PFO can be treated with percutaneous devices. 69 yom is evaluated in the ED for acute onset of substernal CP radiating to the L arm. Former smoker and PMH of HTN. PE 210/95 R arm, 164/56 L arm, HR 90, RR 20, dullness half way up the R posterior thorax, 2/6 diastolic murmur at RUSB, EKG with NSR, 2-3 mm inferior ST segment elevation. What is the most appropriate med to administer? ASA IV heparin Thrombolytic Beta blocker ACEI Dissection 69 yom is evaluated in the ED for acute onset of substernal CP radiating to the L arm. Former smoker and PMH of HTN. PE 210/95 R arm, 164/56 L arm, HR 90, RR 20, dullness half way up the R posterior thorax, 2/6 diastolic murmur at RUSB, EKG with NSR, 2-3 mm inferior ST segment elevation. What is the most appropriate med to administer? ASA IV heparin Thrombolytic Beta Blocker ACEI Aortic Dissection Disparate blood pressures + diastolic murmur of AR = acute ascending aortic dissection (involves the AV) Dullness RCA in R lung = hemothorax (complication of dissection) is the most common involved coronary with dissection, ischemia (STEMI). Initial Treatment beta blockade (decrease shear stress) Start BB before afterload reduction. Avoid: ASA, heparin, thrombolytics Increased risk of: periaortic hemorrhage, aortic rupture, and cardiac tamponade Studies: TEE, chest CT with contrast, contrasted MR. A 68 yom is evaluated in the ED for chest pain that has lasted 90 min. He was eating when he developed sudden onset of sharp precordial pain radiating toward both shoulders and back. The pain is 9/10. PMH for HTN and dyslipidemia. PE: HR 90, RR 19 BP 110/60, O2 sat 94% on RA. Lungs: bibasilar crackles. Heart sounds distant, nl S1, S2, no S4 or S3. 3/6 diastolic murmur at the RUSB, radiates across L precordium. No abdominal bruits. Trace pedal edema. P CXR with prominent thoracic aorta and widening of the mediastinum. Next step? cath fibrinolytic therapy VQ scan CT chest balloon pump Aortic dissection with AR A 68 yom is evaluated in the ED for chest pain that has lasted 90 min. He was eating when he developed sudden onset of sharp precordial pain radiating toward both shoulders and back. The pain is 9/10. PMH for HTN and dyslipidemia. PE: HR 90, RR 19 BP 110/60, O2 sat 94% on RA. Lungs: bibasilar crackles. Heart sounds distant, nl S1, S2, no S4 or S3. 3/6 diastolic murmur at the RUSB, radiates across L precordium. No abdominal bruits. Trace pedal edema. P CXR with prominent thoracic aorta and widening of the mediastinum. Next step? cath fibrinolytic therapy VQ scan CT chest balloon pump – This would exacerbate the acute AR Ascending Dissection with Acute AR Aortic Risk Regurg: Diastolic murmur Factors: age HTN bicuspid aortic valve Coarctations 3rd trimester pregnancy and Marfans) Possible imaging include: CT chest with contrast MRI with contrast TEE Complications: MI from anterograde propogation, Tamponade limb ischemia (if great vessels involved) aortic rupture Ascending vs Descending Ascending dissections are high risk for complications. Do not pass go, instead… go directly to surgery. Descending dissections treat medically (Beta Blockers and nitroprusside-if needed), and if pain persists, it is due to extension of dissection, then go to surgery. Even with repair mortality is 26%, without 55% AAA Screen all men with smoking hx after age 65 (medicare pays for this) AAA, DM are both CAD equivalents Surgery Men >5 cm Women >4.5 Marfans >4.5 expands more than 0.5/year 64 yof presents 6 hrs after onset of severe crushing chest pain associated with diaphoresis, n/v. She has a h/o mild hyperlipidemia, meds include atorvastatin and ASA. BP 140/88, HR 88, lungs clear, no murmurs, abd and extremities normal. EKG 3 mm ST elevation in leads II, III, and aVF, occasional PVCs. No cath lab facilities are present, fibrinolytics are given and transferred to ICU. CP resolves. 2 episodes of 6-10 beats of Vtach noted with stable hemodynamics. EKG now shows <0.5 mV ST segment elevation. In addition to heparin ans ASA, which is the next appropriate step? Cath Plavix Beta blocker amiodarone DSE 64 yow presents 6 hrs after onset of severe crushing chest pain associated with diaphoresis, n/v. She has a h/o mild hyperlipidemia, meds in clude atorvastatin and ASA. BP 140/88, HR 88, lungs clear, no murmurs, abd and extremities normal. EKG 3 mm ST elevation in leads II, III, and aVF, occasional PVCs. No cath lab facilities are present, fibrinolytics are given and transferred to ICU. CP resolves. 2 episodes of 6-10 beats of Vtaqch noted with stable hemodynamics. EKG now shows <0.5 mV ST segment elevation. In addition to heparin ans ASA, which is the next appropriate step? Cath Plavix Beta blocker amiodarone DSE Inferior STEMI Medical management After MI: ASA beta blockers ACEI Statin Reperfusion arrhythmias usu do not require additional antiarrhythmic therapy. Immediate cath after STEMI for: recurrent ischemia persistent ST elevation hemodynamic instability CHF ACS Treatment for the Boards ASA Plavix (with, or prior to, PCI- CURE trial), Lovenox (more effective than heparin) beta blocker ACEI IIbIIIa for PCI but NOT without PCI Statin smoking cessation. 78 yom brought to the ED for malaise, fatigue and mild dyspnea on exertion. Intermittent CP for 5 days, with the most severe episode 2 days ago. Pain free since then. PMH: HTN, DM type 2, meds: ACEI and metformin. BP 112/82, HR 92, JVP is 5 mmHg, no carotid bruits, lungs clear. CV nl S1/S2, 2/6 holosystoloic murmur at apex to axilla, diminished leg pulses, no edema. EKG with sinus tach, Q waves in V1-4. Renal fn and Hct are normal. CK 120, Troponin 6.8. CXR with mild pulmonary edema. Pt is started on lovenox and ASA. Next appropriate therapeutic approach is? plavix glycoprotein receptor blocker fibrinolysis urgent cath beta blocker Anterior STEMI 78 yom brought to the ED for malaise, fatigue and mild dyspnea on exertion. Intermittent Cp for 5 days, most severe episode 2 days ago. Pain free since then. PMH: HTN, DM type 2, meds: ACEI and metformin. BP 112/82, HR 92, JVP is 5 mmHg, no carotid bruits, lungs clear. CV nl S1/S2, 2/6 holosystoloic murmur at apex to axilla, diminished leg pulses, no edema. EKG with sinus tach, Q waves in V1-4. Renal fn and Hct are normal. CK 120, Troponin 6.8. CXR with mild pulmonary edema. Pt is started on lovenox and ASA. Next appropriate therapeutic approach is? plavix glycoprotein receptor blocker fibrinolysis urgent cath beta blocker Anterior STEMI Beta Blockers are always a good answer. Unless signs of persistent ischemia, cath is not urgently indicated. Late fibrinolysis not beneficial, and increases risk of hemorrhage in the infarcted zone. No benefit of plavix added to ASA if there are no plans on PCI IIbIIIa is indicated for patients who are going to cath/PCI, if there are high risk factors such as: TIMI>3 elevated troponin ongoing ischemia new ST changes CHF or DM hemodynamic instability PCI within the past 6 months 42 yom evaluated in Halifax Regional for L shoulder chest pain that radiates to the jaw, associated with diaphoresis and mild dyspnea. No PMH, no meds. FH of CAD in first degree relatives. ED administered IV heparin, atenolol, ASA. BP 100/79, HR 61, no JVD, no carotid bruits, lungs clear, nl S1/S2, no murmurs. Abd and extremities wnl. No cath lab at the OSH, UNC is 62 miles away, and will take 2 hours. Before transfer you should give….. 2b3a receptor blocker plavix esmolol fibrinolytic therapy NTG STEMI with no Cath Lab 42 yom evaluated in rural ED for L shoulder chest pain that radiates to the jaw, associated with diaphoresis and mild dyspnea. No PMH, no meds. FH of CAD in first degree relatives. ED administered IV heparin, atenolol, ASA. BP 100/79, HR 61, no JVD, no carotid bruits, lungs clear, nl S1/S2, no murmurs. Abd and extremities wnl. No cath lab at the OSH, UNC is 62 miles away, and will take 2 hours. Before transfer you should give….. 2b3a receptor blocker plavix esmolol fibrinolytic therapy NTG STEMI and Fibrinolytics The best answer is always CATH Second best is FIBRINOLYSIS Fibrinolysis Given within 30 minutes of arrival to ED DO NOT give if >12 hours after onset of symptoms and asymptomatic (this pt is less than 12 hours) Contraindications: recent surgery CVA Bleeding uncontrolled HTN PUD cardiogenic shock 68 yom seen 14 hrs after onset of substernal CP that lasted for 2 hrs. 6 hrs prior to presentation he experienced 2 additional shorter episodes of CP, each 10 min in duration. CP associated with diaphoresis, no dyspnea, palpitations, or dizziness. H/o HTN, DM, active smoker 40 pack year hx. Home meds: ASA, norvasc, metoprolol and glyburide. PE: normotensive, NAD, enlarged PMI. CK and troponins elevated, EKG with small R waves in V1-3, unchanged by day 3 of hospitalization. ECHO with severe hypokinetic LV anterior wall, moderate hypokinesis of the inferior wall and LVEF 38%. Current meds: metoprolol, asa, NTG, plavix, lipitor, lisinopril, heparin. What is the most appropriate evaluation prior to discharge? 24 hr EKG low level treadmill stress test dobutamine viability study cath 68 yom seen 14 hrs after onset of substernal CP that lasted for 2 hrs. 6 hrs prior to presentation he experienced 2 additional shorter episodes of CP, each 10 min in duration. CP associated with diaphoresis, no dyspnea, palpitations, or dizziness. H/o HTN, DM, active smoker 40 pack year hx. Home meds: ASA, norvasc, metoprolol and glyburide. PE: normotensive, NAD, enlarged PMI. CK and troponins elevated, EKG with small R waves in V1-3, unchanged by day 3 of hospitalization. ECHO with severe hypokinetic LV anterior wall, moderate hypokinesis of the inferior wall and LVEF 38%. Current meds: metoprolol, asa, NTG, plavix, lipitor, lisinopril, heparin. What is the most appropriate evaluation prior to discharge? 24 hr EKG low level treadmill stress test dobutamine viability study cath >12 Hours out from an Anterior MI Patient did not get revascularization or thrombolytics. By ECHO pt has decreased EF and 2 areas of WMA with TIMI 5 High risk factors for complications after MI: Multivessel CAD anterior MI EF <40% CHF recurrent ischemia Never subject a high risk pt to stress testing even if submaximal stress. Post-MI complications 1. Recurrent ischemia: 1/3 of patients, and more common in NSTEMI rather than STEMI. 2. Arrhythmias: bradycardia, SVT/atrial fibrillation, ventricular arrhythmias (mostly in the first few hours), AV block, 3. CHF 4. Myocardial rupture: rupture of the LV, 1% of pts, 2-7 days (pseudoaneurysm- rupture sealed by pericardium) 5. LV aneursym: from scar, predisposed to CHF, thrombus, and arrhythmias 6. Papillary muscle rupture: posteromedial papillary muscle is more common b/c single blood supply from RCA. Classic case: inferior MI, later becomes hypotensive, large V waves in PA wedge tracing, new holosytolic murmur at the apex. 7. Mural thrombi (in anterior and apical STEMI) 8. pericarditis 45 yom brought by EMS for severe CP. Pain similar to prior episode when he underwent angioplasty 8 m ago. H/O HTN, on beta blocker, also takes ASA 81 mg q day. Nl serum CH and no h/o DM, DOE or claudication. PE: BP 90/60, HR 59, no JVD, no bruits, lungs clear, Nl S1, S2. S4 present with 1/6 SEM at LSB, nonradiating. Abd and extremities nl. EKG with ST depression in II, III, and aVF. Admitted and placed on plavix, nitrates, and lovenox. Troponin 0.8 (nl <0.5). What is the next appropriate step? Heparin esmolol abciximab NTG USA 45 yom brought by EMS for severe CP. Pain similar to prior episode when he underwent angioplasty 8 m ago. H/O HTN, on beta blocker, also takes ASA 81 mg q day. Nl serum CH and no h/o DM, DOE or claudication. PE: BP 90/60, HR 59, no JVD, no bruits, lungs clear, Nl S1, S2. S4 present with 1/6 SEM at LSB, nonradiating. Abd and extremities nl. EKG with ST depression in II, III, and aVF. Admitted and placed on plavix, nitrates, and lovenox. Troponin 0.8 (nl <0.5). What is the next appropriate step? Heparin esmolol abciximab NTG USA and NSTEMI IIbIIIa: beneficial with pts going to PCI associated with increased mortality for those not going to PCI Who should get it: TIMI >3 recurrent angina elevated troponin new ST depressions prior CABG percutaneous intervention within 6 months VTach hemodynamic instability Plavix is also indicated, but usually held if going to cath in case CABG needed. 49 yom presents to the ED with mild chest discomfort, with nausea and dyspnea for 2 hours. No relief with antacids. No PMH, no meds. Older brother with an MI 9 months earlier, father with CABG 12 years ago. BP 109/78, HR 88, no jvd, no carotid bruits, nl S1/S2, no m/r/g, lungs, abd, extremities wnl. Troponin of 6. EKG with 1mV ST elevation in II, III and aVF. Started on lovenox, asa, metoprolol, and IIbIIIa, and sent to cath. DES placed in subtotally occluded RCA. ECHO on d#2 shows nl LV, no MR, no effusion. D#4 no complications, and plan on d/c. In addition to ASA, plavix, and metoprolol what should be given? Lipitor lisinopril warfarin niacin 49 yom presents to the ED with mild chest discomfort, with nausea and dyspnea for 2 hours. No relief with antacids. No PMH, no meds. Older brother with an MI 9 months earlier, father with CABG 12 years ago. BP 109/78, HR 88, no jvd, no carotid bruits, nl S1/S2, no m/r/g, lungs, abd, extremities wnl. Troponin of 6. EKG with 1mV ST elevation in II, III and aVF. Started on lovenox, asa, metoprolol, and IIbIIIa, and sent to cath. DES placed in subtotally occluded RCA. ECHO on d#2 shows nl LV, no MR, no effusion. D#4 no complications, and plan on d/c. In addition to ASA, plavix, and metoprolol what should be given? Lipitor lisinopril warfarin niacin Statins are given regardless of cholesterol level after MI because they reduce late CV events. PROVE-IT TIMI 22: showed high dose atorvastatin 80 was superior to pravastatin 40 with a 16% reduction of a composite endpoint. Dyslipidemia Develop more side effects on statins when you are concurrently on fibrates or niacin. Goals: ATP III-R 2005 RF: tobacco, HTN, Family history, AGE (men>45, women >55) LDL goal NonHDL goal CAD or <70 equivele nt (DM) <130 2+ RF <100 <160 0-1 RF <130 <190 23 yof is brought to the ED after a witnessed syncopal event. The patient reports having been at church where she DFO, after standing for 45 minutes. She noted feeling sweaty and lightheaded and seeing spots. She was aware of the sensation of her heart beating and then developed LOC. After the fall, witnessed said she had a thready pulse and urinary incontinence. She regained consciousness within 3 minutes. Which of the following aspects of the hx is not consistent with neurocardiogenic syncope? Urinary incontinence Prodrome of seeing spots, diaphoresis and lightheadedness Thready pulse None of the above 23 yof is brought to the ED after a witnessed syncopal event. The patient reports having been at church where she DFO, after standing for 45 minutes. She noted feeling sweaty and lightheaded and seeing spots. She was aware of the sensation of her heart beating and then developed LOC. After the fall, witnessed said she had a thready pulse and urinary incontinence. She regained consciousness within 3 minutes. Which of the following aspects of the hx is not consistent with neurocardiogenic syncope? Urinary incontinence Prodrome of seeing spots, diaphoresis and lightheadedness Thready pulse None of the above Neurocardiogenic syncope vasovagal and vasodepressor: Lose of sympathetic tone with vasodilation. with vasovagal there is bradycardia (due to increased vagal tone) Look for situational stressors: hot, crowded spaces, stressful environment, long period of standing, hunger, pain. Prodrome: light-headedness Diaphoresis Nausea Weakness visual changes pallor Incontinence suggests seizure Cardiogenic syncope Arrhythmia: Bradyarrhythmia, ventricular arrhythmia or V fib, AV node block Mechanical: Aortic valve (AS) or HOCM Absence of premonitory symptoms, usually exertional Quick recovery Orthostatic syncope 1st- Dehydration 2nd- polypharmacy AV nodal blockade (BB, CCB) Anticholinergics 3rd- autonomic insufficiency- DM HTN-JNC7 Treatment of HTN benefits are greater in the older patients compared to young patients. Reduces CVA, CHF and CV events, but not overall mortality Isolated systolic HTN is still high risk, even in the elderly, and should be treated. Wide pulse pressure is a risk factor for CHF. All patients: weight loss stop EtOH, limit Na, exercise HTN-JNC 7 1. 2. 3. 4. 5. 6. Stage 1: 140-159/90-99 Stage II: >160/100 Goal: treat to < 140/90 or <130/80 if DM Always start with a thiazide unless Post MI or CKD The number one reason for failure to control hypertension despite multiple agents is the failure to use a thiazide diuretic. CHF: thiazide, BB, ACEI, ARB, spironolactone POST MI: BB, ACEI, spironolactone DM: thiazide, BB< ACEI, ARB, CCB CKD: ACEI, ARB Recurrent CVA: thiazide, ACEI High CVD risk: thiazide, BB, ACEI, CCB